What is Optic Nerve Hypoplasia?
Optic nerve hypoplasia (ONH) is a congenital disorder characterized by underdevelopment of the optic nerve, which transmits visual information from the eyes to the brain. This developmental anomaly can result in a reduction in the number of optic nerve fibers, causing varying degrees of visual impairment. ONH is frequently associated with other neurological and endocrine abnormalities, making it a complicated and multifaceted condition that necessitates thorough evaluation and management.
Detailed Examination of Optic Nerve Hypoplasia
Anatomy and Development
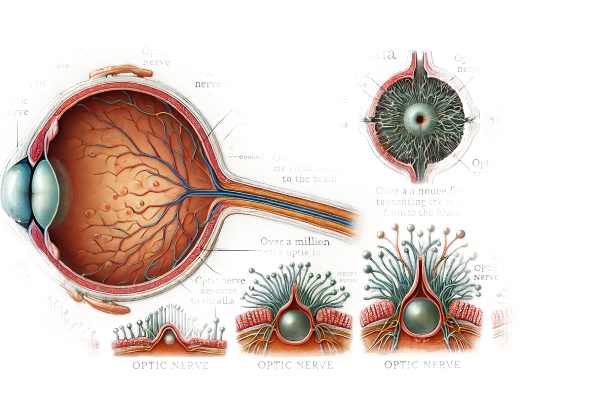
The optic nerve is essential for vision because it contains over a million nerve fibers that transmit visual signals from the retina to the brain. During fetal development, these nerve fibers multiply and form a fully functional optic nerve. When this process is disrupted, the optic nerve shrinks and develops less than it should.
Causes and Risk Factors
The exact cause of optic nerve hypoplasia is unknown, but it is believed to result from a combination of genetic and environmental factors:
- Genetic factors:
- Certain genetic mutations and hereditary conditions may predispose people to ONH. However, most cases are sporadic and lack a clear genetic link.
- Environmental factors:
- Maternal health and environmental exposures during pregnancy are important factors. Maternal diabetes, alcohol consumption, drug use, and toxin exposure have all been linked to the development of ONH.
- Intrauterine Growth Restrictions:
- Conditions that limit fetal growth and development can disrupt the formation of the optic nerve, resulting in hypoplasia.
- Infections:
- Maternal infections, such as rubella or toxoplasmosis, during pregnancy can disrupt the normal development of the fetal optic nerve.
Clinical Presentation
The severity of visual impairment in optic nerve hypoplasia varies greatly according to the extent of optic nerve underdevelopment. Clinical features may include:
- Visual acuity loss:
- Reduced visual acuity is a common symptom, which can range from minor blurring to complete vision loss. Certain individuals may be legally blind.
- Nystagmus:
- Individuals with ONH frequently experience involuntary eye movements known as nystagmus. This condition may impair visual stability and clarity.
- Strabismus:
- Eye misalignment, or strabismus, is frequently associated with ONH, resulting in difficulties with binocular vision and depth perception.
- Optical Disc Anomalies:
- The optic disc, which is where the optic nerve enters the eye, may appear abnormally small or pale when examined, indicating that the optic nerve is underdeveloped.
Associated Conditions
Optic nerve hypoplasia is frequently part of a broader set of neurological and endocrine abnormalities known as septo-optic dysplasia (SOD) or de Morsier syndrome. Associated conditions include:
- Midline brain abnormalities:
- Many ONH patients have abnormalities in the brain’s midline structures, including the corpus callosum and septum pellucidum. These abnormalities can result in a variety of neurological deficits.
- Hypopituitarism:
- The pituitary gland, which regulates a variety of hormones, is frequently underdeveloped in ONH patients. This can lead to hypopituitarism, which is characterized by a lack of one or more pituitary hormones that affects growth, metabolism, and sexual development.
- Developmental delays:
- Children with ONH may have developmental delays and cognitive impairments as a result of associated brain abnormalities.
Differential Diagnosis
Several conditions can cause symptoms similar to optic nerve hypoplasia, necessitating a careful differential diagnosis.
- Optical Neuritis:
- Optic nerve inflammation, which is most commonly associated with multiple sclerosis, can result in acute vision loss and optic disc swelling. Differentiation is based on clinical history, MRI findings, and corticosteroid response.
- Congenital Optic Nerve Atrophy:
- This condition is characterized by primary degeneration of the optic nerve fibers, resulting in optic disc pallor and vision loss. It differs from ONH in that there is no optic disc hypoplasia on fundoscopy.
- Leber’s Hereditary Optic Neuropathy (LHON):
- A mitochondrial disorder that causes bilateral vision loss, particularly in young adults. Genetic testing can help confirm the diagnosis and distinguish it from ONH.
Prognosis
The prognosis for people with optic nerve hypoplasia varies depending on the severity of the condition and the presence of other abnormalities. While vision loss in ONH is usually permanent, early intervention and supportive care can greatly improve quality of life and developmental outcomes. Regular monitoring and multidisciplinary management are required to meet the complex needs of people with ONH and associated conditions.
Methods to Diagnose Optic Nerve Hypoplasia
Diagnosing optic nerve hypoplasia necessitates a multifaceted approach that includes clinical evaluation, imaging studies, and endocrine assessments.
Clinical Evaluation
- Ophthalmological Examination:
- Visual Acuity Testing: This is an important initial assessment to determine the severity of visual impairment. Depending on the patient’s age and cooperation, a variety of tools can be used, such as Snellen charts or age-appropriate visual acuity tests.
- Fundoscopy: Direct examination of the optic disc is required. To visualize the optic disc, use an ophthalmoscope or a slit-lamp biomicroscope equipped with a fundus lens. The presence of a small, pale optic disc indicates optic nerve hypoplasia.
- Pupil Reactions: Assessing the pupil’s response to light can aid in the identification of afferent pupillary defects. An abnormal response may indicate optic nerve dysfunction.
- Neurological assessment:
- A comprehensive neurological evaluation is required to detect any associated brain abnormalities or developmental delays. This includes a thorough medical history, evaluation of developmental milestones, and a neurological exam.
Imaging Studies
- Magnetic Resonance Imaging(MRI):
- MRI is the preferred imaging modality for diagnosing optic nerve hypoplasia. It provides detailed images of the brain and optic nerves, which aid in the identification of structural abnormalities. MRI can detect midline brain defects, such as agenesis of the corpus callosum or the absence of the septum pellucidum, which are frequently associated with ONH.
- Contrast-enhanced MRI can provide additional information about the optic nerves and surrounding structures, assisting in the elimination of other conditions such as tumors or inflammatory processes.
- Optical Coherence Tomography (OCT):
- OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve head. It can aid in determining the thickness of the retinal nerve fiber layer, providing objective evidence of optic nerve hypoplasia.
Endocrine Evaluation
- Hormone Level Test:
- Given the link between ONH and hypopituitarism, comprehensive endocrine testing is required. Blood tests to determine levels of key hormones such as growth hormone, thyroid-stimulating hormone, cortisol, and sex hormones are required to assess pituitary function.
- An endocrinologist may perform additional tests, such as stimulation tests, to determine the pituitary gland’s functional capacity.
- Bone Age Assessment:
- A bone age assessment in children using a hand and wrist X-ray can help determine growth delays and the need for growth hormone therapy.
Treatment Options for Optic Nerve Hypoplasia
Standard Treatment Options
Optic nerve hypoplasia (ONH) is a congenital condition that has no cure, but there are several treatment options that can help manage symptoms, improve visual function, and address associated endocrine and neurological issues.
- Visual rehabilitation:
- Low Vision Aids: Patients with significant vision impairment may benefit from low vision aids such as magnifying glasses, telescopic lenses, and electronic devices that improve visual function.
- Vision Therapy: Customized vision therapy programs can help children improve their visual skills and coordination, particularly those with associated conditions such as strabismus or nystagmus.
- Management of the associated endocrine abnormalities:
- Hormone Replacement Therapy: Hormone replacement therapy is essential for patients suffering from hypopituitarism. Depending on the specific deficiencies identified, this may include replacements for growth hormone, thyroid hormone, cortisol, and sex hormone.
- Regular Endocrine Monitoring: Endocrinologists must continuously monitor and adjust hormone therapy to ensure optimal growth, development, and metabolic function.
- Neurological and developmental support:
- Early Intervention Programs: Children with ONH frequently benefit from early intervention services, such as physical, occupational, and speech therapy, to address developmental delays and improve functional outcomes.
- Special Education Services: Individualized education plans (IEPs) and special education services can help children with ONH meet their unique learning needs, ensuring they receive the necessary support at school.
Innovative and Emerging Therapies
- Genetic Therapy:
- Gene therapy, while still in the experimental stage, shows promise for treating the genetic causes of ONH. Researchers are looking into techniques for correcting genetic mutations that cause problems with optic nerve development, which could lead to a new treatment option.
- Stem Cell Treatment:
- Stem cell research is another emerging field that could benefit ONH. Researchers are looking into the use of stem cells to regenerate damaged optic nerve fibers and improve visual function. While still in the research phase, this approach has the potential to revolutionize treatment options for congenital optic nerve disorders.
- Neuroprotective Agents:*
- Neuroprotective drugs work to preserve the remaining optic nerve fibers and prevent further damage. Citicoline and brimonidine are being investigated for their ability to improve neural function and protect against optic nerve degeneration.
Supportive Care
- Psychological support:
- Living with a lifelong visual impairment and related conditions can be difficult. Psychological support and counseling for patients and their families can help address emotional and mental health concerns, as well as provide stress-management strategies and improve quality of life.
- Assistive Technology:
- Advances in assistive technology, such as screen readers, text-to-speech software, and adaptive computer interfaces, can greatly improve the independence and functionality of people with ONH.
- Social Support Network:
- Participating in support groups and communities for people with visual impairments and their families can provide important resources, shared experiences, and emotional support.
Monitoring and Follow-up
Regular follow-up with a multidisciplinary team, including ophthalmologists, endocrinologists, neurologists, and developmental specialists, is critical for monitoring the patient’s condition, managing associated abnormalities, and adjusting treatment plans as needed.
Effective Ways to Improve and Prevent Optic Nerve Hypoplasia
- Pre-natal Care:
- Get regular prenatal checkups and live a healthy lifestyle while pregnant. Proper prenatal care can help prevent conditions that could lead to ONH.
- Avoiding Teratogenic Substances:
- Pregnant women should avoid alcohol, drugs, and other harmful substances that can impair fetal development and potentially cause optic nerve hypoplasia.
- Controlling Maternal Diabetes:
- Proper management of maternal diabetes during pregnancy can lower the risk of developmental abnormalities, including ONH.
- Early detection:
- Early diagnosis and intervention are critical. Routine eye examinations for infants and young children can help detect ONH and other visual impairments early on, allowing for timely treatment.
- Regular monitoring:
- For children with ONH, regular follow-up with healthcare providers, such as ophthalmologists and endocrinologists, is critical to monitor progress and adjust treatments as needed.
- Educational support:
- Collaborate with early intervention and special education programs to meet the developmental and educational needs of children with ONH.
- A Healthy Lifestyle:
- Maintain a well-balanced diet, engage in regular physical activity, and avoid smoking to improve overall health and potentially reduce the risk of future complications.
- Awareness & Advocacy:
- Raise awareness of ONH and advocate for research and resources to help people with the condition and their families.
- Family Support:
- Participate in family support groups and counseling to share experiences, gain insights, and receive emotional and practical assistance with managing ONH.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright
- “Genetic Disorders and the Eye” by Elias I. Traboulsi






