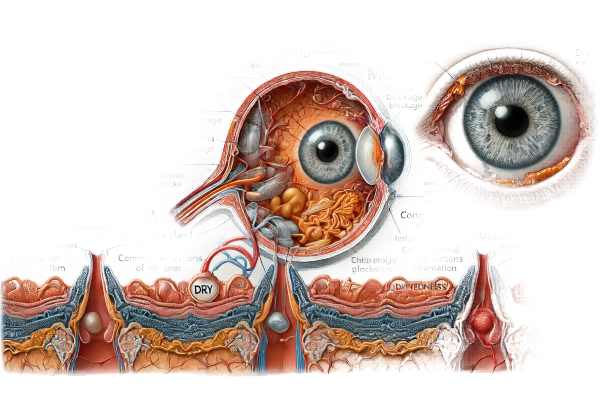
What is the Meibomian Gland Dysfunction?
Meibomian gland dysfunction (MGD) is a common ocular condition characterized by the obstruction or irregular secretion of the meibomian glands, which are required to maintain a healthy tear film. These glands in the eyelids secrete oils that prevent the tear film from evaporating. When these glands do not function properly, it can cause dry eye syndrome, irritation, and inflammation. MGD is a major contributor to evaporative dry eye disease and can have a significant impact on a person’s quality of life due to the discomfort and visual disturbances it produces.
Detailed Investigation of Meibomian Gland Dysfunction
Meibomian gland dysfunction (MGD) is a complicated and multifaceted condition that affects ocular surface health. To understand MGD, one must first understand the anatomy and function of the meibomian glands, as well as the pathophysiology of the dysfunction, risk factors, prevalence, and clinical manifestations.
Anatomy and Function of the Meibomian Glands
The meibomian glands are sebaceous glands that reside within the eyelids’ tarsal plates. Each eyelid contains 25 to 40 meibomian glands, whose primary function is to secrete lipids into the tear film. These lipids make up the tear film’s outermost layer, known as the lipid layer, which reduces tear evaporation and keeps the film stable. Lipids reach the ocular surface via tiny ducts that open at the eyelid margin, just behind the eyelashes.
The meibomian glands are hormonally and neurally controlled. Androgens, in particular, play an important role in controlling lipid production. Normal meibomian gland function is critical to ocular surface health because a stable tear film is required for clear vision and comfort.
Pathogenesis of Meibomian Gland Dysfunction
MGD develops when the meibomian glands become obstructed or produce abnormal secretions. Changes in glandular structure, inflammation, and hormonal imbalances can all contribute to this condition. MGD has two types of pathophysiology: obstructive MGD and hypersecretory MGD.
Obstructive MGD
The most common type of MGD is obstructive MGD, which is distinguished by meibomian gland duct blockages. Several mechanisms may contribute to this obstruction:
- Hyperkeratinization: Excessive keratinization can clog gland ducts, preventing lipid flow. This is frequently associated with conditions such as acne rosacea.
- Gland Atrophy: Over time, the meibomian glands may undergo structural changes, including atrophy, limiting their ability to produce and secrete lipids.
- Inflammation: Prolonged inflammation of the eyelid margin (blepharitis) can result in gland obstruction and subsequent dysfunction.
- Microbial Overgrowth: Bacterial colonization of the eyelid margin can worsen inflammation and clog the gland ducts.
Hypersecretory MGD
Hypersecretory MGD is less common and is defined by excessive lipid production. While the glands are not obstructed, the quality of the secreted lipids may be compromised, resulting in an unstable tear film.
Risk Factors for Meibomian Gland Dysfunction
There are several risk factors for MGD, such as:
- Age: The prevalence of MGD rises with age, as gland function declines over time.
- Hormonal Changes: Hormonal imbalances, particularly a decrease in androgens, can lead to MGD. This explains why the condition is more common in postmenopausal women.
- Systemic Diseases: Diabetes, acne rosacea, and autoimmune diseases (e.g., Sjögren’s syndrome) are all associated with an increased risk of MGD.
- Environmental Factors: Prolonged exposure to environmental stressors like low humidity, wind, and air pollution can worsen MGD symptoms.
- Contact Lens Wear: Long-term contact lens use has been associated with changes in meibomian gland function and morphology.
Clinical Features of Meibomian Gland Dysfunction
MGD can cause a wide range of symptoms and signs, which vary in severity. The primary clinical manifestations are:
- Dry Eye Symptoms: Patients with MGD frequently complain of dry eyes, including a gritty or sandy sensation, burning, itching, and fluctuating vision. These symptoms result from increased tear evaporation and tear film instability.
- Eyelid Changes: Examining the eyelids may reveal signs of inflammation, such as redness, swelling, and crusting along the margins. Common findings include thickened or irregular eyelid margins, as well as plugged gland orifices.
- Tear Film Abnormalities: The tear film in MGD patients is usually unstable, resulting in a short tear break-up time (TBUT). This instability may cause temporary visual disturbances and discomfort.
- Ocular Surface Damage: Chronic MGD can damage the ocular surface epithelium, causing punctate epithelial erosions, filamentary keratitis, and, in severe cases, corneal ulceration.
- Pain and Discomfort: MGD-related inflammation and irritation can cause significant pain and discomfort, reducing the patient’s quality of life.
Prevalence and Impact
MGD is a very common condition, with studies indicating that it affects a large proportion of the population. According to estimates, MGD affects up to 70% of people with dry eye disease. The condition can affect people of any age, but it is most common in older adults.
MGD can have a significant impact on overall quality of life. Patients frequently report chronic discomfort, visual disturbances, and a reduced ability to perform daily tasks such as reading, using digital devices, and driving. MGD imposes a significant economic burden because it increases healthcare utilization and associated costs.
Diagnostic methods
Meibomian gland dysfunction (MGD) is diagnosed using a combination of clinical examination, patient history, and specialized diagnostic tests. Early and accurate diagnosis is critical for successful management and prevention of long-term complications. Here, we look at the various diagnostic methods used to identify MGD.
Clinical Examination
A thorough clinical examination is the foundation for MGD diagnosis. This involves a thorough examination of the eyelids, meibomian glands, and tear film. The key components of the clinical examination are:
- Eyelid Examination: The clinician examines the eyelid margins for inflammation, redness, swelling, and abnormalities like telangiectasia (small dilated blood vessels). Crusting, irregularities, and blocked gland orifices are also visible.
- Meibomian Gland Expression: The function of the meibomian glands is evaluated by gently pressing the eyelid to release gland secretions. The quality and quantity of expressed lipids are important diagnostic indicators. Normal secretions are clear and fluid, whereas altered secretions can be thick, turbid, or absent.
- Slit-Lamp Biomicroscopy: This instrument enables a thorough examination of the eyelids, conjunctiva, and cornea. It aids in the detection of inflammation, gland dropout, and other ocular surface abnormalities.
Specialized Diagnostic Tests
In addition to the clinical examination, several specialized diagnostic tests can help diagnose MGD:
- Meibography: Meibography is an imaging technique that allows for a detailed view of the meibomian glands. Infrared light is used to examine the gland structure and detect abnormalities like gland dropout or atrophy. Meibography can be done with a variety of equipment, including slit-lamp mounted systems and dedicated meibography instruments.
- Tear Film Break-Up Time (TBUT): TBUT assesses the stability of the tear film. A fluorescein dye is introduced into the eye, and the time it takes for dry spots to appear on the corneal surface is recorded. A lower TBUT suggests tear film instability, which is common in MGD.
- Osmolarity Testing: Tear film osmolarity tests determine the concentration of solutes in the tear film. Elevated osmolarity indicates tear film instability and inflammation, which is common in MGD and dry eye disease.
- Lipid Layer Thickness Measurement: Devices such as the LipiView II ocular surface interferometer can measure the tear film’s lipid layer. This non-invasive test provides quantitative information on lipid layer health, which is critical for diagnosing and managing MGD.
- Meibomian Gland Evaluators: Handheld devices like the Korb Meibomian Gland Evaluator can apply standardized pressure to the eyelid, allowing for consistent assessment of gland function during clinical examination.
Patient History and Symptom Assessment
A thorough patient history and symptom evaluation are critical components of MGD diagnosis. Clinicians should ask about:
- Dry Eye Symptoms: Inquire about the presence, frequency, and severity of dry eye symptoms, such as dryness, burning, itching, foreign body sensation, and visual disturbances.
- Lifestyle and Environmental Factors: Details about the patient’s lifestyle, occupation, and environmental exposures can help identify potential risk factors for MGD. This includes prolonged screen time, contact lens wear, and exposure to dry or windy weather.
- Medical and Ocular History: A comprehensive medical and ocular history helps identify underlying conditions that may contribute.
Meibomian Gland Dysfunction Treatment
Treatment for Meibomian gland dysfunction (MGD) aims to reduce symptoms, restore normal gland function, and improve patients’ quality of life. A multifaceted approach, often involving a variety of therapies, is usually required. Below, we look at different treatment options and highlight innovative and emerging therapies.
Conventional Treatment Alternatives
- Warm Compresses: Applying warm compresses to the eyelids helps to melt the thickened secretions within the meibomian glands, making them easier to express. Using commercially available heat masks or warm washcloths, you can perform this simple and effective treatment at home.
- Lid Hygiene: Good eyelid hygiene is essential for managing MGD. Patients should clean their eyelid margins daily with lid scrubs or commercially available eyelid cleansers to remove debris and reduce bacterial load.
- Manual Expression: An eye care professional can perform in-office manual expression of the meibomian glands to clear blockages and improve gland function. This procedure entails applying pressure to the eyelids to release the gland contents.
- Artificial Tears: Lubricating eye drops, particularly those with lipid layer enhancement, can provide symptomatic relief by stabilizing the tear film and reducing evaporation.
- Anti-inflammatory Medication: Topical or oral anti-inflammatory medications, such as corticosteroids or doxycycline, may be used to reduce inflammation and improve gland function. These medications help to reduce inflammation and bacterial growth along the eyelid margin.
Innovative and Emerging Therapies
- LipiFlow® Thermal Pulsation: LipiFlow is an FDA-approved device that uses heat and gentle pressure on the eyelids to effectively clear blocked meibomian glands. This in-office procedure has demonstrated promising results in terms of gland function and symptom reduction.
- Intense Pulsed Light (IPL) Therapy: Originally used in dermatology, IPL therapy has been modified to treat MGD. IPL uses light pulses to target and reduce inflammation, improve meibomian gland function, and reduce bacterial loads on the eyelids.
- MiBo Thermoflo: This device uses continuous thermal energy to liquefy thickened gland secretions, making them easier to express. It offers a comfortable in-office treatment option for MGD patients.
- Omega-3 Fatty Acid Supplements: Studies have shown that taking omega-3 fatty acids orally can help improve meibomian gland function and reduce inflammation. These supplements can be an effective addition to other MGD treatments.
- Cyclosporine A (Restasis®) and Lifitegrast (Xiidra®): These prescription eye drops are primarily used to treat dry eyes, but they can also help MGD patients by reducing ocular surface inflammation and improving tear film stability.
Future Directions
Ongoing research is investigating novel therapeutic approaches for MGD. Future treatments could include gene therapy to address underlying genetic factors, regenerative medicine techniques to regenerate glandular tissue, and the development of new pharmacological agents that target specific pathways involved in gland dysfunction.
Effective Ways to Improve and Prevent Meibomian Gland Dysfunction
- Maintain Daily Lid Hygiene: Use a gentle lid scrub or commercially available eyelid cleanser to remove debris and reduce bacterial load.
- Use Warm Compresses: Apply warm compresses to your eyelids for 5-10 minutes daily to help melt and expel thickened gland secretions.
- Stay Hydrated: Drink plenty of water to stay hydrated and promote healthy tear production and gland function.
- Maintain a Healthy Diet: Consume omega-3 fatty acids from fish, flaxseeds, and walnuts, or consider supplementation to reduce inflammation and support gland function.
- Limit Screen Time: Take frequent breaks during prolonged screen use to reduce eye strain and encourage blinking, which helps spread the tear film evenly across the eye.
- Protect Your Eyes: Wear sunglasses to protect your eyes from wind, dust, and UV rays, which can worsen MGD symptoms.
- Avoid Contact Lens Overuse: To reduce stress on your meibomian glands, follow the recommended contact lens wear and care guidelines.
- Quit Smoking: Smoking can exacerbate MGD symptoms and harm overall eye health. Seek help to quit smoking if necessary.
- Manage Underlying Conditions: If you have systemic conditions such as acne, rosacea, or diabetes, consult with your doctor to effectively manage them, as they can contribute to MGD.
- Regular Eye Exams: Schedule regular eye exams with your optometrist or ophthalmologist to monitor meibomian gland function and receive appropriate treatment.
Trusted Resources
Books
- “The Dry Eye Remedy” by Robert Latkany
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
- “The MGD Book: A Guide to Meibomian Gland Dysfunction and Treatment” by Dr. Sandra Cremers






