What is Lowe syndrome?
Lowe syndrome, also called oculocerebrorenal syndrome, is a rare genetic condition that affects the eyes, brain, and kidneys. Mutations in the OCRL gene on the X chromosome cause phosphatidylinositol 4,5-bisphosphate 5-phosphatase deficiency. This enzyme deficiency causes abnormal accumulation of certain substances in cells, which is characteristic of Lowe syndrome. The ocular manifestations are frequently the most visible and early signs of the syndrome, affecting patients’ vision and quality of life.
Understanding the Impact of Lowe Syndrome on Vision
Lowe syndrome causes a variety of ocular abnormalities that can impair vision from a young age. Understanding the disease’s pathophysiology, clinical presentation, and associated complications is critical for effective management.
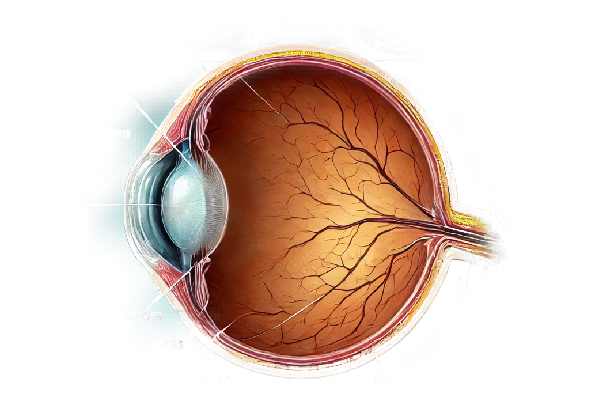
Pathophysiology Of Ocular Manifestations
Lowe syndrome’s primary ocular abnormalities are congenital cataracts, glaucoma, and corneal and conjunctival issues. The underlying pathophysiology is due to OCRL protein dysfunction, which regulates the actin cytoskeleton and vesicular trafficking. The absence or malfunction of this protein interferes with normal cellular functions, resulting in the development of these ocular abnormalities.
Congenital Cataracts
Congenital cataracts are the most common ocular manifestation of Lowe syndrome, occurring in almost all affected people. These cataracts are usually bilateral and appear at birth or within the first few months of life. The severity of cataracts varies, ranging from partial lens opacities to complete lens clouding, which can significantly impair vision. The exact mechanism by which the OCRL gene mutation causes cataract formation is unknown, but it is believed to involve abnormal cell signaling and lens fiber cell differentiation.
Glaucoma
Glaucoma is another common ocular manifestation of Lowe syndrome, affecting roughly 50% of patients. Glaucoma can develop in these patients for a variety of reasons, including abnormal anterior chamber angle development, increased intraocular pressure (IOP), and structural abnormalities in the trabecular meshwork. Glaucoma can develop at any age, but it typically appears in early childhood. If left untreated, it can cause progressive optic nerve damage and permanent vision loss.
Corneal and conjunctival abnormalities
Patients with Lowe syndrome may also have corneal and conjunctival abnormalities. These may include corneal opacities, keratopathy, and recurring corneal erosions. The conjunctiva may exhibit chronic inflammation, resulting in conjunctivitis. These conditions cause discomfort, photophobia, and increased visual impairment.
Retinal and Optic Nerve Changes
Lowe syndrome can also cause retinal and optic nerve abnormalities, though these are rarer. Some patients may develop pigmentary retinopathy, a condition in which pigment accumulates in the retina and causes progressive vision loss. Optic nerve hypoplasia, or an underdeveloped optic nerve, can also cause visual impairment.
Ocular motility disorders
Strabismus, or eye misalignment, is a common finding in Lowe syndrome patients. Muscle weakness or neurological factors can cause this condition, which frequently necessitates surgical intervention or corrective lenses to improve eye alignment and vision. Nystagmus, which is characterized by involuntary eye movements, can also occur and exacerbate the visual disturbances experienced by these patients.
Clinical Features and Symptoms
The clinical presentation of ocular manifestations in Lowe syndrome varies by individual. Common symptoms and signs are:
- Visual Impairment: The extent of cataracts, glaucoma, and other ocular abnormalities determines the severity of visual impairment. Patients may have poor visual tracking and responsiveness since infancy.
- Photophobia: Light sensitivity is common, especially in cases of corneal opacities and cataracts.
- Ocular Pain: Elevated IOP in glaucoma, recurrent corneal erosions, or chronic conjunctivitis can all cause pain.
- Tearing and Redness: Chronic irritation and inflammation can cause excessive tearing and conjunctival redness.
Differential Diagnosis
It is critical to distinguish the ocular manifestations of Lowe syndrome from other congenital and genetic disorders that present similarly. Conditions to consider are:
- Congenital Cataracts: While congenital cataracts can occur alone or in conjunction with other syndromes, the presence of renal and neurological abnormalities suggests Lowe syndrome.
- Primary Congenital Glaucoma: Although the symptoms are similar to Lowe syndrome, the systemic manifestations and genetic background differ significantly.
- Other Metabolic Disorders: Cataracts can be associated with disorders such as galactosemia and hypocalcemia, which must be differentiated using appropriate biochemical and genetic tests.
Effects on Quality of Life
The ocular manifestations of Lowe syndrome have a significant impact on patients’ quality of life. Early-onset visual impairment can impede normal visual development, compromising motor skills, cognitive development, and educational attainment. The chronic nature of the ocular conditions, frequent medical visits, and potential surgical interventions all add to the physical and emotional strain on patients and their families.
Diagnostic methods
The ocular manifestations of Lowe syndrome require a multifaceted approach that includes clinical evaluation, imaging techniques, and specialized tests.
Clinical Evaluation
- Patient History and Symptoms: A detailed patient history is required, with emphasis on the onset and progression of visual symptoms, a family history of genetic disorders, and any associated systemic symptoms such as renal or neurological issues.
- Slit-Lamp Examination: This is an important tool for detecting congenital cataracts and other anterior segment abnormalities. It provides detailed views of the cornea, anterior chamber, lens, and iris.
- Tonometry: Measuring intraocular pressure (IOP) is critical for diagnosing glaucoma. Elevated IOP may indicate the presence of glaucoma, necessitating further evaluation and treatment.
Imaging Techniques
- Optical Coherence Tomography (OCT): OCT uses high-resolution cross-sectional images of the retina and optic nerve to detect retinal changes, optic nerve hypoplasia, and other structural abnormalities.
- Ultrasound Biomicroscopy (UBM): This imaging technique provides detailed images of anterior segment structures, such as the angle and ciliary body, which aids in the diagnosis of glaucoma and anterior segment dysgenesis.
- Fundus Photography: Fundus photography produces detailed images of the retina, allowing for the detection and documentation of retinal abnormalities like pigmentary retinopathy.
Specialized Tests
- Electroretinography (ERG): ERG measures the retina’s electrical responses to light stimuli, which helps assess retinal function and detect conditions such as retinopathy.
- Genetic Testing: To confirm the diagnosis of Lowe syndrome, genetic testing to identify mutations in the OCRL gene is usually required. This is critical for a conclusive diagnosis and genetic counseling.
- Visual Field Testing: Examining the visual field can help determine the extent of vision loss and the effect of glaucoma or other retinal abnormalities on peripheral vision.
Lowe Syndrome Ocular Manifestations Treatment
Treating Lowe syndrome’s ocular manifestations requires a multidisciplinary approach that addresses each individual condition in order to preserve and improve vision. Treatment plans are custom-made for each patient and may include both medical and surgical interventions.
Medical Management
- Anti-inflammatory and Lubricant Eye Drops: These are often prescribed to treat chronic inflammation and irritation. Lubricating drops relieve dry eye symptoms, whereas anti-inflammatory drops reduce inflammation caused by conjunctivitis and corneal issues.
- Glaucoma Medications: To lower intraocular pressure (IOP), patients with glaucoma use topical medications such as beta-blockers, prostaglandin analogs, alpha agonists, and carbonic anhydrase inhibitors. These medications help to prevent optic nerve damage and preserve vision.
- Antibiotic Drops: Antibiotic eye drops may be prescribed to treat recurring infections or to prevent infection after surgical procedures.
Surgical Interventions
- Cataract Surgery: The primary treatment for congenital cataracts is surgically removing the cloudy lens and, in many cases, implanting an intraocular lens (IOL). Early intervention is critical for preventing amblyopia and promoting healthy visual development. However, given the high risk of complications in Lowe syndrome, surgical timing and technique must be carefully considered.
- Glaucoma Surgery: If medical treatment fails to control IOP, surgical options such as trabeculectomy, goniotomy, or implantation of drainage devices (e.g., shunts or stents) may be required. These procedures aim to increase aqueous humor outflow and lower IOP.
- Corneal Surgery: To improve vision and comfort, patients with significant corneal opacities or recurring erosions may benefit from surgical interventions such as corneal transplantation (penetrating keratoplasty) or surface procedures (phototherapeutic keratectomy).
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy for Lowe syndrome is currently underway, with the goal of correcting the underlying genetic defect in the OCRL gene. Although still experimental, gene therapy shows promise in treating the underlying cause of the condition and preventing its ocular manifestations.
- Stem Cell Therapy: Advances in stem cell research show promise for regenerating damaged ocular tissues. Stem cell therapy has the potential to open up new treatment options for Lowe syndrome cornea and retina repair.
- New Drug Developments: Ongoing research seeks to create new medications that target specific pathways involved in Lowe syndrome. These medications may provide more effective treatment of the condition’s ocular and systemic symptoms.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS techniques, which involve smaller incisions and less trauma to ocular tissues, are being investigated for patients with Lowe syndrome. These procedures can provide effective IOP control with fewer complications and a shorter recovery time.
Post-operative Care
Postoperative care is critical for ensuring successful outcomes after ocular surgery.
- Anti-inflammatory and Antibiotic Drops: Using these drops regularly helps to manage inflammation and prevent infection during the healing process.
- Close Monitoring: Regular follow-up visits are required to monitor healing, identify complications early on, and adjust treatment as needed.
- Supportive Therapies: Lubricating drops and other supportive measures can help keep the eyes comfortable and healthy after surgery.
To optimize visual outcomes and improve quality of life for affected individuals, effective management of Lowe syndrome’s ocular manifestations necessitates a combination of medical and surgical treatments, ongoing research into innovative therapies, and meticulous postoperative care.
Effective Strategies for Improving and Avoiding Lowe Syndrome Ocular Manifestations
- Early Diagnosis and Intervention: Early detection and treatment of ocular issues can reduce complications and improve outcomes. Regular eye examinations beginning in infancy are essential.
- Regular Monitoring: Patients with Lowe syndrome should have regular follow-up appointments with an ophthalmologist to watch for the development of cataracts, glaucoma, and other ocular conditions.
- Medication Adherence: Strict adherence to prescribed glaucoma medications and other eye drops is critical for controlling IOP and avoiding optic nerve damage.
- Protective Eyewear: Wear protective eyewear when participating in activities that may result in eye injury to avoid trauma and subsequent ocular complications.
- Maintain Good Hygiene: Keeping your eyes clean and not rubbing them can help prevent infections and irritation.
- Manage Systemic Health: Managing systemic conditions, such as kidney issues associated with Lowe syndrome, can help to reduce the disease’s overall burden and promote better eye health.
- Nutritional Support: Eat a diet high in antioxidants and essential nutrients to promote overall eye health. Specific deficiencies may necessitate the use of supplements.
- Educate on Symptoms: Patients and caregivers should be informed about the symptoms of cataracts, glaucoma, and other eye problems in order to seek prompt medical attention if they occur.
- Innovative Therapies: Stay up to date on emerging treatments and, if appropriate, enroll in clinical trials to gain access to potential new therapies that may improve condition management.
Trusted Resources
Books
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright and Peter H. Spiegel
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Laura Ensign Grillo
- “Genetics for Ophthalmologists: The Molecular Genetic Basis of Ophthalmic Disorders” by Graeme C. M. Black
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- Ophthalmology Times – ophthalmologytimes.com
- Lowe Syndrome Association – lowesyndrome.org






