A conjunctival laceration is a tear or cut in the conjunctiva, the clear membrane covering the white part of the eye and inner eyelids. This injury often results from trauma—such as fingernail scratches, foreign bodies, or blunt force—and, though sometimes minor, may signal more serious ocular damage. Prompt and accurate assessment is essential to prevent complications like infection, scarring, or involvement of deeper eye structures. In this comprehensive guide, you’ll find an up-to-date exploration of current therapies, surgical techniques, and the latest innovations, with practical tips and a warm, reader-centered approach.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
- Disclaimer
Condition Overview and Epidemiology
A conjunctival laceration involves a disruption in the conjunctival tissue, ranging from a small superficial tear to a more extensive wound. This condition may occur in isolation or, more seriously, in conjunction with deeper eye injuries (such as scleral or corneal lacerations). Understanding the context and severity of the trauma is essential, as a conjunctival tear can sometimes mask more severe ocular damage.
Key Points:
- Definition: A partial or full-thickness break in the conjunctival tissue.
- Common Causes:
- Direct trauma (fingernails, twigs, toys, tools, sports accidents)
- Foreign bodies
- Surgical complications (post-ophthalmic surgery or injections)
- Animal scratches or bites
- Prevalence: Conjunctival lacerations are relatively common, especially among children, active adults, and those working in high-risk environments.
- Risk Factors:
- Participation in contact sports
- Use of power tools or gardening equipment
- Children’s play and unsupervised activities
- Elderly individuals (falls, decreased reflexes)
Pathophysiology:
- The conjunctiva is richly supplied with blood vessels and immune cells, which can help healing but also make it prone to swelling, bleeding, and secondary infection.
- While most conjunctival lacerations are not vision-threatening, those that expose the underlying sclera or allow foreign material into the eye require urgent attention.
Clinical Presentation:
- Redness, tearing, foreign body sensation
- Visible tear or flap in the conjunctiva
- Possible subconjunctival hemorrhage (red patch under the surface)
- Pain or discomfort, especially with blinking
- In more severe cases: decreased vision, deeper eye pain, or signs of globe rupture
Diagnosis:
- Careful slit-lamp examination, sometimes aided by fluorescein staining, reveals the extent and depth of the injury.
- Assessment for retained foreign bodies, globe integrity, and involvement of the limbus or fornices is vital.
- If the wound is near the limbus or deep, imaging (e.g., B-scan ultrasound, CT scan) may be warranted to rule out intraocular injury.
Practical Advice:
If you experience sudden eye pain after trauma—especially with a visible cut, blood, or discharge—avoid rubbing your eye, protect it with a clean shield or cloth, and seek prompt medical attention. Do not attempt to remove any embedded material yourself.
Conventional and Pharmacological Therapies
Most conjunctival lacerations are minor and heal well with conservative management, but the key is to tailor therapy based on the injury’s size, depth, and location.
Primary Non-Surgical Treatments:
- Observation: Small (<10 mm), superficial lacerations without underlying tissue exposure often heal spontaneously within 7–10 days. Gentle care and close monitoring suffice.
- Topical Antibiotics: To prevent infection, broad-spectrum antibiotic drops or ointments (such as erythromycin, polymyxin-bacitracin, or moxifloxacin) are routinely prescribed.
- Lubricants: Artificial tears and lubricating gels reduce discomfort and promote healing.
- Analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen help manage pain.
- Tetanus Prophylaxis: Particularly important for traumatic wounds from contaminated sources.
Indications for Medical Therapy:
- All patients should be evaluated for signs of infection (increased redness, pus, worsening pain).
- Inflammation (chemosis, swelling) may be controlled with cold compresses and, rarely, mild topical steroids—always under specialist supervision.
Practical Steps for At-Home Care:
- Wash hands thoroughly before touching the eye or applying medications.
- Avoid rubbing or squeezing the eyelids.
- Apply drops or ointment as prescribed, usually several times daily.
- Wear protective eyewear if there is a risk of further trauma or during recovery.
- Return for follow-up if symptoms worsen or do not improve within a few days.
When to Seek Urgent Care:
- Deep wounds
- Signs of globe perforation (sudden vision loss, misshapen pupil, severe pain)
- Retained foreign bodies
- Involvement of the limbus (edge of cornea)
- Associated injuries (orbital fractures, lid lacerations)
Patient Empowerment:
Stay vigilant for signs of infection or worsening discomfort. Early intervention can prevent complications and speed recovery.
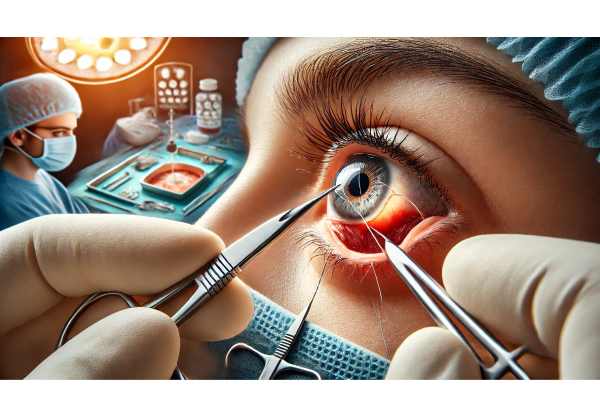
Surgical and Interventional Procedures
Surgical repair is considered for larger or more complex conjunctival lacerations, those with tissue avulsion, persistent bleeding, or associated injuries.
Surgical Indications:
- Lacerations >10 mm or with gaping, tissue loss, or poor alignment
- Exposure of underlying sclera or rectus muscles
- Foreign bodies embedded in the conjunctiva or sclera
- Combined injuries involving the eyelid, sclera, or cornea
- Non-healing wounds after conservative treatment
Surgical Techniques:
- Wound Preparation: Local anesthesia is administered; the area is cleaned, and any foreign material is carefully removed.
- Suturing: Fine, absorbable sutures (e.g., 8-0 or 9-0 vicryl) are used to re-approximate the conjunctival edges. Minimal tension is applied to avoid tissue necrosis.
- Hemostasis: Gentle cautery or pressure controls bleeding.
- Closure of Adjacent Tissues: If the sclera, Tenon’s capsule, or rectus muscles are involved, layered closure may be necessary.
- Adjunctive Measures: Use of tissue adhesives (fibrin glue) in select, superficial cases to speed healing and improve comfort.
Postoperative Care:
- Continued topical antibiotics and lubricants
- Short course of topical steroids if indicated (to reduce inflammation)
- Avoidance of eye rubbing, heavy lifting, or strenuous activity for several days
- Timely follow-up to monitor healing and remove any non-absorbable sutures if used
Managing Complications:
- Monitor for infection, wound dehiscence, or conjunctival scarring.
- Prompt treatment of symblepharon (adhesion between eyelid and eyeball) with topical lubricants, massage, or surgical release.
Recovery Outlook:
With skilled care, most patients regain normal appearance and function with minimal scarring. Severe injuries may require staged surgeries or reconstructive procedures.
Practical Advice:
After any eye surgery, always adhere closely to post-op instructions. Report persistent redness, pain, or changes in vision to your doctor without delay.
Emerging Innovations and Advanced Technologies
In recent years, management of conjunctival lacerations has benefited from several technological and procedural innovations.
Bioengineered Tissue and Advanced Healing Agents:
- Amniotic Membrane Transplantation (AMT): Biologic grafts provide scaffolding for healing, reduce inflammation, and minimize scarring. Used for extensive or recurrent wounds.
- Tissue Adhesives: Fibrin glue and newer synthetic adhesives speed wound closure and patient comfort, reducing the need for sutures in minor tears.
- Growth Factor Eye Drops: Emerging therapies utilize recombinant human growth factors to accelerate healing in complex or slow-to-heal cases.
Digital Tools and AI-Powered Diagnostics:
- Mobile devices with high-resolution cameras and AI algorithms support remote assessment and triage in emergency settings.
- Teleophthalmology services connect patients with specialists for prompt guidance after ocular injuries.
Improved Imaging Modalities:
- Ultra-high-resolution anterior segment optical coherence tomography (OCT) enables precise visualization of wound depth and associated injuries, enhancing surgical planning.
Personalized Wound Management:
- Genetically informed approaches (under investigation) may optimize healing based on individual risk of scarring or inflammation.
Clinical Integration:
These advances are becoming more accessible, especially in major trauma centers and academic eye hospitals. Patients should inquire about the latest options available locally.
Practical Advice:
If referred to a tertiary center for advanced therapies, don’t hesitate to ask about the benefits and risks of newer treatments versus traditional options.
Clinical Trials and Future Directions
The ongoing quest to improve outcomes for ocular trauma—including conjunctival lacerations—has spurred a range of research and clinical trials.
Current Research Highlights:
- Novel Tissue Scaffolds: Trials are underway for synthetic and stem cell-derived conjunctival grafts that could revolutionize severe injury repair.
- Advanced Anti-Scarring Agents: Investigational medications aim to prevent symblepharon and reduce post-traumatic scarring.
- Regenerative Medicine: Cell-based therapies and biologics may soon enable better tissue regeneration after complex lacerations.
- Telehealth Integration: Studies assess the efficacy and safety of remote triage and post-injury monitoring using digital platforms and AI.
Key Goals for Future Therapies:
- Faster, more comfortable healing
- Reduced risk of infection and long-term complications
- Enhanced visual and cosmetic outcomes
- Broader access to specialist care in rural and underserved communities
How Patients Can Participate:
- Many clinical trials are recruiting individuals with acute or complex conjunctival injuries.
- Participation often provides access to cutting-edge treatments and meticulous follow-up.
- Ask your provider about eligibility or explore registries at major academic eye centers.
Empowering Patients:
Staying engaged with research is a powerful way to access the latest advances and contribute to knowledge that may help others in the future.
Frequently Asked Questions
What is a conjunctival laceration and how serious is it?
A conjunctival laceration is a cut or tear in the clear tissue covering the white of the eye. While often minor, some cases may indicate deeper injuries and require prompt professional assessment.
What should I do immediately after an eye injury that causes bleeding or a tear?
Do not rub the eye. Gently shield it and seek medical care promptly. Avoid removing any objects embedded in the eye and do not apply pressure.
How are conjunctival lacerations treated?
Small lacerations may heal with antibiotic drops alone. Larger or more complex wounds may require stitches, tissue adhesives, or even surgery, depending on severity.
Can conjunctival lacerations heal on their own?
Superficial tears often heal without surgical intervention within a week, but proper hygiene and antibiotic drops are essential to prevent infection.
What are the signs of complications after an eye injury?
Persistent pain, increased redness, discharge, vision changes, or eyelid sticking to the eyeball (symblepharon) are warning signs—prompt re-evaluation is needed.
Are there any new treatments for conjunctival injuries?
Yes, advances such as amniotic membrane grafts, tissue adhesives, and AI-assisted teleophthalmology are improving outcomes and comfort in selected cases.
Disclaimer
The information provided here is for educational purposes only and should not be interpreted as medical advice. Always seek personalized care and recommendations from a qualified eye care professional for diagnosis and treatment of any eye injury.
If this article helped you, please consider sharing it on Facebook, X (formerly Twitter), or your favorite social network. Follow us for more expert updates, and support our mission to make quality eye health information accessible to all!






