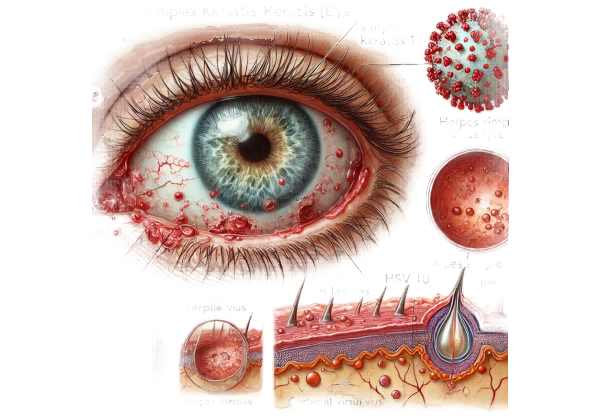
What is herpes simplex keratitis?
Herpes simplex keratitis (HSK) is an ocular infection caused by the herpes simplex virus (HSV), specifically HSV-1. It is the leading cause of infectious blindness in developed countries, and if not treated properly, it can cause recurring corneal infections, resulting in significant visual impairment. The virus infects the cornea, causing inflammation and ulcers. Symptoms include eye pain, redness, blurred vision, tearing, and light sensitivity. Early diagnosis and treatment are critical for avoiding complications and preserving vision.
Comprehensive Guide to Herpes Simplex Keratitis
Herpes Simplex Keratitis (HSK) is a complex, recurring corneal infection caused primarily by herpes simplex virus type 1 (HSV-1). Herpes simplex virus type 2 (HSV-2) is occasionally implicated, usually after genital herpes infections. HSV-1 is commonly associated with orofacial infections, but it can also reactivate and spread to the eye, resulting in HSK.
Pathophysiology
HSV-1 infection of the cornea usually starts with a primary exposure, often during childhood, and progresses to a latent infection in the trigeminal ganglion. Stress, fever, UV light exposure, or immunosuppression can all cause the virus to reactivate after years of dormancy. When the virus reactivates, it travels along the trigeminal nerve to the cornea, resulting in recurring keratitis.
The corneal infection can be classified into different types depending on the depth and area of corneal involvement.
- Epithelial Keratitis is the most common initial manifestation, with dendritic ulcers on the corneal surface. These ulcers are branching lesions that stain with fluorescein dye and are excellent indicators of HSV infection.
- Stromal Keratitis: This form affects the cornea’s deeper layers and can result in stromal necrosis and scarring. Stromal keratitis can be either necrotizing or non-necrotizing, and it is frequently immune-mediated, resulting in significant visual impairment if not treated.
- Endothelial Keratitis: Inflammation of the innermost corneal layer, which causes disciform keratitis with disc-shaped stromal edema. This can cause decreased vision and corneal decompensation.
Clinical Manifestations
The clinical presentation of HSK varies according to the type and severity of infection. Common symptoms include:
- Eye Pain: Typically a sharp or throbbing sensation.
- Redness: Conjunctival hyperemia near the cornea.
- Tearing is excessive lacrimation caused by irritation.
- Photophobia: sensitivity to light.
- Blurred Vision: Result of corneal involvement and scarring.
- Discharge: Watery discharge, rather than the purulent discharge seen in bacterial infections.
Epidemiology
HSK is a major cause of corneal blindness worldwide. It is estimated that approximately 1.5 million people are affected worldwide, with approximately 40,000 new cases of severe visual impairment or blindness reported each year. Recurrent episodes are common, and each recurrence raises the possibility of corneal scarring and vision loss.
Risk Factors
Several factors can raise the risk of developing HSK, including:
- History of HSV Infection: Past orofacial herpes infections.
- Immunosuppression: HIV/AIDS, using immunosuppressive drugs, or undergoing chemotherapy.
- UV Light Exposure: Sunlight and UV lamps can cause reactivation.
- Stress: Physical or emotional stress may trigger reactivation.
- Trauma to the Eye: Corneal abrasions or surgeries can allow viral entry.
Complications:
HSK can cause a variety of complications, particularly with recurring infections. This includes:
- Corneal Scarring: Causes permanent visual impairment.
Severe stromal keratitis can cause corneal thinning and perforation. - Secondary Bacterial Infections: The compromised corneal epithelium can become infected with bacteria.
- Glaucoma: Inflammation can cause increased intraocular pressure and damage to the optic nerve.
- Uveitis: Inflammation of the uveal tract, which can lead to additional vision loss.
Immunopathology
HSK pathogenesis involves both direct viral cytotoxicity and host immune responses. Immune-mediated damage is particularly important in stromal keratitis. The immune response consists of both innate and adaptive components, with neutrophils, T-cells, and cytokines contributing to tissue damage. Understanding immune involvement has been critical in developing treatment strategies that target the virus while also modulating the immune response to prevent corneal damage.
Diagnostics
HSK is diagnosed using clinical signs, patient history, and diagnostic tests. The presence of dendritic ulcers is strongly suggestive of HSV infection. Confirmatory tests involve:
- Fluorescein Staining identifies dendritic ulcers.
- PCR Testing: Detects HSV DNA from corneal scrapings.
- Viral Culture: Isolates the virus from ocular samples, but is less commonly used due to the time commitment.
Disease Management & Patient Education
Managing HSK entails not only treating the acute infection, but also preventing recurrences and managing complications. Patient education on identifying early symptoms and avoiding triggers is critical. Stress management, UV protection, and early treatment of recurrences can help to reduce the frequency and severity of episodes.
Diagnostic methods
Herpes Simplex Keratitis is diagnosed using a combination of clinical examination, laboratory tests, and imaging techniques. Accurate diagnosis is critical for providing appropriate treatment and avoiding complications.
Clinical Examination
The initial diagnosis of HSK is frequently based on a clinical examination and patient history. Key features include:
- Visual Acuity Testing: Determine the infection’s impact on vision.
- Slit Lamp Examination: A thorough examination of the cornea with a slit lamp microscope to detect distinguishing features such as dendritic ulcers, stromal haze, and endothelial deposits.
Lab Tests
Laboratory tests are essential for confirming a diagnosis, particularly in atypical cases or when the clinical presentation is unclear.
- Fluorescein Staining: An important diagnostic tool in which fluorescein dye is applied to the eye, highlighting dendritic ulcers under blue light. These ulcers indicate HSV infection.
- Polymerase Chain Reaction (PCR): PCR testing of corneal scrapings detects HSV DNA with high sensitivity and specificity. It is especially useful in situations where the clinical diagnosis is uncertain.
- Viral Culture: Although less commonly used due to the time commitment, viral culture from corneal swabs can detect HSV infection. This method involves growing the virus in cell culture and identifying it using immunofluorescence or other techniques.
- Tzanck Smear: A cytological test in which cells from the corneal lesion are stained and examined under a microscope to detect multinucleated giant cells, indicating HSV infection.
Imaging Techniques
Imaging techniques can reveal additional details about the extent and type of corneal involvement.
- Confocal Microscopy: This imaging technique allows for detailed visualization of the corneal layers, including the identification of inflammatory cells and viral particles.
- Anterior Segment Optical Coherence Tomography (AS-OCT): Provides high-resolution cross-sectional images of the cornea, which are useful for determining stromal and endothelial involvement.
Approaches to Treating Herpes Simplex Keratitis
Herpes Simplex Keratitis (HSK) is treated with antiviral therapy to control the viral infection, anti-inflammatory medications to manage the immune response, and supportive care to promote corneal healing and prevent complications. Early and appropriate treatment is critical for preventing vision loss and lowering the risk of recurrence.
Standard Treatment Options
- Antiviral Medications: The cornerstone of HSK treatment is antiviral medication. Commonly used antivirals include:
- Topical Antivirals: Trifluridine (Viroptic), ganciclovir (Zirgan), and acyclovir ointment can help treat epithelial keratitis. These medications work by inhibiting viral replication and promoting dendritic ulcer healing.
- Oral Antivirals: Acyclovir, valacyclovir, and famciclovir are frequently prescribed to treat stromal and endothelial keratitis, as well as to prevent future episodes. Oral antivirals are especially effective for treating severe infections and patients who do not tolerate topical treatments.
- Corticosteroids: Topical corticosteroids (such as prednisolone acetate) are used to treat stromal and endothelial keratitis by reducing inflammation and scarring. Corticosteroids, on the other hand, should be used with caution and under the close supervision of an ophthalmologist, as they can exacerbate the viral infection if not managed properly.
- Cycloplegic Agents: These medications (e.g., atropine, cyclopentolate) dilate the pupil and reduce ciliary muscle spasms, thereby relieving pain and preventing synechiae formation.
- Supportive Care: Lubricating eye drops and ointments can help relieve dry eye symptoms while also promoting corneal healing. Patching or protective contact lenses may be used in certain circumstances to protect the cornea and improve patient comfort.
Innovative and Emerging Therapies 1. New Antiviral Agents Research is being conducted to develop new antiviral medications with greater efficacy and fewer side effects. For example, pritelivir and brincidofovir are newer agents being studied for their ability to treat HSK.
- Immunomodulatory Therapies: Understanding the immune response in HSK has prompted the development of immunomodulatory treatments. Drugs that target the inflammatory pathways involved in stromal keratitis, such as interleukin inhibitors, are being investigated.
- Gene Therapy: Gene editing technologies like CRISPR/Cas9 have the potential to directly target and eliminate HSV DNA in the cornea. While still in the experimental stage, these approaches may provide long-term solutions to recurring HSK.
- Vaccines: The development of an HSV-1 vaccine could prevent both primary infection and subsequent reactivation. Several vaccine candidates are currently undergoing preclinical and clinical trials with the goal of providing long-term immunity against HSV.
Surgical Interventions
In severe cases of HSK with extensive corneal scarring or perforation, surgical intervention may be required.
- Corneal Transplantation: In cases of severe corneal scarring, a penetrating or lamellar keratoplasty may be required to restore vision.
- Amniotic Membrane Transplantation: A procedure used to promote healing and reduce inflammation in refractory cases.
Healthcare providers can better manage Herpes Simplex Keratitis by combining standard treatments with innovative therapies that reduce the frequency and severity of recurrences while also preserving vision.
Best Practices for Avoiding Herpes Simplex Keratitis
- Avoid Eye Contact with Infected Areas: If you have an active herpes simplex infection (for example, a cold sore), avoid touching your eyes and wash your hands frequently to avoid spreading the virus.
- Use UV Protection: Wear UV-blocking sunglasses to reduce the risk of reactivation caused by sunlight exposure.
- Manage Stress: Practice stress-reduction techniques like meditation, exercise, and getting enough sleep, as stress can cause viral reactivation.
- Maintain a Healthy Immune System: Eating a healthy diet, exercising regularly, and avoiding smoking and excessive alcohol consumption can all help strengthen your immune system and lower your risk of reactivation.
- Regular Eye Examinations: If you have a history of HSK, regular visits to an ophthalmologist can help detect early signs of reactivation and prompt treatment.
- Avoid Contact Lenses During Active Infection: If you wear contact lenses, do not use them while you have an active herpes simplex infection to avoid further irritation and virus spread.
- Early Treatment of Recurrences: Seek medical attention as soon as you notice symptoms like eye pain, redness, or blurred vision to begin antiviral treatment and avoid complications.
- Use Antiviral Prophylaxis: Long-term antiviral prophylaxis (such as daily oral acyclovir) can help reduce the frequency of episodes and prevent serious complications in people who have recurrent infections.
Individuals at risk for Herpes Simplex Keratitis can lower their chances of reactivation and protect their vision by taking these precautions.
Trusted Resources
Books
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
- “Herpetic Eye Diseases: Their Management and Treatment” by James P. Dunn and Robert B. Nussenblatt
- “Corneal Surgery: Theory, Technique, and Tissue” by Frederick S. Brightbill