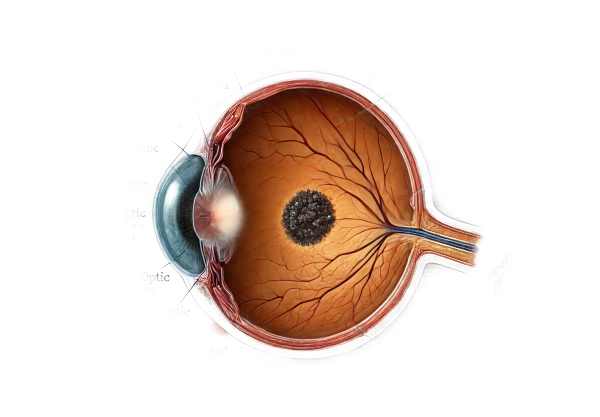
What is Melanocytoma of the Optic Disc?
Melanocytoma of the optic disc is a rare, benign pigmented tumor that develops near the optic nerve head. These tumors are typically dark brown to black in color due to their high melanin content and are made up of melanocytes. Although melanocytomas are usually asymptomatic, they can occasionally cause visual disturbances, especially if they compress adjacent structures or undergo malignant transformation. These tumors are usually discovered by chance during routine eye exams, but they require close monitoring to detect any changes that could indicate complications.
Detailed Examination of Melanocytoma of the Optic Disc
Melanocytoma of the optic disc is an intriguing and important condition in the field of ophthalmology because of its distinct characteristics and potential implications for ocular health. Understanding this condition necessitates a thorough examination of its causes, clinical manifestations, associated risks, and implications for visual function.
Origin and Pathophysiology
Melanocytomas develop from melanocytes, which are cells that produce melanin, the pigment that gives color to the skin, hair, and eyes. The uvea, sclera, and optic nerve are typically home to these melanocytes. Melanocytoma occurs when these cells form a benign tumor at the optic disc, which is where the optic nerve enters the eye.
The tumor itself is made up of densely pigmented, round to oval cells. Histologically, these cells are distinguished by numerous melanin granules, which give the tumor its distinct dark appearance. The presence of such a pigmented lesion on the optic disc can occasionally be mistaken for other pigmented ocular conditions, emphasizing the importance of accurate diagnosis.
Clinical Presentation
Melanocytomas are most commonly discovered during routine eye exams, as many patients are asymptomatic. However, when symptoms appear, they can include:
- Visual Disturbances: Although uncommon, patients may experience visual disturbances if the tumor compresses nearby structures or obstructs the flow of nutrients through the optic nerve. This can cause visual field defects, reduced visual acuity, or even a relative afferent pupillary defect (RAPD).
- Floaters: Some patients have reported seeing floaters, which are shadows cast on the retina by the tumor or associated cellular debris.
- Color Vision Changes: In rare cases, changes in color vision may occur if the tumor affects the optic nerve fibers responsible for color perception.
- Secondary Complications: Melanocytomas can occasionally cause secondary complications such as central retinal vein occlusion (CRVO) or peripapillary choroidal neovascularization, which can impair vision even more.
Differential Diagnosis
Differentiating melanocytoma of the optic disc from other pigmented lesions is essential. Conditions that may resemble melanocytoma include:
- Choroidal Nevus: These are benign pigmented lesions that form in the choroid and can spread to the optic disc.
- Choroidal Melanoma: A malignant tumor that can present similarly but is typically more aggressive and causes more severe symptoms.
- Pigmented Retinal Epithelium: Hyperplasia or hypertrophy of the retinal pigment epithelium can resemble melanocytoma, but it lacks the location-specific features of optic disc melanocytomas.
Associated Risks
While melanocytomas are generally benign and slow-growing, there are a number of associated risks and potential complications that require regular monitoring:
- Malignant Transformation: Although rare, there is a risk of malignant transformation into melanoma. This low risk necessitates regular ophthalmologic evaluations.
- Optic Nerve Compression: Significant tumor growth can cause compression of the optic nerve fibers, resulting in visual field loss and other optic neuropathy.
- Vascular Complications: The presence of a melanocytoma can result in vascular complications such as CRVO, which can severely impair vision.
Epidemiology
Melanocytomas are uncommon, and there is no clear gender or racial preference. They can occur at any age, but are most commonly diagnosed in middle-aged and older adults. Because these tumors are benign, many people may live with the condition for years without experiencing any noticeable symptoms.
Pathophysiological Mechanisms
The exact mechanisms that drive the development of melanocytoma are unknown. However, it is believed that genetic and environmental factors may play a role. The high melanin content of these tumors is a distinguishing feature, contributing to their dark appearance under ophthalmoscopic examination.
Impact on Visual Function
A melanocytoma’s impact on visual function is largely determined by its size, location, and any secondary effects that may occur. Most tumors remain stable and do not significantly impair vision. However, if the tumor grows or causes complications, visual function may be impaired.
- Visual Field Defects: Compression of optic nerve fibers can cause localized visual field defects. Perimetry testing is commonly used to detect these defects during a comprehensive eye exam.
- Visual Acuity: If the tumor affects the central optic nerve fibers, visual acuity may decrease. This is more likely if secondary complications like CRVO or neovascularization develop.
- Color Vision: Although less common, changes in color vision may occur if the tumor affects the optic nerve fibers responsible for color differentiation.
Long-term prognosis
Individuals with optic disc melanocytoma typically have a good long-term prognosis. Most tumors are benign and have no significant effect on visual function. Regular monitoring is required to detect changes that could indicate complications or malignant transformation.
Diagnostic methods
The diagnosis of optic disc melanocytoma requires a combination of clinical examination, imaging studies, and, in some cases, histopathological evaluation. Early and accurate diagnosis is critical for effective treatment and monitoring of potential complications. In this section, we will look at the various diagnostic methods for detecting optic disc melanocytomas.
Clinical Examination
The first step in diagnosing melanocytoma is to have an ophthalmologist perform a thorough clinical examination. The key components of the examination are:
- Ophthalmoscopy: Direct and indirect ophthalmoscopy enable clinicians to visualize the optic disc and detect the presence of a pigmented lesion. Melanocytoma is identified by the tumor’s characteristic dark brown to black coloration and location on the optic disc.
- Slit-Lamp Biomicroscopy: This technique allows for a detailed view of the anterior and posterior segments of the eye. When combined with a contact lens or a 90-diopter lens, it enables a more detailed examination of the optic disc and surrounding structures.
Imaging Studies
Imaging studies play an important role in confirming the diagnosis and assessing the characteristics of the tumor.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve head. It aids in determining the thickness and extent of the tumor, as well as any accompanying retinal changes such as edema or atrophy.
- Fundus Photography: Color fundus photography can produce detailed images of the optic disc and tumor. These images can be used to document the lesion’s appearance over time and track any changes.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and taking pictures as it travels through the retinal vessels. It aids in detecting vascular abnormalities associated with the tumor, such as neovascularization or leakage.
- Ultrasound: B-scan ultrasonography can be used to determine the size and spread of the tumor. It is especially useful when the tumor is not visible under ophthalmoscopy due to media opacities.
Histopathologic Evaluation
In rare cases where the diagnosis is uncertain or there is a suspicion of malignant transformation, a biopsy and histopathological examination may be required. This entails extracting a tissue sample from the tumor and examining it under a microscope to confirm the presence of melanocytes and look for signs of cancer.
Differential Diagnosis
The accurate diagnosis of melanocytoma requires distinguishing it from other pigmented lesions of the optic disc. This includes:
- Choroidal Nevus: To distinguish a melanocytoma from a choroidal nevus, examine the location and characteristics of the lesion. Choroidal nevi are typically found within the choroid and can spread to the optic disc, whereas melanocytomas are primarily found on the optic disc.
- Choroidal Melanoma: A potentially fatal condition distinct from melanocytoma. Choroidal melanomas frequently exhibit more aggressive characteristics, such as progressive growth, elevated lesions, and more severe symptoms.
- Optic Disc Drusen: Calcified deposits on the optic disc that resemble melanocytomas. Imaging tests, such as OCT and ultrasound, can help distinguish between the two conditions.
Melanocytoma of the Optic Disc Treatment
Given its benign nature, melanocytoma of the optic disc usually requires careful monitoring rather than immediate intervention. However, treatment may be required if complications develop or there is a suspicion of malignant transformation.
Conservative Management
- Observation and Regular Monitoring: The primary approach to managing optic disc melanocytoma is to observe it regularly. Patients should have regular eye exams, including ophthalmoscopy and imaging studies such as OCT and fundus photography, to check for changes in the size or characteristics of the tumor. This is critical for detecting any early signs of malignant transformation or secondary complications.
- Patient Education: It is critical to educate patients about the nature of their condition and the importance of regular follow-up visits. Patients should be informed of any symptoms that may indicate complications, such as sudden changes in vision, increased floaters, or eye pain, and advised to seek immediate medical attention if they occur.
Surgical and Laser Interventions
- Excisional Biopsy: When there is significant uncertainty about the diagnosis or a high suspicion of malignant transformation, an excisional biopsy may be done. This entails the surgical removal of the tumor for histopathological examination. This procedure is typically reserved for cases in which the benefits of receiving a definitive diagnosis outweigh the risks of surgery.
- Laser Photocoagulation: Laser photocoagulation may be considered in cases where the tumor causes secondary complications such as peripapillary choroidal neovascularisation. This procedure uses laser energy to cauterize abnormal blood vessels, preventing further leakage or bleeding.
Innovative and Emerging Therapies
- Photodynamic Therapy (PDT): Photodynamic therapy, which is commonly used for choroidal neovascularization, is being investigated as a possible treatment for melanocytoma-related complications. PDT uses a light-activated photosensitizing agent to selectively target and destroy abnormal tissue.
- Targeted Molecular Therapy: Current research is looking into targeted molecular therapies that may inhibit pathways involved in tumor growth and progression. These therapies aim to provide a more precise and minimally invasive approach to treating melanocytomas, particularly those that show signs of malignancy.
- Genetic and Biomarker Research: Progress in genetic and biomarker research is improving our understanding of melanocytoma pathogenesis. Identifying specific genetic mutations and biomarkers associated with malignant transformation can help with early detection and personalized treatment options.
Managing Complications
- Treatment of Vascular Complications: If a melanocytoma causes vascular complications like central retinal vein occlusion (CRVO), additional treatments may be necessary. These may include anti-VEGF (vascular endothelial growth factor) injections to reduce macular edema and improve visual outcomes.
- Addressing Visual Impairments: Patients with significant visual impairments caused by the tumor or its complications may benefit from low vision aids and rehabilitation services. These can help maximize the patient’s remaining vision and improve their quality of life.
Overall, treating optic disc melanocytoma necessitates a personalized approach based on the patient’s condition, risk factors, and the presence of any complications. Regular monitoring and a proactive response to emerging symptoms are critical to achieving positive outcomes.
Effective Methods to Improve and Avoid Melanocytoma of the Optic Disc
- Regular Eye Exams: Seek routine comprehensive eye exams from an ophthalmologist to detect any early signs of melanocytoma or other ocular conditions. Early detection and monitoring are critical for successfully managing this condition.
- Maintain General Eye Health: Live a healthy lifestyle to benefit your overall eye health. This includes eating a well-balanced diet high in antioxidants and omega-3 fatty acids, which help to maintain healthy retinal and optic nerve function.
- Protect Your Eyes from UV Radiation: When outdoors, wear sunglasses that completely block UV rays. UV radiation can cause a variety of eye conditions, so protection is important for overall ocular health.
- Monitor for Symptoms: Be aware of any changes in your vision, such as the appearance of floaters, flashes of light, or sudden visual field changes. Please notify your eye care provider as soon as you notice these symptoms.
- Avoid Smoking: Smoking increases the risk of many eye diseases, including melanocytoma complications. Quitting smoking can improve overall health while lowering the risk of ocular complications.
- Manage Underlying Health Conditions: Keep systemic conditions like hypertension and diabetes under control, as they can have an impact on eye health. Proper management of these conditions can lower the risk of secondary complications from melanocytoma.
- Educate Yourself: Learn about melanocytoma and its possible implications. Knowing more about the condition can help you make better decisions about your eye health and follow your doctor’s recommendations more effectively.
- Genetic Counseling: If you have a family history of ocular conditions or melanocytoma, seek genetic counseling. Understanding your genetic risk can aid in early detection and prevention efforts.
- Follow Medical Advice: Stick to the treatment and follow-up schedules recommended by your healthcare provider. To effectively manage melanocytoma, it is necessary to monitor it consistently and follow medical advice.
Trusted Resources
Books
- “Clinical Ophthalmic Oncology: Uveal Tumors” by Arun D. Singh and Bertil E. Damato
- “Ocular Pathology” by Myron Yanoff and Joseph W. Sassani
- “Spencer’s Pathology of the Eye” by Alan C. Bird and W.R. Lee






