What is Limbal Stem Cell Deficiency?
Limbal stem cell deficiency (LSCD) is an ocular condition characterized by the absence or dysfunction of limbal stem cells, which are essential for the maintenance and regeneration of the corneal epithelium. The limbus, which separates the cornea from the sclera, contains these stem cells. When these cells become damaged or depleted, the cornea can become opaque, resulting in vision impairment or blindness. Genetic disorders, chemical injuries, infections, and inflammatory diseases are all contributing factors to LSCD.
Detailed Investigation of Limbal Stem Cell Deficiency
Limbal stem cell deficiency (LSCD) is a major challenge in ophthalmology due to its impact on vision and the difficulties associated with its treatment. To fully comprehend the condition, it is necessary to understand the anatomy of the limbus, the role of limbal stem cells, and the mechanisms that cause LSCD.
Anatomy and Function of the Limbus
The limbus is the space between the cornea and the sclera. It is critical to ocular health because it houses the limbal stem cells that regenerate the corneal epithelium. These stem cells are constantly producing new cells to replace the old or damaged cells on the corneal surface, ensuring its transparency and integrity. The corneal epithelium is necessary for clear vision because it provides a smooth refractive surface and acts as a protective barrier against pathogens and injury.
Pathophysiology of Limbal Stem Cell Deficit
LSCD occurs when the limbal stem cells become depleted or dysfunctional, making it impossible to maintain the corneal epithelium. This condition can result from a variety of causes.
- Genetic Disorders: Because of inherent abnormalities in the limbal stem cells, conditions such as aniridia, a congenital absence of the iris, are associated with LSCD.
- Chemical and Thermal Burns: Exposure to caustic substances or high temperatures can destroy the limbal stem cells and their niche, resulting in LSCD.
- Inflammatory Diseases: Chronic inflammatory conditions, including Stevens-Johnson syndrome, ocular cicatricial pemphigoid, and severe allergic conjunctivitis, can harm limbal stem cells and their microenvironment.
- Infections: Serious infections such as trachoma or herpes simplex keratitis can result in scarring and the loss of limbal stem cells.
- Iatrogenic Causes: Surgical procedures or long-term use of contact lenses can cause trauma to the limbal region, resulting in LSCD.
Clinical Features of Limbal Stem Cell Deficiency
Patients with LSCD typically present with a variety of symptoms and clinical signs, which vary in severity depending on the extent of the deficiency.
- Visual Disturbances: Blurred vision is a common symptom of corneal transparency loss and surface irregularities.
- Photophobia: As a result of corneal epithelial breakdown and inflammation, individuals may experience increased light sensitivity.
- Ocular Discomfort and Pain: Chronic irritation, burning, and pain are common symptoms of epithelial defects and inflammation.
- Recurrent Epithelial Defects: Non-healing epithelial defects or chronic corneal ulcers are common in LSCD.
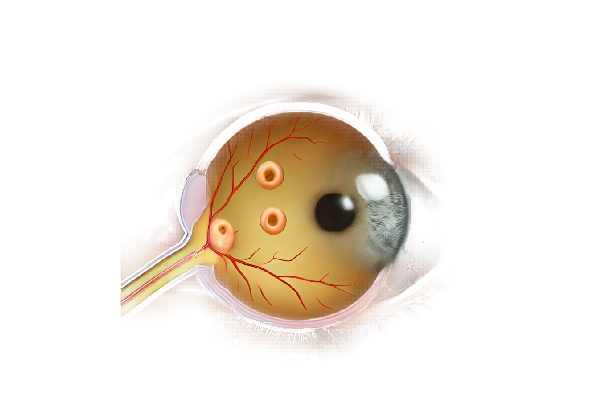
- Vascularization: Abnormal blood vessels grow into the cornea from the limbus, reducing corneal transparency and causing scarring.
- Conjunctivalization: The conjunctival epithelium replaces the corneal surface, making it less transparent and more susceptible to inflammation and scarring.
Causes of Limbal Stem Cell Deficiency
The pathogenesis of LSCD includes both intrinsic and extrinsic factors that disrupt the delicate balance required for the maintenance of limbal stem cells.
- Intrinsic Factors: Genetic mutations and systemic diseases can impair the production, proliferation, and survival of limbal stem cells.
- Extrinsic Factors: Environmental insults such as chemical injuries, infections, and chronic inflammation can all destroy limbal stem cells and their supporting niche.
Complications of Limbal Stem Cell Deficiency
If left untreated, LSCD can cause a number of serious complications:
- Corneal Scarring: Persistent epithelial defects and recurring inflammation can cause extensive scarring, resulting in permanent vision loss.
- Infection: A compromised epithelial barrier increases the risk of microbial infections, which can cause additional corneal damage and potentially lead to endophthalmitis, a severe intraocular infection.
- Glaucoma: Chronic inflammation and scarring can disrupt aqueous humor drainage, resulting in elevated intraocular pressure and glaucoma.
- Symblepharon Formation: Adhesions between the conjunctiva and the cornea or eyelid can form, limiting eye movement and causing additional discomfort.
Distinguishing LSCD from other corneal conditions
Accurate diagnosis of LSCD is critical because treatment differs significantly from other corneal pathologies. Differential diagnoses to consider are:
- Herpetic Keratitis: Herpetic keratitis is characterized by dendritic or geographic ulcers and can mimic some features of LSCD, but it usually responds to antiviral therapy.
- Keratoconjunctivitis Sicca (Dry Eye Syndrome): Although dry eye can cause similar symptoms such as discomfort and epithelial defects, it rarely results in the same level of vascularization and conjunctivalization as LSCD.
- Neurotrophic Keratopathy: This condition causes epithelial defects and ulcers but lacks the extensive limbal involvement and vascularization found in LSCD.
Diagnostic methods
Diagnosing limbal stem cell deficiency requires a multi-faceted approach that includes clinical evaluation, imaging techniques, and specialized tests to confirm the diagnosis and determine the extent of the deficiency.
Clinical Evaluation
- Patient History and Symptoms: A thorough patient history is required, with emphasis on symptoms such as chronic ocular discomfort, blurred vision, photophobia, and recurrent epithelial defects. Information about previous eye injuries, surgeries, infections, and systemic diseases is also required.
- Slit-Lamp Examination: This procedure allows for a thorough examination of the cornea and limbus. The key findings in LSCD are:
- Vascularization is the presence of blood vessels growing into the cornea from the limbus.
- Conjunctivalization: Replaces corneal epithelium with conjunctival epithelium, which is more opaque and vascular.
- Persistent Epithelial Defects: Areas of the cornea that do not heal or regenerate properly.
- Stromal Scarring: The corneal stroma opacifies and thickens as a result of chronic inflammation and healing.
Imaging Techniques
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT generates high-resolution cross-sections of the cornea and limbus. It can help identify epithelial disruption, limbal thinning, and vascularization.
- Confocal Microscopy: This technique allows for microscopic examination of the corneal layers in vivo, which aids in determining the density and health of limbal stem cells as well as detecting inflammatory cells or pathogens.
- Fluorescein Staining: Applying fluorescein dye to the ocular surface highlights epithelial defects and assesses corneal epithelial integrity.
Specialized Tests
- Impression Cytology: This test collects superficial epithelial cells from the corneal surface using a small cellulose acetate filter. The cells are then examined under a microscope to detect conjunctivalization and the presence of goblet cells, which are uncommon on the cornea.
- Limbal Stem Cell Marker Testing: Recent research has revealed specific markers for limbal stem cells. Immunohistochemistry and molecular testing can be used to detect these markers and determine the presence and health of limbal stem cells.
Differential Diagnosis
A thorough examination is required to distinguish LSCD from other corneal conditions that may present with similar symptoms. These conditions include the following:
- Herpetic Keratitis: Herpetic keratitis is characterized by dendritic or geographic ulcers and can mimic some features of LSCD, but it usually responds to antiviral therapy.
- Keratoconjunctivitis Sicca (Dry Eye Syndrome): Although dry eye can cause similar symptoms such as discomfort and epithelial defects, it rarely results in the same level of vascularization and conjunctivalization as LSCD.
- Neurotrophic Keratopathy: This condition causes epithelial defects and ulcers but lacks the extensive limbal involvement and vascularization found in LSCD.
Limbal Stem Cell Deficiency Treatment
Treatment for limbal stem cell deficiency (LSCD) entails symptom management, healing promotion, and corneal epithelium function restoration. The severity of the condition, the extent of the deficiency, and the underlying cause all influence treatment options.
Medical Management
- Anti-inflammatory Therapy: Topical corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs) are frequently used to reduce inflammation and prevent additional damage to the limbal stem cells. Chronic inflammation requires careful management to avoid complications.
- Lubrication and Tear Supplements: Preservative-free artificial tears and lubricating ointments help keep the cornea hydrated and the ocular surface protected. These are essential for managing symptoms and promoting epithelial healing.
- Autologous Serum Eye Drops: These drops are made from the patient’s own blood serum and contain growth factors and vitamins that aid in epithelial healing and inflammation reduction.
Surgical Treatments
- Limbal Stem Cell Transplantation: This is the primary treatment option for severe LSCD. The procedure entails transplanting healthy limbal stem cells from a donor or the patient’s other eye. There are several techniques, including:
- Conjunctival Limbal Autograft (CLAU): Taking limbal tissue from the patient’s healthy eye and transplanting it into the affected eye.
- Living-Related Conjunctival Limbal Allograft (lr-CLAL): Utilizes limbal tissue from a related donor.
- Kerato-Limbal Allograft (KLAL): Uses cadaveric donor tissue for transplantation.
- Amniotic Membrane Transplantation: This procedure involves applying a layer of amniotic membrane to the ocular surface to promote healing and provide a scaffold for epithelial development. The amniotic membrane has anti-inflammatory and anti-scarring properties, making it useful for treating LSCD.
- Simple Limbal Epithelial Transplantation (SLET): This relatively new technique involves taking a small biopsy of healthy limbal tissue, which is then divided into small pieces and distributed on an amniotic membrane placed over the affected area. This method stimulates stem cell growth and promotes healing.
Innovative and Emerging Therapies
- Cultivated Limbal Epithelial Cell Transplantation (CLET): This technique harvests and cultures limbal stem cells in a laboratory to increase their numbers. The cultured cells are then transplanted into the affected eye. This method is especially useful for bilateral LSCD with limited donor tissue.
- Induced Pluripotent Stem Cells (iPSCs): Researchers are investigating the use of iPSCs to generate limbal stem cells. iPSCs can be derived from the patient’s own cells, lowering the risk of rejection and potentially providing an endless supply of stem cells for transplantation.
- Gene Therapy: The use of gene therapy to correct genetic defects that cause LSCD is a developing field. This method attempts to restore the function of defective stem cells or protect them from immune-mediated damage.
- Nanotechnology: Another promising area of research is the development of nanoparticle-based drug delivery systems capable of providing therapeutic agents to the limbal region in a targeted and sustained manner. This technology has the potential to improve the efficacy of current treatments while also reducing side effects.
Post-operative Care
- Immunosuppressive Therapy: To prevent rejection of transplanted tissue, patients may require systemic immunosuppressive medications, particularly in allograft cases.
- Close Monitoring: Regular follow-up visits are critical for monitoring the healing process, detecting signs of rejection or infection, and adjusting treatment as necessary.
- Supportive Care: It is critical to continue using lubricants, anti-inflammatory medications, and other supportive therapies to ensure successful outcomes.
Effective Ways to Improve and Prevent Limbal Stem Cell Deficiency
- Protect Eyes from Trauma: Wear protective eyewear when participating in activities that pose a risk of eye injury, such as sports or hazardous work environments, to avoid limbal damage.
- Manage Systemic Diseases: Manage systemic diseases such as diabetes, autoimmune disorders, and infections, which can all contribute to LSCD.
- Avoid Long-Term Contact Lens Use: Prolonged use of contact lenses can result in microtrauma to the limbal area. To reduce the risk, maintain proper hygiene and replace your lenses as recommended.
- Early Treatment of Ocular Surface Diseases: Prompt treatment for conditions such as dry eye syndrome, allergic conjunctivitis, and infections can prevent complications that could lead to LSCD.
- Regular Eye Exams: Schedule routine eye exams to detect early signs of limbal stem cell damage and begin treatment promptly.
- Avoid Toxic Chemicals: Keep toxic chemicals out of your eyes, as they can cause burns and damage to the limbal stem cells.
- Healthy Lifestyle: Eat a well-balanced diet high in antioxidants and nutrients to improve overall eye health and possibly delay the onset of limbal stem cell damage.
- Educate on Symptoms: Be aware of the symptoms of LSCD, such as persistent eye discomfort, photophobia, and blurred vision, and seek immediate medical attention if they appear.
- Immunosuppressive Therapy Adherence: For patients undergoing stem cell transplantation, following the prescribed immunosuppressive therapy is critical to preventing graft rejection and ensuring successful outcomes.
Trusted Resources
Books
- “Corneal Stem Cell Biology, Basic Science and Clinical Application” by Noriko Koizumi, Julie T. Daniels, and Ryuhei Hayashi
- “Stem Cell Therapy for Degenerative Eye Disorders” by Norman Saunders
- “Cornea: Fundamentals, Diagnosis and Management” by Krachmer, Mannis, and Holland
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- International Society for Stem Cell Research (ISSCR) – isscr.org
- MedlinePlus – Limbal Stem Cell Deficiency – medlineplus.gov






