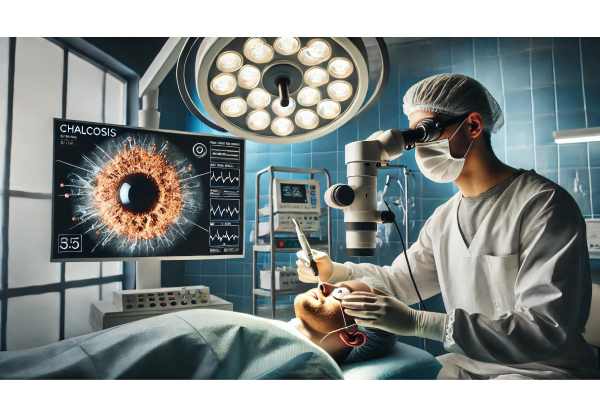
Chalcosis is a rare yet significant ophthalmic condition caused by the deposition of copper or copper-containing foreign bodies within the eye, typically after trauma or accidental introduction. This chronic exposure to copper ions can result in distinctive ocular changes, including corneal discoloration, lens opacities, and retinal damage, which may threaten vision if not identified and managed promptly. Early recognition and intervention are essential for preserving eye health and function. In this comprehensive guide, we’ll explore the underlying mechanisms, established and advanced therapies, surgical solutions, and the most recent innovations shaping chalcosis management today.
Table of Contents
- Defining Chalcosis: Epidemiology and Risk Factors
- Non-Surgical and Medical Approaches for Initial Management
- Operative Procedures and Minimally Invasive Techniques
- Next-Generation Treatments and Technology Advances
- Ongoing Research, Clinical Trials, and Future Outlook
- Frequently Asked Questions
Defining Chalcosis: Epidemiology and Risk Factors
Chalcosis refers to a chronic, toxic reaction caused by intraocular copper or copper-alloy foreign bodies. The term “chalcosis bulbi” is used when copper deposits trigger characteristic structural and functional changes within the eye. Unlike acute copper toxicity (as seen in copper sulfate injuries), chalcosis evolves slowly and often follows occupational or accidental trauma, particularly involving wire, machinery, or metallic fragments.
Key Features and Pathophysiology
- Copper ions slowly leach from the foreign body, depositing in ocular tissues such as the cornea (producing a greenish Kayser-Fleischer ring), lens (sunflower cataract), and retina.
- Toxicity develops over months to years, often presenting subtly before noticeable vision loss or discomfort.
Epidemiology
- Rare in the general population, with higher incidence among metal workers, mechanics, or individuals with occupational hazards.
- More common in young to middle-aged males, reflecting greater risk of work-related eye injuries.
Risk Factors
- Penetrating eye trauma with retention of copper-based foreign bodies.
- Lack of eye protection during industrial, agricultural, or construction activities.
- Delayed medical attention following ocular injury.
Clinical Signs
- Hazy vision, colored halos, or gradual vision decline.
- Copper-induced corneal and lens changes, sometimes visible to the naked eye.
- Secondary complications like uveitis or retinal degeneration in advanced cases.
Practical Advice:
Always seek immediate ophthalmic evaluation after any metallic eye injury. Even if initial symptoms are minor, long-term exposure to copper can lead to irreversible damage.
Non-Surgical and Medical Approaches for Initial Management
While definitive management of chalcosis usually requires surgical intervention, early non-surgical strategies play a key role in minimizing toxicity and protecting vision.
Immediate Steps After Injury
- Prompt Assessment:
Seek emergency care for all cases of suspected intraocular foreign bodies. A thorough eye examination, including slit-lamp and imaging (X-ray, CT, or ultrasound), is crucial to localize and characterize the object. - Avoid Eye Manipulation:
Do not attempt to remove embedded metal or rinse the eye without professional guidance, as this can worsen injury or disperse toxins.
Medical Therapies
- Antibiotic Prophylaxis:
Topical and systemic antibiotics reduce the risk of secondary infection (endophthalmitis), which can complicate penetrating injuries. - Steroid Use:
Short courses of topical or systemic corticosteroids may be prescribed to control inflammation, though these are adjuncts rather than definitive treatments. - Chelation Therapy:
Systemic copper chelators (such as penicillamine) have a limited role in ocular chalcosis but may be considered if systemic copper toxicity is suspected. Their direct efficacy in reversing ocular findings is not well-established.
Vision Support and Symptom Management
- Artificial Tears and Lubricants:
Used to relieve ocular surface irritation or dryness caused by corneal changes. - Regular Monitoring:
Frequent follow-up examinations to monitor the progression of deposits, inflammation, and vision changes.
Patient Counseling
- Educate about the importance of surgical removal and the risks of delaying intervention.
- Discuss potential for permanent vision changes and the goals of therapy, emphasizing early detection and consistent monitoring.
Practical Advice:
If you work in a high-risk environment, wear appropriate eye protection and report any eye injuries promptly, even if initial discomfort is minor.
Operative Procedures and Minimally Invasive Techniques
Definitive management of chalcosis centers on the surgical removal of the offending copper foreign body, combined with measures to address secondary tissue damage.
Foreign Body Removal
- Pars Plana Vitrectomy:
- The primary surgical method for extracting intraocular foreign bodies.
- Involves removing the vitreous gel and carefully extracting the copper fragment with specialized forceps or magnets.
- Offers direct access to the retina and minimizes trauma to surrounding tissues.
- Magnet-Assisted Extraction:
- When the copper content is sufficiently high and the foreign body is magnetic, intraocular magnets can assist in retrieval, often combined with vitrectomy.
Addressing Secondary Effects
- Cataract Surgery:
- Many patients develop a characteristic “sunflower” cataract; phacoemulsification with intraocular lens implantation may be performed at the same time as foreign body removal.
- Corneal Surgery:
- Severe corneal deposits or decompensation may require endothelial keratoplasty or, rarely, penetrating keratoplasty (corneal transplant).
- Retinal Repair:
- Retinal tears, detachment, or degeneration secondary to copper toxicity may require laser therapy, cryotherapy, or internal tamponade (gas or oil).
Minimally Invasive Innovations
- 23/25-Gauge Microincision Vitrectomy:
- Newer microincision techniques reduce surgical trauma, shorten recovery, and lower complication risk.
- Robotic-Assisted Extraction:
- Investigational systems provide ultra-fine control, reducing iatrogenic damage during foreign body retrieval.
Postoperative Care
- Intensive topical and systemic antibiotics to prevent infection.
- Steroid drops or tablets to control inflammation.
- Regular follow-up to monitor for recurrence or late complications such as glaucoma, macular edema, or retinal scarring.
Practical Advice:
Choose a surgeon experienced in ocular trauma and foreign body extraction for the best chance of vision preservation. Adhering to all postoperative instructions maximizes outcomes.
Next-Generation Treatments and Technology Advances
Innovations in both technology and medical science are rapidly improving outcomes for patients with chalcosis, focusing on precision, safety, and faster recovery.
Advanced Diagnostic Tools
- High-Resolution Imaging:
- Optical coherence tomography (OCT) and anterior segment imaging help map the extent of copper deposits and guide surgical planning.
- Elemental Analysis:
- New diagnostic techniques can rapidly identify the metal composition of intraocular foreign bodies, facilitating targeted management.
Novel Therapeutic Strategies
- Sustained-Release Drug Implants:
- Experimental intravitreal implants may deliver anti-inflammatory or neuroprotective agents over time to mitigate copper-induced retinal damage.
- Nanotechnology:
- Nanoparticles are being developed to bind and neutralize copper ions within ocular tissues, potentially reversing some toxic effects.
AI and Robotics
- Robotic Surgery Platforms:
- Precision micro-robotics enhance foreign body removal, reduce tissue damage, and may eventually automate some aspects of vitreoretinal surgery.
- Artificial Intelligence Diagnostics:
- AI tools are being trained to distinguish chalcosis from similar conditions (such as siderosis bulbi) on imaging, improving early diagnosis and triage.
Telemedicine and Remote Monitoring
- Digital apps and wearable sensors are in development to monitor visual function, alerting both patients and providers to early signs of progression or complications.
Practical Advice:
Discuss the availability of advanced imaging or minimally invasive surgery options with your ophthalmologist, especially at major eye trauma or tertiary centers.
Ongoing Research, Clinical Trials, and Future Outlook
Cutting-edge research is paving the way for safer, more effective, and personalized approaches to chalcosis care.
Current Clinical Studies
- Comparative Surgical Trials:
- Head-to-head comparisons of standard vs. microincision vitrectomy for foreign body removal, focusing on recovery time and long-term vision.
- Neuroprotection Trials:
- Investigating the use of neuroprotective agents and antioxidants to limit retinal degeneration after copper exposure.
- Chelation Therapy Studies:
- Assessing novel chelating agents or delivery systems for localized copper detoxification in ocular tissues.
Research Pipeline and Expected Advances
- Genomic and Proteomic Profiling:
- Understanding genetic factors that affect susceptibility and healing after copper exposure.
- Biomarker Discovery:
- Identifying blood or ocular fluid biomarkers for early detection of copper toxicity or predicting surgical outcomes.
Future Directions
- Earlier and more accurate diagnosis using portable imaging and AI analysis.
- Broader access to robotic and minimally invasive surgery, even in smaller centers.
- Integration of personalized medicine—treatments tailored to individual risk factors, injury characteristics, and healing capacity.
Practical Advice:
Consider participating in clinical trials if eligible, as this can provide access to state-of-the-art therapies and contribute to medical advancement. Stay in touch with your specialist about upcoming options.
Frequently Asked Questions
What is chalcosis and how does it affect vision?
Chalcosis is eye toxicity from retained copper, leading to deposits in cornea, lens, and retina. It can cause vision changes, colored rings, or cataracts if not treated.
How is chalcosis diagnosed?
Diagnosis combines a history of metal injury, clinical examination, and imaging such as X-ray or CT to detect copper fragments, plus slit-lamp exam for characteristic deposits.
Is surgery always required for chalcosis?
Most cases require surgical removal of the copper foreign body to prevent progressive toxicity. The sooner surgery is performed, the better the chance of vision preservation.
Can vision recover after treatment for chalcosis?
Vision often improves if copper is removed early and secondary damage is limited. Severe or delayed cases may result in permanent vision loss, highlighting the importance of prompt care.
What complications can occur with chalcosis?
Potential complications include cataracts, corneal opacities, retinal damage, glaucoma, and chronic inflammation. Early detection and management reduce these risks.
Are there ways to prevent chalcosis?
Wearing eye protection in high-risk jobs and seeking immediate care for eye injuries are the best preventive measures. Early removal of metallic foreign bodies is crucial.
What are the latest advances in chalcosis management?
Recent advances include microincision vitrectomy, AI-powered imaging, nanomedicine, and sustained-release ocular drug implants—all improving safety and outcomes.
Disclaimer:
This guide is intended for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Please consult your eye specialist for individual assessment and management of chalcosis or any eye injury.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform. Your support helps us continue providing reliable, up-to-date health information. Follow us on social media for more expert eye care insights!






