What is non-arteritic anterior ischemic optic neuropathy (NAION)?
Non-arteritic anterior ischemic optic neuropathy (NAION) is a condition that causes sudden, painless vision loss in one eye due to a lack of blood flow to the anterior portion of the optic nerve. It is the most common cause of acute optic neuropathy among people over the age of 50. Unlike arteritic anterior ischemic optic neuropathy, which is associated with giant cell arteritis, NAION is not associated with artery inflammation. Understanding NAION is critical for early detection and treatment, which can help to reduce vision loss and prevent recurrence in the other eye.
Detailed Investigation of Non-Arteritic Anterior Ischemic Optic Neuropathy (NAION)
NAION is a complex ocular condition caused by ischemia, or insufficient blood supply, to the optic nerve head. This section discusses the pathophysiology, risk factors, clinical presentation, and potential complications of NAION.
Pathophysiology
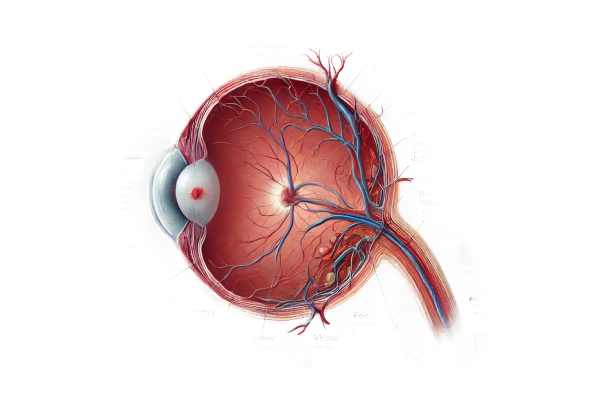
NAION results from a disruption in blood flow to the optic nerve head, which is supplied by the posterior ciliary arteries. This disruption causes ischemia and subsequent damage to the optic nerve fibers. Several mechanisms have been suggested to explain this ischemia:
- Structural Factors: People with a “crowded” optic disc, also called a “disc at risk,” are more likely to develop NAION. This anatomical variation can compress the small blood vessels supplying the optic nerve, increasing their susceptibility to ischemia.
- Nocturnal Hypotension: Blood pressure naturally drops while sleeping. In some people, nocturnal hypotension can reduce blood flow to the optic nerve to dangerously low levels, precipitating an ischemic event.
- Vascular Risk Factors: Hypertension, diabetes, hyperlipidemia, and obstructive sleep apnea can all contribute to atherosclerosis and other vascular abnormalities, reducing blood flow to the optic nerve.
Clinical Features
NAION is characterized by sudden, painless vision loss in one eye upon waking. The degree of vision loss varies, but it typically affects the central or inferior visual fields. Key clinical characteristics include:
- Decreased Visual Acuity: Most patients experience a decrease in visual acuity, which can be mild to severe.
- Visual Field Defects: Patients commonly report altitudinal field defects, which affect either the upper or lower half of their visual field.
- Relative Afferent Pupillary Defect (RAPD): An abnormal pupil response to light in the affected eye, which indicates optic nerve dysfunction.
- Optic Disc Edema: Swelling of the optic nerve head is typically visible during a fundoscopic examination. The edema may be sectoral or diffuse.
- Disc Hemorrhages: Small hemorrhages on or near the optic disc may occur, indicating vascular leakage.
Risk Factors
Several factors raise the risk of developing NAION:
- Age: NAION primarily affects people over the age of fifty.
- Cardiovascular Disease: Hypertension, diabetes, and hyperlipidemia are major risk factors.
- Sleep Apnea: Obstructive sleep apnea is strongly associated with NAION due to intermittent hypoxia and vascular dysregulation.
- Medications: NAION has been associated with certain medications, such as phosphodiesterase inhibitors used to treat erectile dysfunction.
- Genetic Predisposition: A family history of NAION or other vascular conditions may heighten the risk.
Complications
The main complication of NAION is permanent vision loss in the affected eye. Approximately 40% of patients experience some level of visual improvement, but significant recovery is uncommon. Other complications are:
- Second Eye Involvement: Within five years, approximately 15-20% of patients develop NAION in their fellow eye.
- Psychosocial Impact: A sudden loss of vision can cause significant emotional distress, anxiety, and depression, reducing the patient’s quality of life.
Differential Diagnosis
Several conditions can mimic the presentation of NAION, so accurate diagnosis is essential.
- Arteritic Anterior Ischemic Optic Neuropathy (AAION): Similar to giant cell arteritis, AAION presents with systemic signs of inflammation such as headache, jaw claudication, and elevated erythrocyte sedimentation rate (ESR).
- Optic Neuritis: Inflammatory demyelination of the optic nerve, commonly associated with multiple sclerosis, is characterized by pain with eye movement and a more pronounced recovery of vision.
- Central Retinal Artery Occlusion (CRAO): Sudden, painless vision loss caused by occlusion of the central retinal artery. Fundoscopy reveals a distinctive cherry-red spot on the macula.
- Branch Retinal Artery Occlusion (BRAO): Similar to CRAO, but affects a branch of the retinal artery, resulting in sectoral visual field loss.
Diagnostic methods
A comprehensive approach, including clinical evaluation, imaging studies, and laboratory tests, is required to accurately diagnose NAION. Each diagnostic method is critical for confirming the diagnosis and ruling out other possible causes of optic neuropathy.
Clinical Evaluation
- Patient History: A detailed history is required, with emphasis on the onset and progression of vision loss, associated symptoms, and underlying medical conditions. Questions about cardiovascular health, sleep apnea, and medication use are especially important.
- Ophthalmic Examination: A thorough eye examination involves:
- Visual Acuity Test: Determines the extent of vision loss.
- Pupillary Response: Assessing for a relative afferent pupillary defect (RAPD).
- Fundoscopy: Examine the optic disc for edema, pallor, and hemorrhages.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve head, allowing for detailed visualization of optic disc edema and structural changes in the retinal nerve fiber layer.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and then taking sequential images of the retinal circulation. It aids in the identification of areas with delayed or blocked blood flow and distinguishes NAION from other vascular disorders.
- Magnetic Resonance Imaging (MRI): An MRI of the brain and orbits may be used to rule out compressive or infiltrative lesions affecting the optic nerve, as well as to distinguish NAION from other optic neuropathies like optic neuritis or tumors.
Lab Tests
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These inflammatory markers are critical for ruling out arteritic anterior ischemic optic neuropathy (AAION), which requires immediate treatment.
- Blood Glucose and Lipid Profile: Assessing diabetes and hyperlipidemia, both of which are risk factors for NAION.
- Complete Blood Count (CBC): Looking for underlying systemic conditions that could lead to vascular compromise.
Treatment
The primary goals of treating Non-Arteritic Anterior Ischemic Optic Neuropathy (NAION) are to manage acute episodes, prevent recurrence, and address underlying risk factors. While there is no universally accepted treatment for NAION-related vision loss, several approaches aim to improve outcomes and reduce the likelihood of future damage.
Immediate Management
- Observation and Monitoring: Many cases of NAION are managed with close observation, as the condition’s natural course can include some spontaneous improvement in vision. Regular follow-ups are required to monitor the condition and detect changes.
- Steroids: While the efficacy of steroids in treating NAION is debatable, some doctors prescribe corticosteroids to alleviate inflammation and edema in the optic nerve. High-dose oral or intravenous steroids may be considered in certain cases, especially during the acute phase.
Long-Term Management
- Control of Vascular Risk Factors: Treating underlying conditions like hypertension, diabetes, and hyperlipidemia is critical. Effective management of these risk factors can aid in preventing recurrence and protecting the unaffected eye.
- Antihypertensive Medications: Controlling blood pressure is critical to lowering the risk of future ischemic events.
- Diabetic Management: To prevent vascular complications, patients with diabetes must maintain strict glycemic control.
- Lipid-Lowering Agents: Statins and other lipid-lowering drugs can help lower the risk of atherosclerosis and subsequent ischemic events.
- Lifestyle Modifications: Encouraging patients to live healthier lifestyles can help prevent future episodes.
- Diet and Exercise: Maintaining a healthy diet and engaging in regular physical activity can help control weight, blood pressure, and cholesterol levels.
- Smoking Cessation: Smoking is a major risk factor for vascular diseases, and quitting can help reduce the risk of NAION recurrence.
- Sleep Apnea Treatment: Continuous positive airway pressure (CPAP) therapy for patients with obstructive sleep apnea can improve oxygenation during sleep and lower the risk of nocturnal hypotension.
Emerging and Experimental Therapies
- Neuroprotective Agents: Researchers are looking into medications that could protect the optic nerve from ischemic damage. These agents seek to preserve nerve function and prevent further deterioration.
- Ischemic Preconditioning: Researchers are looking into whether controlled, short-term ischemic episodes in other parts of the body can help the optic nerve withstand ischemia better.
- Gene Therapy: Although still in its early stages, gene therapy holds promise for treating genetic predispositions to vascular conditions that contribute to NAION.
- Regenerative Medicine: Stem cell therapy and other regenerative approaches are being investigated for repairing optic nerve damage and restoring vision.
Strategies for Improving and Avoiding Non-Arteritic Anterior Ischemic Optic Neuropathy (NAION)
Preventing and managing NAION requires a combination of medical treatments and lifestyle changes. Here are a few effective methods:
- Regular Medical Check-Ups: Routine health screenings can help detect and manage risk factors such as hypertension, diabetes, and hyperlipidemia at an early stage.
- Blood Pressure Control: To reduce the risk of ischemic events, maintain optimal blood pressure levels with medication, diet, and exercise.
- Blood Sugar Management: Diabetic patients must maintain strict glycemic control to avoid vascular complications that can lead to NAION.
- Lipid Management: Use lipid-lowering medications such as statins to control cholesterol levels and lower the risk of atherosclerosis.
- Smoking Cessation: Quit smoking to improve vascular health and lower your risk of ischemic optic neuropathy.
- Healthy Diet and Exercise: A balanced diet high in fruits, vegetables, and whole grains, combined with regular physical activity, can improve cardiovascular health and lower NAION risk.
- Sleep Apnea Treatment: For people with obstructive sleep apnea, CPAP therapy can improve oxygenation and reduce nocturnal hypotension, lowering their risk of NAION.
- Medication Review: Consult with your doctor on a regular basis to avoid medications that may increase your risk of NAION, such as certain vasodilators or erectile dysfunction drugs.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Peter A. Demaer
- “Neuro-Ophthalmology Illustrated” by Valerie Biousse and Nancy J. Newman










