What is infectious uveitis?
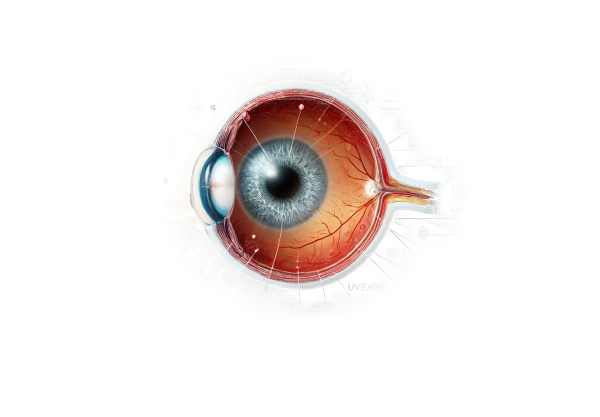
Infectious uveitis is a serious infection-related inflammation of the uveal tract, the eye’s middle layer. The uveal tract consists of the iris, ciliary body, and choroid, all of which are necessary for blood supply to the retina. Bacteria, viruses, fungi, and parasites are all possible pathogens that could cause this condition. If not diagnosed and treated promptly, infectious uveitis can cause severe visual impairment or blindness. The inflammation can affect one or both eyes and may be acute or chronic, with the possibility of recurrence over time.
Extensive Review of Infectious Uveitis
The location of the inflammation within the uveal tract and the type of infectious agent responsible determine the classification of infectious uveitis. Understanding the underlying causes, clinical manifestations, and potential complications is critical for timely diagnosis and management.
Causes and Pathogens
The pathogens responsible for infectious uveitis are diverse, including:
- Bacteria: Common bacterial causes are Mycobacterium tuberculosis, Treponema pallidum (syphilis), Bartonella henselae (cat scratch disease), and Borrelia burgdorferi (Lyme disease). These bacteria can enter the uveal tract directly or via hematogenous spread.
- Viruses: The following viral infections can cause uveitis: herpes simplex virus (HSV), varicella-zoster virus (VZV), cytomegalovirus (CMV), and rubella virus. These viruses can cause a significant inflammatory response in the eyes.
- Fungi: Fungal infections, while uncommon, can be severe. Pathogens such as Candida species, Aspergillus, and Histoplasma capsulatum can enter the uveal tissues, especially in immunocompromised people.
- Toxoplasmosis, caused by Toxoplasma gondii, is a significant contributor to infectious uveitis. Other parasites include Toxocara canis and Onchocerca volvulus (river blindness).
Clinical Manifestations
The symptoms of infectious uveitis differ depending on the pathogen, the site of inflammation, and the severity of the infection. Common clinical characteristics include:
- Anterior Uveitis: This type, also known as iritis, causes inflammation of the iris and anterior chamber. Symptoms may include eye pain, redness, photophobia, and blurred vision. The presence of keratic precipitates, anterior chamber cells, and flare are distinguishing features.
- Intermediate Uveitis: In this type, the inflammation primarily affects the vitreous body and the peripheral retina. Patients frequently report floaters, blurred vision, and mild discomfort. Snowbanking or snowballs (inflammatory aggregates) in the vitreous are common findings.
- Posterior Uveitis: This affects the retina and choroid, causing symptoms like floaters, blurred vision, and loss of visual acuity. Retinal vasculitis, choroiditis, and retinitis are common findings on fundoscopic examination.
- Panuveitis: This severe form affects the entire uveal tract and presents with symptoms similar to anterior, intermediate, and posterior uveitis. It can cause significant visual impairment and is often difficult to manage.
Pathogenesis
Infectious uveitis develops when pathogens invade ocular tissues, triggering an immune response. The inflammatory process aims to eliminate the infection, but it can also cause tissue damage. The body’s immune response, which includes the activation of T-cells and macrophages, is critical in the pathophysiology. Cytokines and chemokines produced during the inflammatory response help to recruit immune cells to the site of infection.
Complications
Infectious uveitis can cause severe complications if not treated or managed properly, including:
- Cataracts: Chronic inflammation can cause the formation of cataracts, resulting in progressive vision loss.
- Glaucoma: Increased intraocular pressure due to inflammation or corticosteroid treatment can damage the optic nerve, resulting in glaucoma.
- Retinal Detachment: Inflammation can result in tractional or rhegmatogenous retinal detachment, requiring immediate surgical intervention.
- Macular Edema: A common complication of uveitis is the accumulation of fluid in the macula, which can significantly impair central vision.
- Optic Neuritis: Inflammation of the optic nerve can result in pain and vision loss.
Diagnostic Challenges
Because of the variety of clinical presentations and potential pathogens, diagnosing infectious uveitis can be difficult. A thorough history, including travel, exposure, and systemic symptoms, is required to determine the possible cause. Laboratory tests and imaging studies are critical in determining the diagnosis.
Epidemiology
Geographic and socioeconomic factors influence the prevalence and incidence of infectious uveitis around the world. For example, tuberculosis-related uveitis is more common in areas with a high tuberculosis prevalence, whereas toxoplasmosis is a leading cause of posterior uveitis globally. Understanding epidemiological patterns aids in identifying at-risk populations and implementing effective screening measures.
Immunocompromised Patients
Individuals with weakened immune systems, such as those with HIV/AIDS or receiving immunosuppressive therapy, are more likely to develop infectious uveitis. Opportunistic infections, such as CMV retinitis, are particularly prevalent in these patients. Early detection and tailored treatment are critical for avoiding severe ocular and systemic complications.
Genetic Predisposition
Genetic factors can affect an individual’s susceptibility to infectious uveitis. For example, certain HLA genotypes increase the risk of developing uveitis in response to specific pathogens. Research into the genetic predisposition to infectious uveitis could lead to better screening and personalized treatment options.
Prognosis
The prognosis of infectious uveitis is determined by how quickly it is diagnosed, how effective the treatment is, and what the underlying cause is. While some types of uveitis can be treated successfully with little long-term impact, others can cause irreversible vision loss and chronic complications. Regular follow-up and monitoring are required to ensure optimal results and avoid recurrences.
Methods to Diagnose Infectious Uveitis
To identify the causative pathogen and determine the extent of inflammation in infectious uveitis, a comprehensive approach is required, combining clinical examination with laboratory and imaging studies.
Clinical Examination
A thorough clinical examination is the first step in diagnosing infectious uveitis. This includes:
- Visual Acuity Test: Evaluating the patient’s visual acuity aids in determining the effect of uveitis on vision.
- Slit-Lamp Examination: This allows for detailed visualization of the anterior segment of the eye, revealing signs such as keratic precipitates, anterior chamber cells, and flares.
- Fundoscopy: An examination of the posterior segment reveals findings such as retinal vasculitis, choroiditis, and vitreous inflammation.
Lab Tests
Laboratory investigations are critical in determining the specific pathogen causing uveitis. This may include:
- Blood Tests: Complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels indicate systemic inflammation.
- Serological Tests: Tests for specific antibodies or antigens, such as syphilis, toxoplasmosis IgG and IgM, and tuberculosis QuantiFERON-TB Gold, aid in the identification of the infectious agent.
- Polymerase Chain Reaction (PCR): PCR testing on aqueous or vitreous samples can detect viral, bacterial, or parasitic DNA and provide a precise diagnosis.
Imaging Studies
Imaging studies are critical for determining the severity of ocular inflammation and detecting complications. This includes:
- Optical Coherence Tomography (OCT): OCT uses high-resolution images of the retina and choroid to detect macular edema and structural changes.
- Fluorescein Angiography: This imaging technique visualizes retinal blood vessels and detects leakage or ischemia.
- Ultrasound Biomicroscopy: Used in cases of media opacities, this technique provides detailed images of the anterior segment.
Ancillary tests
Additional tests may be required, depending on the suspected etiology:
- Chest X-ray or CT Scan: Helps diagnose tuberculosis or sarcoidosis-related uveitis.
- Skin Tests: For tuberculosis screening, use the Tuberculin Skin Test or the Mantoux Test.
Infectious Uveitis Treatment
Treating infectious uveitis requires a multifaceted approach that addresses both the infectious agent and the inflammatory response it causes. The pathogen’s identification, the severity of the inflammation, and the patient’s overall health status all influence treatment selection.
Antimicrobial Therapy
- Antibiotics: Bacterial uveitis is treated with appropriate antibiotics based on culture and sensitivity findings. For example, doxycycline or azithromycin are used to treat Bartonella infections, whereas intravenous antibiotics are required for serious cases such as tuberculosis or syphilis.
- Antivirals: Antiviral medications are used to treat viral uveitis, such as herpes simplex and cytomegalovirus. Acyclovir, valacyclovir, and ganciclovir are frequently used to inhibit viral replication and reduce inflammation.
- Antifungals: Antifungal therapy is often required for fungal uveitis, with agents such as amphotericin B, fluconazole, or voriconazole. Treatment may be prolonged, but it is critical for eliminating the infection.
- Antiparasitics: Toxoplasmosis and other parasitic uveitis are treated with a combination of antiparasitic drugs such as pyrimethamine and sulfadiazine, which are frequently used in conjunction with corticosteroids to manage inflammation.
Anti-inflammatory Therapy
- Corticosteroids: These are the cornerstones of uveitis anti-inflammatory therapy. They can be given topically, orally, or as periocular or intraocular injections, depending on the severity and location of the inflammation. However, careful monitoring is required due to possible side effects such as increased intraocular pressure and cataract formation.
- Immunomodulatory Drugs: When corticosteroids are ineffective or contraindicated, immunosuppressive agents such as methotrexate, azathioprine, or mycophenolate mofetil may be used. These drugs reduce inflammation by modulating the immune response.
Emerging Therapies
- Biologics: Monoclonal antibodies targeting specific immune system components, such as TNF-α inhibitors, are being investigated for their potential in treating refractory uveitis. Examples include adalimumab and infliximab.
- Intravitreal Implants: Sustained-release intravitreal implants containing corticosteroids or other anti-inflammatory drugs are a promising treatment for chronic uveitis. These implants provide long-term inflammation relief with few systemic side effects.
- Gene Therapy: Experiments with gene therapy aim to deliver anti-inflammatory genes directly to ocular tissues, potentially providing a long-term solution for chronic uveitis without the need for ongoing medication.
Supportive Care
- Pain Management: Analgesics and cycloplegic agents may be used to treat pain and photophobia caused by anterior uveitis.
- Monitoring and Follow-up: Regular follow-up visits are critical for monitoring treatment response, adjusting medications, and detecting complications early on.
Effective management of infectious uveitis necessitates a comprehensive approach tailored to the specific needs of each patient, which frequently involves collaboration among ophthalmologists, infectious disease specialists, and other healthcare providers.
Effective Ways to Improve and Prevent Infectious Uveitis
There are several strategies for preventing infectious uveitis and minimizing its impact. Here are key measures to consider:
- Maintain Good Hygiene: Regular hand washing and avoiding touching your eyes with dirty hands can help reduce the risk of infection.
- Vaccinations: Keep up with vaccinations, such as the herpes zoster vaccine, to avoid viral infections that can lead to uveitis.
- Prompt Treatment of Systemic Infections: Early treatment of systemic infections such as tuberculosis, syphilis, and HIV can prevent the pathogens from spreading to the eyes.
- Regular Eye Examinations: Routine eye exams can help detect early signs of uveitis and other ocular conditions, allowing for timely intervention.
- Use Protective Eyewear: Wearing protective eyewear in environments with a high risk of ocular trauma or exposure to infectious agents can help prevent infections.
- Manage Underlying Health Conditions: Managing chronic health conditions like diabetes and autoimmune diseases can lower the risk of opportunistic infections that lead to uveitis.
- Safe Contact Lens Practices: To avoid microbial keratitis and subsequent uveitis, keep contact lenses clean and avoid overnight wear.
- Toxoplasmosis Avoidance: To prevent toxoplasmosis, thoroughly cook meat, wash fruits and vegetables, and avoid contact with cat litter.
- Immediate Medical Attention for Eye Symptoms: Seek medical attention right away if you notice any signs of an eye infection, pain, redness, or vision changes to avoid complications.
- Educating High-Risk Populations: Teach preventive measures to people who are at higher risk, such as those with immunosuppressive conditions.
Implementing these measures has the potential to significantly reduce the incidence of infectious uveitis while also improving outcomes for those affected.
Trusted Resources
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- “Ocular Inflammatory Disease” by Jack J. Kanski and Carlos Pavesio
- “Intraocular Inflammation: Uveitis and Ocular Immunology” by Manfred Zierhut, Hans-Georg Rammensee, and Joachim W. Meyer
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- Uveitis Information Group: www.uveitis.net
- Ocular Immunology and Uveitis Foundation: www.uveitis.org
- Mayo Clinic: www.mayoclinic.org






