Introduction to Corneal Mucous Plaques
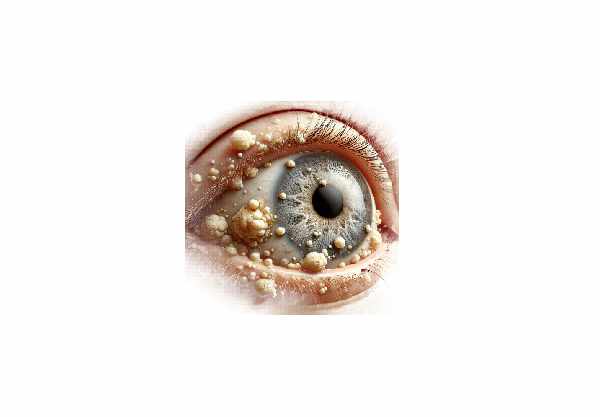
Corneal mucous plaques are a rare but significant ocular condition in which mucoid material accumulates on the corneal surface. These plaques are made up of mucus, inflammatory cells, and other debris that adhere to the cornea, causing a variety of symptoms and complications. Patients with corneal mucous plaques frequently report visual disturbances, discomfort, and a foreign body sensation in their affected eye. This condition can have a variety of underlying causes, including chronic inflammatory diseases, dry eye syndrome, and certain infections. Understanding the nature, causes, and implications of corneal mucous plaques is critical for proper diagnosis and treatment.
Corneal Mucous Plaques Detailed Examination
Corneal mucous plaques are abnormal accumulations of mucous and cellular debris on the corneal surface, which are frequently caused by a tear film or corneal epithelial barrier disruption. These plaques can range in size and density, from small, discrete deposits to large, confluent lesions that cover a large area of the cornea. The presence of these plaques can significantly impair vision and cause discomfort, so timely intervention is critical.
Causes and Risk Factors
- Chronic Inflammatory Diseases: Conditions like keratoconjunctivitis sicca (dry eye syndrome), Sjögren’s syndrome, and rheumatoid arthritis are frequently linked to the formation of corneal mucus plaques. Chronic inflammation disrupts the normal tear film and epithelial integrity, resulting in the accumulation of mucoid material.
- Ocular Surface Disorders: Conditions such as ocular rosacea, Stevens-Johnson syndrome, and chronic blepharitis can all contribute to the formation of mucous plaques by causing chronic inflammation and damage to the ocular surface.
- Infections: Bacterial, viral, and fungal infections can cause excessive mucus production and inflammation. Herpes simplex keratitis, for example, is known to cause corneal mucous plaques as a result of the inflammatory response it induces.
- Contact Lens Wear: Prolonged or improper use of contact lenses can disrupt the corneal epithelium and tear film, allowing mucous plaques to build up. Inadequate lens hygiene and overwearing lenses can aggravate the condition.
- Ocular Trauma and Surgery: Trauma to the cornea, as well as surgical procedures such as corneal transplants and LASIK, can disrupt the normal corneal surface, causing mucous plaques to form during healing.
Pathophysiology
The formation of corneal mucous plaques is a result of a complex interaction between tear film abnormalities, epithelial cell dysfunction, and chronic inflammation. The following mechanisms help to form these plaques:
- Tear Film Instability: A stable tear film is essential for maintaining a healthy cornea. In conditions such as dry eye syndrome, decreased tear production or increased tear evaporation cause tear film instability, allowing mucus and debris to accumulate on the cornea.
- Epithelial Barrier Disruption: The corneal epithelium serves as a barrier, shielding the underlying stroma from external pathogens and debris. Inflammatory diseases and trauma can disrupt this barrier, allowing mucoid material to adhere to the corneal surface.
- Inflammatory Response: Chronic inflammation recruits inflammatory cells to the cornea, where they release cytokines and other mediators that promote mucus production and plaque formation. The presence of these plaques exacerbates the inflammatory cycle.
- Cellular Debris Accumulation: Inflammatory cells and epithelial cells going through apoptosis contribute to the debris found in mucous plaques. This cellular debris, when combined with mucus, forms a thick, adherent layer on the cornea.
Symptoms
The symptoms of corneal mucous plaques can vary in severity depending on their size and location. Common symptoms include:
- Visual Disturbances: The presence of mucous plaques on the cornea can cause severe vision impairment. Patients frequently describe blurred vision, decreased visual acuity, and difficulty focusing.
- Foreign Body Sensation: Mucous plaques cause the sensation that something is stuck in the eye, which can be extremely uncomfortable and irritating.
- Discomfort and Pain: Chronic irritation by mucous plaques can cause discomfort and pain, especially when blinking or moving the eye.
- Redness and Inflammation: The affected eye may appear red and inflamed as a result of the underlying inflammatory processes and the presence of plaques.
- Photophobia: Light sensitivity is common, making patients uncomfortable in bright environments.
Impact on Vision
Corneal mucous plaques can have a significant impact on vision, depending on their size, location, and density:
- Central Plaques: Plaques on the central visual axis cause the most severe visual impairment. They obstruct the passage of light through the cornea, causing blurred and distorted vision.
- Peripheral Plaques: While peripheral plaques do not cause immediate visual disturbance, they can still cause significant discomfort and contribute to overall vision problems if they become widespread.
- Recurrent Plaques: In cases where mucous plaques recur frequently, patients may experience chronic visual disturbances and ongoing discomfort, lowering their quality of life.
Complications:
If left untreated, corneal mucous plaques can cause a variety of complications:
- Corneal Scarring: Persistent plaques and underlying inflammation can cause corneal scarring, permanently impairing vision.
- Secondary Infections: Mucous plaques can predispose the cornea to secondary infections by disrupting the epithelial barrier, allowing pathogens to enter.
- Chronic Dry Eye: Conditions that cause mucous plaques can exacerbate dry eye syndrome, resulting in a vicious cycle of inflammation and tear film instability.
- Corneal Ulcers: Severe or untreated plaques can cause corneal ulcers, which are painful and require intensive treatment to avoid further complications.
Corneal Mucous Plaques Prevention Strategies
- Maintain Proper Eye Hygiene: Regularly clean your eyelids and lashes to remove debris and reduce the risk of inflammation.
- Use Lubricating Eye Drops: Applying preservative-free lubricating eye drops on a regular basis can help maintain a stable tear film and lower the risk of mucous plaque formation.
- Manage Underlying Conditions: Proper management of chronic inflammatory diseases and dry eye syndrome is critical. To minimize the impact on your eyes, follow your healthcare provider’s treatment recommendations for these conditions.
- Avoid Prolonged Contact Lens Wear: Follow the recommended guidelines for contact lens wear, which include proper cleaning, storage, and lens replacement on time. Avoid wearing contact lenses for long periods of time, particularly overnight.
- Protect Your Eyes: Wear protective eyewear in situations where dust, wind, or other irritants are likely. This can help prevent trauma and lower the likelihood of plaque formation.
- Stay Hydrated: Maintain adequate hydration to promote tear production and eye health. Drink plenty of water during the day.
- Follow Post-Surgery Care Instructions: If you have had eye surgery, you should follow all of your surgeon’s post-operative care instructions to promote proper healing and reduce the risk of complications like mucous plaques.
- Don’t Rub Your Eyes: Rubbing your eyes can worsen inflammation and disrupt the tear film. If your eyes are irritated, apply lubricating drops rather than rubbing them.
- Regular Eye Examinations: Schedule regular eye exams to monitor your eye health and detect any early signs of conditions that may result in mucous plaques.
- Use Anti-Inflammatory Medications: If you have chronic inflammatory conditions, take prescribed anti-inflammatory medications to reduce inflammation and the risk of ocular surface damage.
Corneal Mucous Plaques: Diagnostic Techniques
Diagnosing corneal mucous plaques requires a thorough clinical examination as well as the use of advanced diagnostic tools to accurately assess the condition. Here are some of the main diagnostic methods used:
- Patient History and Symptom Assessment: The diagnostic process begins with gathering a thorough patient history to determine the onset, duration, and severity of the symptoms. This includes inquiring about any underlying medical conditions, such as dry eye syndrome, autoimmune diseases, or recent infections.
- Slit Lamp Examination: A slit lamp is an important tool for examining the cornea in detail. During this examination, an ophthalmologist uses a high-intensity light source and a microscope to magnify the cornea. This enables the identification of mucous plaques, including their size, density, and precise location. The slit lamp exam is also useful for assessing the overall health of the ocular surface and detecting associated conditions such as inflammation or corneal ulcers.
- Fluorescein Staining: Fluorescein dye is applied to the eye’s surface, and the cornea is illuminated with cobalt blue light. This technique fluoresces defects in the corneal epithelium, making it easier to identify mucous plaques and evaluate their impact on the corneal surface.
- Tear Film Break-Up Time (TBUT): This test evaluates the stability of the tear film. A shorter TBUT indicates an unstable tear film, which can promote the formation of mucous plaques. Fluorescein dye is used in this test to see how quickly dry spots appear on the cornea after a blink.
- Ocular Surface Staining: Additional dyes, such as lissamine green or rose bengal, can be used to stain the ocular surface and identify epithelial damage or dryness. These dyes highlight mucous plaques and provide information about the severity of ocular surface disease.
- Confocal Microscopy: Confocal microscopy generates high-resolution, in-vivo images of the cornea at the cellular level. This technique is useful for detecting inflammatory cells, assessing epithelial cell health, and identifying mucous plaques that may not be visible using traditional examination methods.
- Tear Osmolarity Test: Determines the concentration of solutes in the tear film. Elevated tear osmolarity is a sign of dry eye disease, which is frequently accompanied by mucous plaque formation. This test assists in determining the underlying tear film abnormalities that contribute to the condition.
- Schirmer’s Test: To measure tear production, place a small strip of filter paper under the lower eyelid. The amount of moisture absorbed by the paper determines the level of tear production. Reduced tear production can lead to dry eye syndrome and the formation of mucous plaques.
Ophthalmologists can use these diagnostic methods to accurately diagnose corneal mucous plaques, understand the underlying causes, and devise an appropriate treatment plan.
Corneal Mucous Plaques: Treatment Methods
The treatment for corneal mucous plaques aims to relieve symptoms, remove the plaques, and address the underlying causes. Here are some emerging therapies, as well as standard treatment options:
Standard Treatments
- Lubricating Eye Drops: Regular use of preservative-free artificial tears aids in the maintenance of a stable tear film, reducing discomfort and preventing the accumulation of mucous plaques. These drops help to hydrate and lubricate the ocular surface.
- Mucolytic Agents: Eye drops containing acetylcysteine can aid in the dissolution of mucous plaques by breaking down the mucus component. These drops are often used in conjunction with lubricating eye drops.
- Anti-Inflammatory Medications: Topical corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to reduce inflammation and control the underlying inflammatory processes that cause mucous plaque formation. These medications must be used under close supervision to avoid potential side effects.
- Punctal Plugs: Punctal plugs are small devices that are inserted into the tear ducts to prevent drainage, improve tear film stability, and alleviate dry eye symptoms. Punctal plugs can help prevent mucous plaque formation by increasing tear retention.
- Autologous Serum Eye Drops: These eye drops are derived from the patient’s blood serum and contain vital growth factors and nutrients that promote healing and reduce inflammation. Autologous serum eye drops can be especially effective for severe dry eyes and ocular surface disease.
Innovative and Emerging Therapies
- Amniotic Membrane Transplantation: The amniotic membrane, which originates from the placenta’s innermost layer, has anti-inflammatory and anti-scarring properties. It can be used as a graft or as a contact lens to promote healing and reduce inflammation in patients with severe mucous plaques.
- Therapeutic Contact Lenses: Soft bandage or scleral lenses can be used to protect the cornea, promote healing, and alleviate discomfort. These lenses maintain a stable environment for the ocular surface, thereby preventing further plaque formation.
- Intense Pulsed Light (IPL) Therapy: IPL therapy, which is commonly used in dermatology, is being investigated for the treatment of dry eye syndrome and related conditions. IPL reduces inflammation and improves meibomian gland function, which may reduce the risk of mucous plaques.
- Lipid-Based Eye Drops: New formulations of lipid-based eye drops seek to stabilize the tear film by replenishing the lipid layer, reducing tear evaporation, and improving overall tear film quality. These drops may be especially beneficial for patients with evaporative dry eye and mucous plaques.
- Gene Therapy: Researchers are investigating ways to improve corneal healing and lower the risk of mucous plaques by targeting specific genes involved in tear production and inflammation.
Healthcare providers can successfully manage corneal mucous plaques, alleviate symptoms, and improve patient outcomes by combining standard treatments with innovative therapies.
Trusted Resources
Books
- “Cornea: Fundamentals, Diagnosis and Management” by Jay H. Krachmer
- “The Dry Eye Remedy” by Robert Latkany






