What is Ocular Surface Squamous Neoplasia?
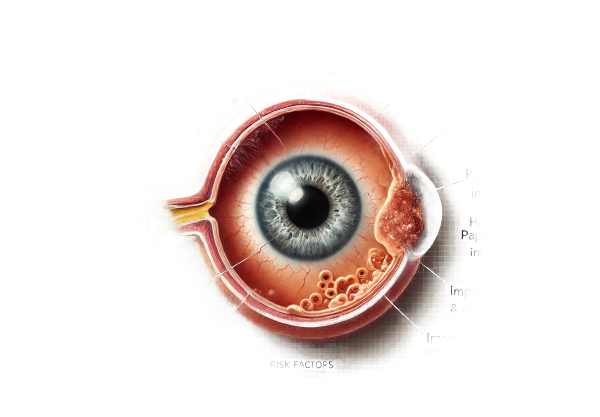
Ocular Surface Squamous Neoplasia (OSSN) is a type of eye tumor that develops from the squamous epithelium of the conjunctiva and cornea. The neoplasms range from benign dysplasia to invasive squamous cell carcinoma. OSSN is the most common type of ocular surface tumor, primarily affecting the elderly, but it can occur at any age. Early detection and appropriate management are critical for preventing progression and maintaining vision.
Detailed Insight into Ocular Surface Squamous Neoplasia
Etiology
Although the exact cause of OSSN remains unknown, several risk factors have been identified:
- Ultraviolet (UV) Radiation: Prolonged exposure to UV radiation, particularly UV-B rays from sunlight, poses a significant risk. UV radiation can damage DNA in the epithelial cells of the ocular surface, resulting in neoplastic changes.
- Human Papillomavirus (HPV): Infection with specific HPV strains, particularly types 16 and 18, has been linked to OSSN. The virus can integrate into the host’s DNA, disrupting normal cell regulation and promoting tumor formation.
- Immunosuppression: Conditions that impair the immune system, such as HIV/AIDS, raise the risk of OSSN. Immunosuppressive medications, which are commonly used in organ transplant recipients, also raise the risk.
- Chemical Exposure: Chronic chemical exposure, such as that found in industrial settings, can contribute to the development of OSSN.
- Chronic Inflammation: Persistent inflammation of the ocular surface, often caused by conditions such as chronic blepharitis or conjunctivitis, can predispose people to OSSN.
Pathophysiology
OSSN refers to a group of diseases characterized by abnormal growth of squamous cells on the ocular surface. The pathophysiology has several stages:
- Dysplasia: The first stage involves dysplastic changes in epithelial cells, which are pre-cancerous changes that can progress to carcinoma if left untreated.
- Carcinoma in Situ: This stage is a more advanced dysplasia in which abnormal cells remain confined to the epithelium and have not yet invaded the underlying tissues.
- Invasive Squamous Cell Carcinoma: Neoplastic cells penetrate the basement membrane and invade the underlying stroma, resulting in invasive squamous cell carcinoma. This stage has a higher risk of metastasis and necessitates more aggressive therapy.
Clinical Presentation
Patients with OSSN may present with a variety of symptoms, which can be subtle or severe depending on the stage and extent of the disease:
- Conjunctival Lesions: Visible growths on the conjunctiva are a common indication. These lesions may appear as elevated, gelatinous, or papillomatous masses. They could be leukoplakic (white and opaque) or have vascularization.
- Corneal Involvement: In some cases, the lesion extends onto the cornea, resulting in opacification and impaired vision.
- Redness and Irritation: The presence of a lesion on the ocular surface is characterized by chronic irritation, redness, and a foreign body sensation.
- Visual Disturbances: Advanced cases with significant corneal involvement may result in visual impairment.
- Pain: Pain is rarely a noticeable symptom unless the lesion becomes ulcerated or infected.
Differential Diagnosis
Differentiating OSSN from other ocular surface conditions is critical for proper diagnosis and treatment. Conditions that may mimic OSSN are:
- Pinguecula: A benign, yellowish growth on the conjunctiva that is often associated with UV exposure but is not precancerous.
- Pterygium: A fibrovascular growth extending from the conjunctiva to the cornea, usually caused by prolonged UV exposure and irritation.
- Conjunctival Intraepithelial Neoplasia (CIN): A precursor to OSSN that encompasses a variety of dysplastic changes in the conjunctival epithelium.
- Conjunctival Melanoma: A malignant tumor that develops from melanocytes in the conjunctiva and appears as a pigmented lesion.
- Conjunctivitis: Inflammation of the conjunctiva caused by infection or allergies, resulting in redness and swelling but lacking the neoplastic growth seen in OSSN.
Epidemiology
Despite its rarity, OSSN is the most common type of ocular surface tumor. Its prevalence varies geographically, with higher rates reported in areas with high UV radiation exposure, such as equatorial countries. The condition is more common in older adults, and men have a higher incidence than women.
Pathogenesis
The pathogenesis of OSSN is a multistep process of cellular transformation:
- Genetic Mutations: Both UV radiation and HPV infection can cause genetic mutations in squamous epithelial cells. These mutations disrupt the normal cell cycle regulation, resulting in uncontrolled cell proliferation.
- Immune Evasion: Neoplastic cells create mechanisms to avoid immune surveillance, allowing them to survive and proliferate in the presence of the immune system.
- Tumor Progression: As genetic instability increases, cells become more aggressive, progressing from dysplasia to carcinoma in situ, and finally invasive carcinoma.
Complications
If left untreated, OSSN can cause a number of complications:
- Local Invasion: Invasive squamous cell carcinoma can infiltrate deeper ocular tissues, such as the sclera and orbit, complicating treatment and potentially causing eye loss.
- Metastasis: Although uncommon, metastatic spread to regional lymph nodes or distant organs can occur, especially in advanced cases of invasive carcinoma.
- Recurrence: Even with treatment, OSSN has a high risk of recurrence, necessitating ongoing follow-up and monitoring.
Effects on Quality of Life
The presence of OSSN has a significant impact on a patient’s quality of life. Visual impairment, chronic irritation, and the psychological toll of a possible cancer diagnosis can all have an impact on daily activities and overall well-being. Early detection and appropriate management are critical for reducing these effects and improving patient outcomes.
Methods to Diagnose Ocular Surface Squamous Neoplasia
Clinical Examination
- Slit-Lamp Biomicroscopy is the primary method for examining the ocular surface. Slit-lamp biomicroscopy provides a detailed view of the lesion’s characteristics, such as size, shape, color, and extent of involvement. The use of high magnification and specialized filters can aid in distinguishing OSSN from benign conditions.
- Visual Acuity Test: Assessing the patient’s visual acuity is critical for determining the impact of the lesion on vision. Any decrease in vision could indicate corneal involvement or other complications.
- Photography: Clinical photography can document the appearance of the lesion and track changes over time, providing a visual record for comparison during subsequent visits.
Imaging Studies
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT generates high-resolution cross-sectional images of the anterior segment, allowing for a more detailed assessment of the lesion’s depth and underlying tissue involvement. It is especially useful for determining the level of corneal involvement.
- Ultrasound Biomicroscopy (UBM): UBM visualizes the internal structure of a lesion as well as its relationship to deeper ocular tissues using high frequency ultrasound. This modality is useful for determining the extent of invasion in advanced cases.
- High-Resolution Anterior Segment Magnetic Resonance Imaging (MRI): MRI can be used to assess the lesion’s size and involvement of surrounding structures. It is especially useful when there is a suspicion of deeper invasion or orbital involvement.
Histopathologic Examination
- Biopsy: A biopsy specimen is histopathologically examined to provide a definitive diagnosis of OSSN. The biopsy can be performed using excisional, incisional, or punch techniques, depending on the size and location of the lesion. The specimen is then examined under a microscope to determine whether it contains dysplastic or neoplastic cells, confirming the diagnosis.
- Immunohistochemistry: Immunohistochemical staining can aid in distinguishing OSSN from other types of neoplasms. Specific markers, such as p63 and Ki-67, can help determine the lesion’s proliferative activity and malignant potential.
Lab Tests
- HPV Testing: When HPV infection is suspected, polymerase chain reaction (PCR) testing can reveal the presence of high-risk HPV strains in the biopsy specimen. This information can help with treatment decisions and prognosis.
- HIV Testing: Because of the link between immunosuppression and OSSN, patients with risk factors or clinical signs of immunodeficiency may benefit from HIV testing.
Effective Treatments for Ocular Surface Squamous Neoplasia
The size, extent, and degree of invasion of the lesion determine the treatment for Ocular Surface Squamous Neoplasia (OSSN). The primary goals are to remove neoplastic tissue, preserve vision, and reduce the risk of recurrence. Treatment options include both surgical and non-surgical methods, with emerging therapies promising new avenues for management.
Surgical Treatment
- Excisional Biopsy: Surgical excision is the most common treatment option for localized OSSN. The lesion is carefully excised, leaving a margin of healthy tissue to ensure complete removal. Adjunctive cryotherapy is frequently used on surgical margins to eliminate residual tumour cells and reduce the risk of recurrence.
- Amniotic Membrane Transplantation: When large areas of conjunctiva are removed, amniotic membrane transplantation can aid in healing and reduce scarring. The amniotic membrane serves as a scaffold for epithelial regrowth and contains anti-inflammatory and scarring properties.
- Lamellar Keratectomy: For corneal lesions, a lamellar keratectomy may be performed to remove the neoplasm’s affected superficial layers.
Non-surgical Treatment
- Topical Chemotherapy: Topical chemotherapeutic agents used to treat OSSN include mitomycin C (MMC), 5-fluorouracil (5-FU), and interferon alpha-2b. These medications, administered as eye drops, work by inhibiting DNA synthesis and promoting cell death in neoplastic cells.
- Interferon Therapy: Interferon alpha-2b, administered topically or subconjunctivally, has antiviral and antiproliferative effects. It is especially effective in patients who cannot undergo surgery or have recurrent disease.
Innovative and Emerging Therapies
- Photodynamic Therapy (PDT): PDT uses a photosensitizing agent that, when activated by light, produces reactive oxygen species that destroy neoplastic cells. This method provides a non-invasive alternative to treating OSSN and can be used in conjunction with other treatments.
- Immunotherapy: Researchers are investigating novel immunotherapeutic approaches, such as checkpoint inhibitors and immune modulators, to improve the immune system’s ability to target and eliminate neoplastic cells.
- Gene Therapy: Advances in gene therapy show promise in targeting specific genetic mutations involved in OSSN. Techniques like CRISPR-Cas9 are being studied for their ability to correct genetic abnormalities and prevent tumor progression.
- Targeted Molecular Therapy: Therapies that inhibit specific molecular pathways involved in OSSN pathogenesis are in the works. These therapies aim to provide a more targeted treatment approach with fewer side effects than traditional chemotherapy.
Effective Ways to Improve and Prevent Ocular Surface Squamous Neoplasia
- Protect Your Eyes From UV Radiation:
- Wear sunglasses that protect against UVA and UVB rays.
- Use a wide-brimmed hat to protect your eyes from direct sunlight.
- Regular Eye Examination:
- Get regular eye exams, especially if you have risk factors like prolonged sun exposure or immunosuppression.
- Early detection and treatment of pre-cancerous lesions can help to prevent OSSN from progressing further.
- Managing Chronic Inflammation:
- Treat and manage chronic inflammatory eye conditions, such as atopic keratoconjunctivitis.
- Follow your doctor’s instructions when taking anti-inflammatory medications.
- HPV Vaccine:
- Get an HPV vaccine to lower your risk of developing virus-related cancers.
- Encourage vaccination among eligible individuals in order to reduce the prevalence of HPV-related diseases.
- Avoid Immunosuppression.
- Keep your immune system healthy by treating conditions that cause immunosuppression, such as HIV/AIDS.
- Follow your doctor’s recommendations for immunosuppressive medications.
- Avoid smoking:
- Quit smoking and avoid secondhand smoke.
- Smoking is an established risk factor for a variety of cancers, including OSSN.
- Keep a Healthy Diet:
- Eat a diet high in antioxidants, vitamins, and minerals to promote eye health.
- Foods high in vitamins A, C, and E, as well as omega-3 fatty acids, can help prevent eye disease.
Trusted Resources
Books
- “Clinical Ophthalmic Oncology: Conjunctival and Eyelid Tumors” by Arun D. Singh
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
- “The Eye: Basic Sciences in Practice” by John V. Forrester, Andrew D. Dick, Paul G. McMenamin, and William R. Lee
Online Resources
- American Academy of Ophthalmology (AAO)
- National Eye Institute (NEI)
- Ocular Surface Society of Optometry (OSSO)
- World Health Organization (WHO) – Eye Health
- PubMed – OSSN Research