Introduction
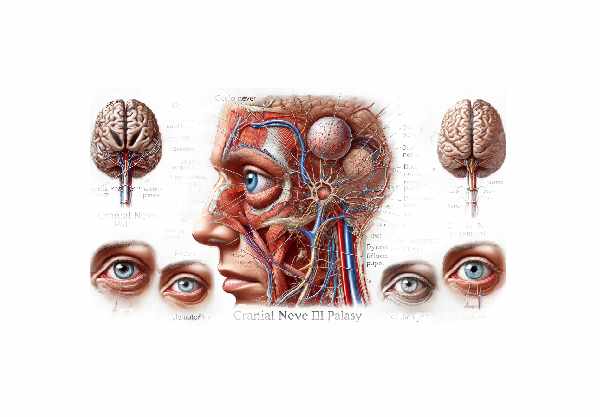
Cranial Nerve III Palsy, also known as oculomotor nerve palsy, is a neurological condition affecting the third cranial nerve, which controls the majority of the eye’s movements, eyelid lifting, and pupil constrictions. Damage or dysfunction in this nerve can cause a variety of symptoms, including double vision, drooping eyelids (ptosis), and the inability to move the eye in specific directions. This condition can be caused by a variety of factors, including vascular issues, trauma, tumors, and infections, and it frequently requires immediate medical attention to address the underlying cause and effectively manage the symptoms.
Cranial Nerve III Palsy: Insights
Cranial Nerve III Palsy is a complex condition with numerous implications for ocular function and overall well-being. Understanding this condition entails investigating the anatomy and function of the oculomotor nerve, the potential causes of its dysfunction, the various clinical manifestations, and the overall impact on patients.
Anatomy and Function
The third cranial nerve, also known as the oculomotor nerve, originates in the midbrain near the superior colliculus and exits the brainstem ventrally. It innervates several important muscles that aid in eye movement and function:
- Medial Rectus: Directs the eye inward.
- Superior Rectus: Directs the eye upward.
- Inferior Rectus: Directs the eye downward.
- Inferior Oblique: Directs the eye upwards and outward.
- Levator Palpebrae Superioris: Lifts the upper eyelids.
Additionally, the oculomotor nerve contains parasympathetic fibers that regulate pupil constriction and lens accommodation for near vision.
The causes of Cranial Nerve III Palsy
Cranial Nerve III Palsy can be divided into several broad categories based on its etiology:
Vascular Causes
- Aneurysms: A posterior communicating artery aneurysm can compress the oculomotor nerve, causing sudden-onset palsy and pain.
- Ischemic Microvascular Disease: This condition is frequently seen in older adults with diabetes or hypertension and is caused by reduced blood flow to the nerves.
Traumatic Causes: – Head Trauma: Injuries from accidents or falls can damage the oculomotor nerve, causing direct trauma or secondary effects such as hematoma or increased intracranial pressure.
Neoplastic Causes
- Tumors: Brain tumors, particularly those located in the midbrain or cavernous sinus, can cause pressure on the oculomotor nerve.
- Meningiomas and Schwannomas: These tumors, which originate in the meninges or nerve sheath, can compress or infiltrate the nerve.
Infectious and Inflammatory Causes
- Meningitis and Encephalitis: Infections with the central nervous system can cause inflammation and impair cranial nerve function.
- Multiple Sclerosis: This autoimmune disease can cause demyelination of the oculomotor nerves.
Congenital Causes: – Congenital Oculomotor Palsy This condition is present at birth and may be associated with other craniofacial abnormalities or occur on its own.
Clinical Manifestations
The symptoms of Cranial Nerve III Palsy can vary greatly depending on the extent of nerve involvement and the underlying cause. Common symptoms include:
- Ptosis: Upper eyelid drooping caused by paralysis of the levator palpebrae superioris muscle.
- Diplopia (Double Vision): Eye misalignment causes double vision, which is most noticeable when looking in the direction controlled by the affected muscles.
- Pupil Involvement: If the parasympathetic fibers are damaged, the pupil may become dilated (mydriasis) and unresponsive to light.
- Eye Movement Limitations: Unable to move the eye upward, downward, or inward, resulting in the affected eye’s characteristic “down and out” position.
Variability & Types
Cranial Nerve III Palsy is classified according to the involvement of the pupillary fibers:
- Pupil-Sparing Third Nerve Palsy: Typically associated with microvascular ischemia, where pupillary function remains intact despite other ocular motor deficits.
- Pupil-Involving Third Nerve Palsy: Often caused by compressive lesions such as aneurysms, which affect the parasympathetic fibers, resulting in pupil dilation and a lack of response to light.
Impact on Daily Life
Cranial Nerve III Palsy can severely impair a person’s daily activities and quality of life. The presence of double vision can make tasks like reading, driving, and navigating difficult. Ptosis can impair vision by obscuring part of the visual field. These symptoms can lead to a reliance on compensatory behaviors like tilting the head or covering one eye to avoid double vision, which can increase strain and discomfort.
Psychological and Social Implications
The sudden onset of symptoms, particularly in cases involving pain or significant visual impairment, can cause anxiety and stress. The condition’s visible symptoms, such as ptosis and abnormal eye movements, can have an impact on self-esteem and social interactions, potentially leading to isolation or embarrassment.
Prevention Tips
- Maintain optimal blood pressure and diabetes control to reduce the risk of microvascular diseases, which can lead to Cranial Nerve III Palsy.
- Regular Medical Check-ups: Routine health screenings can help detect and manage risk factors such as hypertension, diabetes, and high cholesterol, all of which are linked to the condition’s vascular causes.
- Wear Protective Gear: Wearing helmets and other protective gear while participating in activities that pose a risk of head injury, such as cycling and contact sports, can help prevent traumatic causes of Cranial Nerve III Palsy.
- Monitor Aneurysms and Vascular Conditions: If you are diagnosed with an aneurysm or another vascular condition, regular monitoring and prompt medical attention are essential to avoid nerve compression.
- Prevent Infections: Practice good hygiene, get vaccinated, and take precautions to avoid infections that could lead to meningitis or encephalitis, both of which can cause inflammation of the cranial nerves.
- Healthy Lifestyle Choices: Living a healthy lifestyle that includes a balanced diet, regular exercise, and abstaining from smoking and excessive alcohol consumption can reduce the risk of Cranial Nerve III Palsy.
- Seek Prompt Medical Attention: In cases of acute onset Cranial Nerve III Palsy, early intervention for symptoms such as sudden severe headache, vision changes, or eye movement abnormalities can reduce complications and improve outcomes.
Diagnostic Methods
Diagnosing Cranial Nerve III Palsy requires a comprehensive approach that includes clinical evaluation, imaging studies, and occasionally specialized tests to determine the underlying cause and extent of nerve involvement.
Clinical Evaluation
The first step in diagnosing Cranial Nerve III Palsy is a comprehensive clinical evaluation by an ophthalmologist or neurologist. This includes:
- Patient history: A thorough medical history, including the onset of symptoms, associated pain, previous medical conditions, trauma, and vascular risk factors like hypertension or diabetes.
- Physical Examination: Assessing eye movements, checking for ptosis (drooping eyelid), and determining pupil size and reactivity to light. Double vision (diplopia) and direction of gaze limitation are also observed.
Imaging Studies
Imaging is critical for determining the cause of Cranial Nerve III Palsy, particularly to rule out life-threatening conditions such as aneurysms or tumors.
- Magnetic Resonance Imaging (MRI): MRI generates detailed images of the brain and orbits, allowing for visualization of the cranial nerves, brainstem, and potential compressive lesions. It is especially effective at detecting tumors, inflammatory processes, and congenital malformations.
- Magnetic Resonance Angiography (MRA): MRA is frequently used in conjunction with MRI to evaluate the blood vessels in the brain, aiding in the identification of aneurysms or vascular malformations that may compress the oculomotor nerve.
- Computed Tomography (CT) Scan: A CT scan is commonly used in emergency situations to quickly assess acute conditions such as hemorrhages, fractures, or large masses. CT angiography can also be used to visualize blood vessels.
- Digital Subtraction Angiography (DSA): This invasive imaging technique is the most effective for detecting aneurysms and other vascular abnormalities. It generates detailed images of blood vessels that can be used to guide therapeutic interventions.
Specialized Tests
In some cases, additional tests may be required to determine the functional impact of the nerve palsy and guide treatment decisions.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): These tests measure muscle electrical activity and nerve signal speed, which can help determine the extent of nerve damage and the involvement of other cranial nerves.
- Lumbar Puncture (Spinal Tap): If an infectious or inflammatory cause is suspected, cerebrospinal fluid (CSF) analysis performed via a lumbar puncture can provide useful information.
Emerging Diagnostic Techniques
Advances in diagnostic technology improve the ability to diagnose and treat Cranial Nerve III Palsy.
- High-Resolution MRI: Advancements in MRI technology now allow for higher resolution images, improving the ability to detect subtle abnormalities and early signs of nerve compression or inflammation.
- Functional MRI (fMRI): fMRI detects blood flow changes to determine brain activity. It can provide information about how nerve palsy affects brain function and help guide rehabilitation strategies.
- Artificial Intelligence (AI) in Imaging: AI algorithms are being developed to aid in the interpretation of complex imaging data, with the potential to improve diagnostic accuracy and speed.
Treatment
Treating the Cranial Nerve III Palsy treatment entails addressing the underlying cause, relieving symptoms, and promoting nerve function recovery. The treatment approach varies according to the condition’s etiology and severity.
Standard treatment options include medical management.
- Observation: In cases where Cranial Nerve III Palsy is caused by microvascular ischemia, such as in diabetic or hypertensive patients, careful monitoring is frequently the primary approach, as many of these cases resolve spontaneously within a few months.
- Medications: Anti-inflammatory medications or antibiotics may be prescribed if the palsy is caused by inflammation or infection. Pain management may also be required.
Surgical Interventions
Surgery is considered when there is a structural cause, such as a tumor or aneurysm.
- Aneurysm Clipping or Coiling: For aneurysms that cause nerve compression, surgical clipping or endovascular coiling may be used to prevent rupture and relieve pressure on the nerve.
- Tumor Resection: Surgical removal of tumors that compress the oculomotor nerve can help restore function and alleviate symptoms.
- Decompression Surgery: In cases of traumatic injury or other compressive lesions, decompression surgery may be required to relieve pressure on the nerve.
Supportive Treatments
Supportive therapies seek to improve symptoms and quality of life.
- Prism Glasses: Special glasses with prisms can help with double vision by aligning the visual images.
- Eye Patching: Covering one eye can help reduce double vision and increase comfort.
- Botulinum Toxin (Botox) Injections: Injecting Botox into specific eye muscles can temporarily correct misalignment and improve eye movement.
- Physical Therapy: Therapy aimed at improving eye movement and coordination can help with recovery.
Innovative and Emerging Therapies ### Neurostimulation
Neurostimulation techniques, such as transcranial magnetic stimulation (TMS), are being investigated for their potential to improve nerve regeneration and functional recovery.
Regenerative Medicine
Advances in regenerative medicine, such as stem cell therapy and nerve growth factors, are being studied for their ability to repair and regenerate damaged nerve tissues.
Minimally Invasive Surgery
Minimally invasive surgical techniques are being developed to shorten recovery times and improve outcomes in patients requiring surgery for Cranial Nerve III Palsy.
Personalized Medicine
Patients’ genetic and molecular profiles are being used to develop personalized treatment plans that target specific underlying causes and improve therapeutic efficacy.
Trusted Resources
Books
- “Neuro-Ophthalmology Illustrated” by Valerie Biousse and Nancy J. Newman
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakrabarti
- “Cranial Nerves: Functional Anatomy” by Stanley Monkhouse






