Introduction to Duane Retraction Syndrome
Duane Retraction Syndrome (DRS) is a rare congenital eye movement disorder defined by the inability of one or both eyes to move outward (abduction) or inward (adduction). Alexander Duane first described this condition in 1905, and it is caused by an abnormal development of the sixth cranial nerve, which controls the lateral rectus muscle responsible for eye movement. Instead of moving smoothly, the affected eye(s) retract into the socket, causing an abnormal narrowing of the palpebral fissure (the space between the eyelids). DRS affects approximately one in 1,000 to 10,000 people, with females having a slightly higher prevalence. Understanding the complexities of Duane Retraction Syndrome is critical for proper diagnosis and treatment.
Duane Retraction Syndrome: Insights
Etiology and Pathophysiology
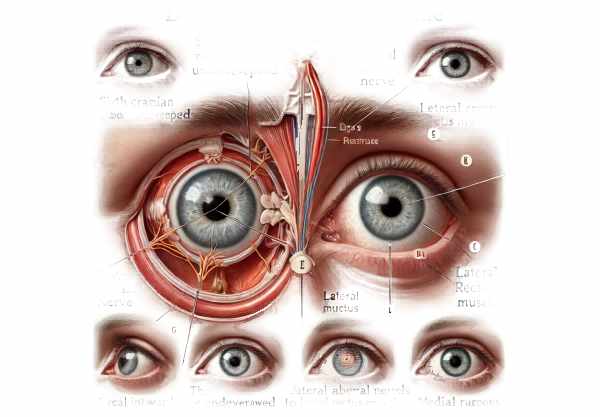
Duane Retraction Syndrome is primarily a congenital condition, which means it is present from birth. It occurs when the sixth cranial nerve fails to properly innervate the lateral rectus muscle. Normally, this nerve causes the lateral rectus muscle to abduct the eye. In DRS, this nerve is either absent or underdeveloped. As a result, the third cranial nerve, which normally innervates the medial rectus muscle, may send abnormal signals to the lateral rectus muscle. When the eye moves inward or outward, the palpebral fissure retracts and narrows due to this miswiring.
Classification of DRS
DRS is classified into three major types based on movement limitations and eye position:
- Type I: The most common type, in which the affected eye has little or no ability to move outward (abduction). However, inward movement (adduction) is usually normal or nearly so.
- Type II: Characterized by restricted inward movement (adduction), while outward movement (abduction) is normal or nearly normal. This type is less common.
- Type III: Restricts inward and outward movements. This type is also less common than Type I.
Symptoms and Clinical Presentation
The symptoms of Duane Retraction Syndrome vary according to the severity and type. Common clinical characteristics include:
- Abnormal Head Posture: To compensate for limited eye movement, people with DRS frequently adopt an abnormal head posture. This may include turning or tilting the head to maintain binocular vision and avoid double vision (diplopia).
- Retraction of the Eyeball: As the affected eye moves inward, it retracts into the socket, narrowing the palpebral fissure. This retraction is one of the defining characteristics of DRS.
- Strabismus: Eye misalignment is common in DRS. The affected eye can be turned inward (esotropia) or outward (exotropia), depending on the type of DRS.
- Restricted Eye Movement: Depending on the type of DRS, the eye’s ability to move outward or inward may be significantly reduced. This can make it difficult to track objects and interfere with depth perception.
- Compensatory Head Turn: People with DRS frequently turn their heads to the side to better align their eyes and maintain clear vision, particularly when viewing objects in their peripheral vision.
Genetic and Environmental Factors
Although the exact cause of Duane Retraction Syndrome is unknown, genetic and environmental factors are thought to play a role. In some cases, DRS develops sporadically without a family history. However, there are cases where DRS has an autosomal dominant inheritance pattern, implying a genetic component.
Mutations in the CHN1 gene have been linked to some cases of DRS. This gene is involved in the formation of ocular motor nerves. However, not all cases of DRS are associated with CHN1 mutations, implying that other genetic or environmental factors may also contribute to the condition.
Associated Conditions
Duane Retraction Syndrome can occur alone or in combination with other systemic conditions. Some associated conditions are:
- Congenital Syndromes: DRS may be part of a larger congenital syndrome, such as Goldenhar syndrome or Wildervanck syndrome, which include additional craniofacial and skeletal abnormalities.
- Hearing Loss: Some people with DRS may develop hearing loss as a result of associated cranial nerve anomalies.
- Vertebral Anomalies: Vertebral abnormalities, such as fusion or segmentation defects, can be linked to DRS.
Effects on Quality of Life
The effect of Duane Retraction Syndrome on quality of life varies with the severity of the symptoms. Individuals with mild cases may have few functional limitations and can live normal lives with little or no intervention. However, severe cases can have a significant impact on daily activities such as reading, driving, and sports. The abnormal head posture used to compensate for eye movement limitations can cause neck and back strain over time.
Complications
If left untreated, Duane Retraction Syndrome can cause a number of complications, including:
- Amblyopia, also known as “lazy eye,” occurs when one eye is consistently misaligned and not used for vision.
- Diplopia: Persistent double vision can impair depth perception and coordination.
- Musculoskeletal Issues: Chronic abnormal head posture can cause neck and back problems over time.
Prevention Tips
- Early Diagnosis and Intervention: Proper management of Duane Retraction Syndrome requires early detection and treatment. Regular eye exams can help detect DRS early and provide timely treatment to avoid complications.
- Genetic Counseling: For families with a history of DRS, genetic counseling can provide important information about the risk of passing the condition down to children. Genetic testing can aid in identifying potential DRS-associated mutations.
- Regular Eye Examinations: Individuals with DRS require ongoing monitoring by an ophthalmologist to manage symptoms and avoid complications such as amblyopia and diplopia.
- Occupational Therapy: Occupational therapy can assist individuals with DRS in developing strategies to adapt to their condition, improving their ability to perform daily activities and lowering the risk of musculoskeletal problems.
- Physical therapy can help with musculoskeletal issues caused by abnormal head posture. Exercises and stretches can help relieve neck and back pain, enhancing overall comfort and function.
- Protective Eyewear: Wearing protective eyewear during activities that could cause eye injury can help prevent further complications in people with DRS.
- Awareness and Education: Educating people with DRS and their families about the condition can help them manage symptoms more effectively and seek appropriate medical care.
- Adaptive Techniques: Learning adaptive techniques, such as head positioning and the use of visual aids, can help people with DRS improve their vision and reduce strain on their eyes and muscles.
- Healthy Lifestyle: Adhering to a healthy lifestyle, which includes a balanced diet and regular exercise, can improve overall well-being and may indirectly benefit eye health.
- Support Groups: Joining a support group for people with Duane Retraction Syndrome can provide emotional support, allow you to share your experiences, and give you practical advice on how to manage the condition.
Diagnostic Process for Duane Retraction Syndrome
Duane Retraction Syndrome (DRS) is diagnosed using a combination of clinical and imaging studies, as well as genetic testing when applicable. The goal is to confirm the diagnosis, determine the severity of the condition, and rule out any other potential causes of similar symptoms.
- Comprehensive Eye Examination: An ophthalmologist’s initial evaluation consists of a detailed medical history and a thorough eye examination. This helps to understand the onset, duration, and severity of symptoms.
- Visual Acuity Test: This test determines the clarity of vision in each eye. It aids in determining whether there is a reduction in visual acuity, which may be associated with amblyopia or other DRS complications.
- Cover Test: This test is used to determine eye alignment. The patient is instructed to focus on an object while one eye is covered, and the movement of the uncovered eye is monitored. This test can detect the presence and type of strabismus associated with DRS.
- Eye Movement Assessment: Observing the range and coordination of eye movements is critical for diagnosing DRS. The ophthalmologist will be looking for limitations in abduction (outward movement) and adduction (inward movement), as well as any abnormal retraction of the eyeball during these movements.
- Binocular Vision Assessment: Tests like the Worth 4-Dot test or the use of prism lenses can assess how well the eyes work together, revealing problems with binocular vision and depth perception.
Innovative Diagnostic Techniques
- Imaging Studies: Advanced imaging techniques, such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT), can produce detailed images of the brain, eye muscles, and cranial nerves. These studies aid in the identification of structural abnormalities in the ocular motor nerves and muscles, confirming the diagnosis of DRS.
- Electrophysiological Testing: Visual Evoked Potentials (VEP) and Electromyography (EMG) can be used to evaluate the functional integrity of the visual pathways as well as neuromuscular control of the eye muscles. These tests provide more information about the severity and nature of the neural dysfunction in DRS.
- Genetic Testing: If there is a family history of DRS or other related genetic conditions, genetic testing may be beneficial. Identifying mutations in genes such as CHN1 can help confirm the diagnosis and shed light on the condition’s hereditary aspects.
- Digital Imaging and Analysis: Modern ophthalmologists frequently use high-resolution digital imaging to capture and analyze eye movements. This technology enables accurate measurement and documentation of the extent of eye movement limitation and retraction, which aids in diagnosis and treatment planning.
Comprehensive Evaluation
A thorough evaluation using these established and novel diagnostic techniques ensures an accurate diagnosis of Duane Retraction Syndrome. It also aids in understanding the unique characteristics of the condition in each patient, which is critical for developing an effective treatment plan.
Effective Treatment for Duane Retraction Syndrome
The treatment of Duane Retraction Syndrome (DRS) aims to improve ocular alignment, binocular vision, and symptoms. While there is no cure for DRS, a variety of treatment options can help manage it effectively.
Standard Treatment Options
- Observation and Monitoring: In mild cases of DRS, where symptoms are minor and have no significant impact on daily activities, careful observation and regular monitoring by an ophthalmologist may be sufficient. This approach ensures that any symptoms that worsen are treated as soon as possible.
- Corrective Lenses: Glasses or contact lenses can help correct refractive errors and improve visual acuity. In some cases, prism lenses may be used to align the eyes and reduce double vision.
- Vision Therapy: A set of exercises designed to improve binocular vision and coordination. While it may not correct the underlying muscular or nerve abnormalities, it can help relieve symptoms and improve functional vision.
- Botulinum Toxin Injections: Injecting Botox into the affected eye muscles can temporarily reduce muscle overactivity, which improves alignment and reduces retraction. This treatment is frequently used as a temporary fix or for diagnostic purposes.
Surgical Treatment Alternatives
- Strabismus Surgery: Surgery to correct ocular misalignment is a common treatment for DRS. The affected eye muscles are typically repositioned or weakened in order to improve alignment and reduce retraction. The specific surgical approach is determined by the type and severity of DRS.
- Recession and Resection Surgery: This surgical technique involves reducing (weakening) the overacting muscle and strengthening the underacting muscle. It seeks to balance the forces acting on the eye, thereby improving its movement and alignment.
- Vertical Rectus Muscle Transposition: When standard horizontal muscle surgery is insufficient, vertical rectus muscle transposition can be used. This procedure involves repositioning the vertical muscles to support the eye’s horizontal movement.
Innovative and Emerging Therapies
- Minimally Invasive Surgery: Advances in surgical techniques have resulted in the creation of minimally invasive procedures that shorten recovery time and improve outcomes. These methods employ smaller incisions and advanced tools to make more precise muscle adjustments.
- Stem Cell Therapy: Research into stem cell therapy has shown promise in regenerating damaged nerve cells and improving muscle function. While still in the experimental stage, this approach may provide new hope for treating congenital nerve and muscle anomalies in the future.
- Gene Therapy: As genetic research advances, gene therapy could become a viable option for correcting the underlying genetic mutations linked to DRS. This treatment would entail repairing or replacing damaged genes to restore normal nerve and muscle function.
- Neurostimulation Devices: Devices that stimulate the cranial nerves that control eye movement are being investigated as a possible treatment for DRS. These devices use targeted electrical stimulation to improve nerve function and muscle coordination.
Trusted Resources
Books
- “Pediatric Ophthalmology and Strabismus” by David Taylor and Creig S. Hoyt
- “Clinical Strabismus Management: Principles and Surgical Techniques” by Arthur L. Rosenbaum and Alvina Pauline Santiago
- “Strabismus: A Decision-Making Approach” by John P. Whitcher, Paul Riordan-Eva, and Patrick J. P. Spiteri Cornish










