What is ocular myasthenia gravis?
Ocular Myasthenia Gravis (OMG) is a subtype of Myasthenia Gravis (MG), an autoimmune neuromuscular disorder that affects the muscles responsible for eye and eyelid movement. Patients with OMG have fluctuating weakness and fatigue of the ocular muscles, which causes symptoms like ptosis (drooping of one or both eyelids), diplopia (double vision), and blurred vision. OMG, unlike generalized Myasthenia Gravis, affects only the muscles around the eyes.
Comprehensive Insights on Ocular Myasthenia Gravis
Pathophysiology
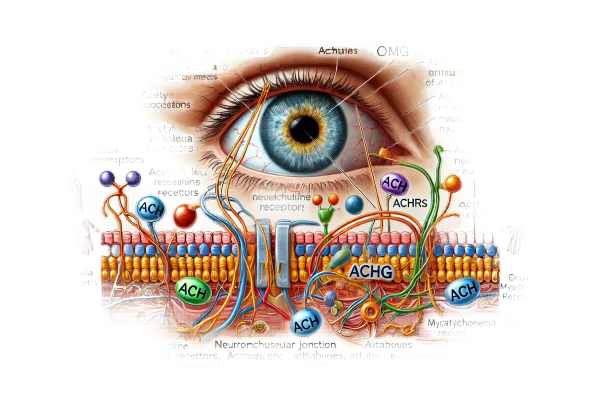
OMG is an autoimmune disease in which the immune system creates antibodies that attack the acetylcholine receptors (AChRs) at the neuromuscular junction. Acetylcholine is a neurotransmitter that sends nerve impulses to muscle fibers, causing them to contract. In OMG, antibodies block or destroy these receptors, preventing nerves and muscles from communicating properly, resulting in muscle weakness and fatigue.
- Immune Mechanisms: The autoimmune response in OMG includes the production of autoantibodies against AChRs and, in some cases, muscle-specific kinase (MuSK). These antibodies disrupt neuromuscular transmission, impairing muscle contraction.
- Neuromuscular Junction Dysfunction: The neuromuscular junction is the primary cause of pathology in OMG. The binding of autoantibodies to AChRs reduces the number of functional receptors and causes complement-mediated damage to the postsynaptic membranes. This reduces the efficiency of neuromuscular transmission.
Clinical Presentation
OMG causes distinct ocular symptoms due to selective involvement of the extraocular and eyelid muscles. The key symptoms are:
- Ptosis: Ptosis, or drooping of the eyelids, is a defining characteristic of OMG. It can affect one or both eyelids and may worsen throughout the day or after prolonged use of the eye muscles.
- Diplopia: Diplopia, also known as double vision, occurs when the extraocular muscles are weak and misaligned. This symptom can be intermittent or persistent, and the severity varies throughout the day.
- Fatigability: Muscle weakness in OMG is defined by fatigability, which occurs when symptoms worsen with continued use and improve with rest. Patients may notice that their ptosis and diplopia become more noticeable after extended periods of reading or other visual activities.
- Variability: OMG symptoms can vary in severity from day to day, and even within the same day. This variability is a key characteristic that distinguishes OMG from other ocular disorders.
Epidemiology
OMG can affect people of all ages, but it is most common in adults aged 20 to 40. It is slightly more common in women than in men. OMG’s prevalence varies by geography, but it is generally considered a rare condition.
Risk Factors
Several factors may increase the risk of developing OMG:
- Genetics: Having a genetic predisposition to autoimmune diseases increases the risk of developing OMG. Individuals with a family history of autoimmune disorders are at an increased risk.
- Thymus Abnormalities: The thymus gland, which is involved in immune system development, may play a role in OMG. Thymic hyperplasia (enlargement) or thymoma (thymus tumor) are associated with MG and can influence OMG development.
- Other Autoimmune Diseases: People who have other autoimmune diseases, such as rheumatoid arthritis, lupus, or thyroiditis, are more likely to develop OMG.
Pathogenesis
The pathogenesis of OMG is a complex interplay of genetic, environmental, and immunological factors:
- Autoantibody Production: The immune system mistakenly produces antibodies against AChRs or MuSK. These autoantibodies disrupt normal neuromuscular transmission, causing muscle weakness.
- Complement Activation: Autoantibodies bind to AChRs, activating the complement system, a component of the immune response that aids in pathogen clearance. This activation causes the destruction of the postsynaptic membrane at the neuromuscular junction.
- Thymic Involvement: The thymus gland is thought to play an important role in the pathogenesis of MG, including OMG. Thymic abnormalities, such as hyperplasia or thymoma, can initiate or exacerbate the autoimmune response.
Differential Diagnosis
OMG can mimic other conditions that cause similar ocular symptoms, so differential diagnosis is essential.
- Chronic Progressive External Ophthalmoplegia (CPEO) is a mitochondrial disorder that results in progressive weakness of the extraocular muscles. Unlike OMG, CPEO typically presents with slowly progressive symptoms and lacks the characteristic variability of OMG.
- Thyroid Eye Disease: Thyroid eye disease, which is associated with thyroid dysfunction, can cause eye muscle swelling and fibrosis, resulting in OMG-like symptoms. However, additional symptoms of thyroid eye disease include proptosis (bulging eyes) and eyelid retraction.
- Oculopharyngeal Muscular Dystrophy (OPMD) is a genetic condition that causes progressive weakness in the eyelid and pharyngeal muscles. It distinguishes itself from OMG’s variable symptoms by presenting with slowly progressive ptosis and dysphagia.
- Myasthenic Syndrome (Lambert-Eaton Myasthenic Syndrome): Similar to MG, this condition primarily affects the limbs and is frequently associated with small cell lung cancer. It rarely affects the eye muscles.
Complications
If left untreated or poorly managed, OMG can cause a number of complications:
- Chronic Ptosis: Persistent ptosis can impair vision and cause secondary complications such as amblyopia (lazy eye) in children.
- Quality of Life: OMG symptoms’ fluctuating and unpredictable nature can have a significant impact on daily activities and emotional well-being.
- Progression to Generalized MG: Although OMG begins in the ocular muscles, it can progress to generalized MG in some patients, affecting other muscle groups and causing more severe complications.
Prognosis
The prognosis for OMG varies by individual. Some patients may experience complete remission, while others may still have symptoms. Early diagnosis and management are critical for improving outcomes and avoiding complications.
Diagnostic Techniques for Ocular Myasthenia Gravis
Clinical Examination
- Patient History: A thorough patient history is required to diagnose OMG. Clinicians will ask about the onset, duration, and variability of symptoms, as well as any factors that exacerbate or alleviate them. A family history of autoimmune diseases could also be relevant.
- Physical Examination: A thorough physical examination, including a detailed neurological and ocular evaluation, is required. The examination focuses on detecting signs of ptosis, diplopia, and ocular muscle fatigue. To assess variability and fatigability, the clinician may observe the patient’s eye movements and eyelid position in a variety of situations.
Diagnostic Tests
- Ice Pack Test: The ice pack test is a simple bedside procedure that distinguishes OMG from other causes of ptosis. Applying an ice pack to the affected eyelid for a few minutes can help with ptosis in OMG patients because it reduces neuromuscular junction fatigue.
- Tensilon Test: This test requires the administration of edrophonium chloride (Tensilon), a short-acting acetylcholinesterase inhibitor. The improvement in muscle strength following the injection supports the diagnosis of MG, including OMG.
- Serological Tests: Blood tests can detect autoantibodies to AChRs or MuSK. The presence of these antibodies supports the diagnosis of MG, including OMG.
Electrophysiological Studies
- Repetitive Nerve Stimulation (RNS): RNS is a nerve conduction study that tests neuromuscular transmission by repeatedly stimulating a nerve and measuring the muscle response. A decremental response indicates MG.
- Single Fiber Electromyography (SFEMG) is a highly sensitive test that detects electrical activity in individual muscle fibers. It can identify abnormalities in neuromuscular transmission even when other tests are inconclusive.
Imaging Studies
- Chest Imaging: A chest X-ray or CT scan is used to examine the thymus gland for abnormalities such as thymic hyperplasia or thymoma, which are linked to MG.
Ocular Myasthenia Gravis Treatment
Medical Management
- Acetylcholinesterase Inhibitors: These medications, including pyridostigmine (Mestinon), improve neuromuscular transmission by inhibiting the enzyme acetylcholinesterase, which degrades acetylcholine. Acetylcholine levels at the neuromuscular junction rise, which improves muscle contraction and relieves symptoms of ptosis and diplopia.
- Immunosuppressive Therapy: Immunosuppressants like corticosteroids (prednisone), azathioprine, and mycophenolate mofetil are used to suppress the autoimmune response. These drugs help to reduce the production of autoantibodies that attack acetylcholine receptors. Corticosteroids can cause serious side effects if used for an extended period of time, so their use is frequently monitored.
- IVIG and Plasmapheresis: These treatments are usually reserved for severe or refractory cases of OMG. IVIG gives the immune system a temporary boost, which helps to reduce antibody levels. Plasmapheresis involves filtering the blood to remove autoantibodies, which provides temporary relief from symptoms.
Surgical Treatment
- Thymectomy: Patients with thymoma or thymic hyperplasia should have the thymus gland surgically removed (thymectomy). Thymectomy can cause remission or significant improvement in symptoms for many MG patients, including those with OMG. It is frequently considered for patients who do not respond well to medical therapy.
Innovative and Emerging Therapies
- Biologic Agents: Emerging therapies that target specific immune system components show promise for treating MG. Monoclonal antibodies like rituximab, which targets B-cells, and eculizumab, which inhibits the complement system, are being investigated for their efficacy in reducing autoantibody production and neuromuscular damage.
- Gene Therapy: Research into gene therapy seeks to correct the underlying genetic defects that predispose people to autoimmune diseases such as MG. Initial research focuses on modifying or replacing faulty genes to prevent or reduce the production of harmful autoantibodies.
- Targeted Molecular Treatments: Advances in molecular biology are enabling the development of drugs that target specific molecular pathways involved in the autoimmune response. These targeted therapies have the potential to improve the efficacy and safety of OMG treatments.
Lifestyle and Supportive Therapies
- Physical Therapy: Physical therapy can help keep muscles strong and functional, reduce fatigue, and improve overall physical fitness. Exercise programs designed to avoid overexertion are beneficial.
- Occupational Therapy: Occupational therapists can offer patients strategies and adaptive tools to help them manage daily activities and maintain independence despite muscle weakness.
- Support Groups and Counseling: Emotional support and counseling can help patients deal with the psychological effects of having a chronic condition like OMG. Support groups allow people to share their experiences and strategies for managing the disease.
Effective Ways to Improve and Prevent Ocular Myasthenia Gravis
- Regular Medical Follow-Up: Make regular appointments with your neurologist and ophthalmologist to monitor disease progression and adjust treatment plans as needed.
- Medication Adherence: Take your prescribed medications on a consistent basis and as directed. Adherence to treatment plans is critical for symptom management and preventing exacerbations.
- Stress Management: Try stress-relieving activities like yoga, meditation, or mindfulness practices. Stress can worsen symptoms, so managing stress is critical for overall health.
- Balanced Diet: Eat a nutritious, well-balanced diet to promote overall health and immune function. Avoid foods that may interact with medications or worsen symptoms.
- Adequate Rest: Get enough rest and avoid over-exertion. Fatigue can exacerbate symptoms, so balancing activity with adequate rest is critical.
- Protect Your Eyes from Strain: Use proper lighting and take breaks to avoid eye strain while reading or working on a computer. Consider using eyeglasses or other aids prescribed by your ophthalmologist.
- Monitor for Symptoms: Keep an eye on your symptoms and notify your healthcare provider as soon as they change. Early intervention can help prevent complications.
- Avoid Infections: Maintain good hygiene to reduce the risk of infection, as illnesses can worsen OMG symptoms. Stay up to date on vaccinations and avoid contact with sick people.
- Wear Sunglasses: Sunlight and glare can exacerbate symptoms of diplopia and ptosis. Wearing sunglasses outside and in bright environments can help to alleviate discomfort.
- Educate Yourself: Stay current on OMG and its management. Understanding your condition allows you to make more informed decisions about your health and treatment.
Trusted Resources
Books
- “Myasthenia Gravis: A Manual for the Health Care Provider” by John G. Byrne
- “Myasthenia Gravis: The Facts” by Henry J. Kaminski
- “Neuromuscular Disorders: Treatment and Management” by Matthew N. Meriggioli and Jerry R. Mendell
Online Resources
- Myasthenia Gravis Foundation of America (MGFA): myasthenia.org
- National Institute of Neurological Disorders and Stroke (NINDS): ninds.nih.gov
- Mayo Clinic: mayoclinic.org










