What is pediatric glaucoma?
Pediatric glaucoma, also known as congenital glaucoma, is a rare but severe eye condition that affects infants and young children. It is defined by an increase in intraocular pressure (IOP) within the eye, which, if left untreated, can damage the optic nerve and result in vision loss. Unlike adult glaucoma, which usually develops gradually over time, pediatric glaucoma can appear at birth or soon after, necessitating early detection and treatment to preserve vision.
Types of Pediatric Glaucoma
There are several types of pediatric glaucoma, each with different causes and clinical features:
Primary Congenital Glaucoma (PCG): This type results from abnormal development of the eye’s drainage system during fetal development. It is the most common type of pediatric glaucoma, usually diagnosed within the first year of life. PCG is frequently bilateral (affecting both eyes) and may have a genetic component, with specific gene mutations linked to the condition.
Secondary Pediatric Glaucoma: This type develops as a result of another eye condition or systemic disease. Trauma, inflammation, tumors, and previous eye surgery are all possible causes. Secondary glaucoma can appear at any age in childhood and is frequently associated with other ocular or systemic abnormalities.
Juvenile Open-Angle Glaucoma: This type is similar to adult open-angle glaucoma, but it affects older children and teenagers. It is usually inherited in an autosomal dominant manner, which means that a single copy of the altered gene can cause the disease. Juvenile open-angle glaucoma develops more slowly than congenital glaucoma, but it still necessitates close monitoring and treatment.
Causes and Risk Factors
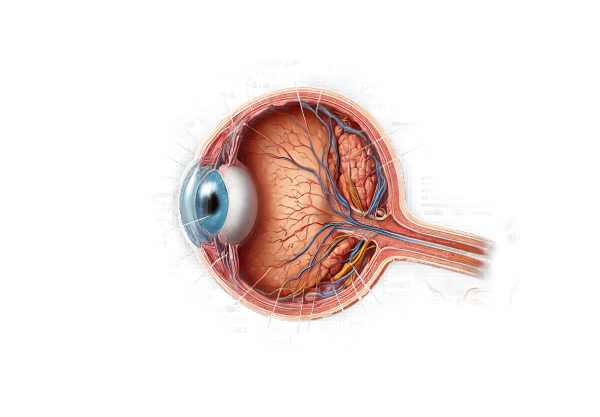
The primary cause of pediatric glaucoma is a problem with the eye’s aqueous humor drainage system. In a healthy eye, the ciliary body produces aqueous humor, which flows through the pupil into the anterior chamber before draining through the trabecular meshwork and Schlemm’s canal. In pediatric glaucoma, this drainage pathway becomes obstructed or malformed, resulting in fluid accumulation and elevated intraocular pressure.
Genetic Factors: Genetic mutations are responsible for a large number of cases of primary congenital glaucoma. Mutations in the CYP1B1 gene, for example, can result in abnormal development of the trabecular meshwork and Schlemm’s canal. These genetic factors are inherited, and a family history of glaucoma raises the risk.
Systemic Conditions: Some systemic diseases and syndromes increase the risk of secondary pediatric glaucoma. Sturge-Weber syndrome, neurofibromatosis, and Marfan syndrome can all have an impact on the structure and function of the eye, resulting in high intraocular pressure levels.
Ocular Conditions: Uveitis (inflammation of the uveal tract), retinopathy of prematurity, and congenital cataracts can all increase a child’s risk of developing glaucoma. Glaucoma can develop after eye surgery or trauma.
Symptoms
The symptoms of pediatric glaucoma vary depending on the age of onset and severity of the disease. In infants and young children, the signs can be subtle and easily missed, making early detection difficult. Common symptoms include:
Excessive Tearing: One of the first symptoms of pediatric glaucoma is excessive tearing (epiphora). This happens because the increased intraocular pressure irritates the cornea and causes tear production.
Light Sensitivity: Children with glaucoma frequently experience photophobia, or sensitivity to light. Elevated intraocular pressure causes corneal edema (swelling), which causes this symptom.
Enlarged Eyes: Buphthalmos, or enlargement of the eyeball, is a sign of advanced pediatric glaucoma. The increased pressure causes the sclera (the white part of the eye) to stretch, giving it an enlarged appearance.
Cloudy Cornea: Edema can cause the cornea to become cloudy or hazy, resulting in a milky appearance. This is frequently associated with visible corneal opacities.
Frequent Eye Rubbing: Glaucoma-affected infants and young children may frequently rub their eyes due to discomfort and irritation caused by high intraocular pressure.
Poor Vision: As the optic nerve deteriorates, children with glaucoma may experience difficulty focusing on objects, poor eye contact, or a lack of visual response to stimuli.
Impact on Vision
The increased intraocular pressure in pediatric glaucoma can cause irreversible damage to the optic nerve, resulting in progressive vision loss. The extent of vision impairment is determined by the age at diagnosis, the severity of the condition, and the timing of treatment. If left untreated, pediatric glaucoma can lead to blindness.
Early intervention is critical for preserving vision. Regular monitoring and treatment can help control intraocular pressure and protect the optic nerve from further damage. Even with the best possible management, some children may continue to have visual deficits.
Psychological and Social Implications
Living with pediatric glaucoma can have a significant psychological and social impact on both the child and the family. The chronic nature of the condition, the need for frequent medical visits, and the possibility of visual impairment can all cause emotional stress and anxiety.
Children with visual impairments may struggle in their academic and social development. They may need special educational support and accommodations to succeed academically. Children with visual impairments may struggle with activities that require good vision, such as sports and games, which can have an impact on their social interactions.
Parents and caregivers play an important role in managing pediatric glaucoma. They must be vigilant in identifying symptoms, enforcing treatment regimens, and providing emotional support. Support groups and counseling can be invaluable resources for families dealing with the difficulties of pediatric glaucoma.
Long-Term Outlook
The long-term prognosis for children with pediatric glaucoma is determined by a number of factors, including the type and severity of the disease, the efficacy of treatment, and the presence of any associated conditions. Many children with pediatric glaucoma can have good visual outcomes and live fulfilling lives with early detection and treatment.
However, lifelong monitoring and follow-up care are required. Regular eye exams and intraocular pressure measurements are required to detect any changes in the condition and adjust treatment accordingly. Advances in medical and surgical treatments are improving the prognosis for children with pediatric glaucoma, providing hope for better outcomes and quality of life.
Diagnostic methods
A comprehensive approach is required to diagnose pediatric glaucoma, which includes clinical examinations, imaging techniques, and, in some cases, genetic testing. Early and accurate diagnosis is critical for starting appropriate treatment and avoiding vision loss.
Clinical Examination
History and Symptoms: The first step in diagnosing pediatric glaucoma is to take a thorough medical history and review the symptoms. Parents and caregivers should report any signs of excessive tearing, light sensitivity, enlarged eyes, or a cloudy cornea in their child.
Visual Acuity Testing: Measuring visual acuity in young children is difficult, but it provides valuable information about the child’s vision. Visual function can be evaluated using age-appropriate methods like preferential looking tests or visual evoked potentials.
Intraocular Pressure Measurement: Determining intraocular pressure (IOP) is critical for diagnosing glaucoma. Applanation tonometry, rebound tonometry, and pneumotonometry are some of the techniques available. To obtain accurate measurements in young children, sedation or general anesthesia may be necessary.
Ophthalmoscopy
Ophthalmoscopy examines the eye’s interior structures, particularly the optic nerve head. Direct or indirect ophthalmoscopy allows the clinician to examine the optic disc for cupping, pallor, and nerve fiber layer thinning, all of which indicate glaucoma damage.
Gonioscopy
Gonioscopy is a technique for examining the anterior chamber angle, which contains the eye’s drainage system. This procedure aids in the identification of any structural abnormalities that may be causing impaired aqueous humor outflow. Gonioscopy is especially effective at distinguishing between primary congenital glaucoma and secondary glaucoma caused by other conditions.
Imaging Techniques
Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve head. It is useful for identifying early changes in the retinal nerve fiber layer and tracking disease progression.
Ultrasound Biomicroscopy (UBM): UBM employs high-frequency ultrasound to visualize anterior segment structures such as the drainage angle and ciliary body. It is useful for detecting anatomical abnormalities and planning surgical procedures.
Genetic Testing
Genetic testing may be performed if glaucoma runs in the family or if genetic mutations are suspected. Identifying specific gene mutations, such as those in the CYP1B1 gene, can help confirm the diagnosis and guide treatment plans.
Additional Tests
Corneal Diameter Measurement: Measuring the corneal diameter can reveal the presence of buphthalmos, a feature of advanced pediatric glaucoma.
Pachymetry: Pachymetry measures corneal thickness, which can affect intraocular pressure readings and aid in the differentiation of various types of glaucoma.
Electrophysiological Tests: These tests, such as visual evoked potentials (VEP) and electroretinography (ERG), assess the functional integrity of the visual pathway and can aid in determining visual function in young children.
Effective Treatments for Pediatric Glaucoma
The goal of pediatric glaucoma treatment is to lower intraocular pressure (IOP) in order to protect the optic nerve and maintain vision. The treatment approach varies depending on the type and severity of the glaucoma, as well as the child’s age and general health. Here are the main treatment options:
Medications
Medications are frequently the first line of treatment for pediatric glaucoma. They help to lower intraocular pressure by either decreasing aqueous humor production or increasing its outflow. Common types of medications are:
Beta-blockers: These inhibit the production of aqueous humor. Examples include timolol and betaxolol. Beta-blockers are usually well tolerated, but they can cause fatigue, bradycardia, and respiratory problems in some children.
Prostaglandin Analogues: These promote the flow of aqueous humor. Latanoprost and bimatoprost are two commonly used prostaglandin analogues. They are generally effective and have fewer systemic side effects, but they can cause local side effects such as increased eye redness and eyelash lengthening.
Carbonic Anhydrase Inhibitors: These suppress the production of aqueous humor. Orally (e.g., acetazolamide) or as eye drops (e.g., dorzolamide). With oral formulations, potential side effects include gastrointestinal upset and metabolic acidosis.
Alpha Agonists: These reduce aqueous humor production while increasing outflow. Brimonidine is a commonly used alpha agonist. Possible side effects include drowsiness, fatigue, and allergic reactions.
Surgical Treatment
When medications fail to control intraocular pressure, surgical intervention may be required. Several surgical procedures are available, each with their own indications and potential benefits:
Goniotomy: This procedure involves making an opening in the trabecular meshwork to allow aqueous humor outflow. It is especially effective in infants with primary congenital glaucoma.
Trabeculotomy: Trabeculotomy, like goniotomy, involves opening the trabecular meshwork, but it is usually used when goniotomy fails or is not feasible. It is possible to perform it alongside other surgeries.
Trabeculectomy: This procedure removes a portion of the trabecular meshwork and adjacent structures, resulting in a new drainage pathway for aqueous humor. It is commonly used in cases of refractory glaucoma.
Glaucoma Drainage Devices: These devices, such as the Ahmed valve or Baerveldt implant, are inserted to provide an alternative drainage route for aqueous humor. They are used in complex cases where other surgical procedures have failed or are not appropriate.
Cyclophotocoagulation: This laser procedure targets the ciliary body and reduces aqueous humor production. It can be used when other surgical options are ineffective or have been exhausted.
Lifestyle and Supportive Measures
In addition to medical and surgical treatments, supportive measures and lifestyle changes can help manage pediatric glaucoma.
Regular Monitoring: Frequent follow-up visits with an ophthalmologist are required to monitor intraocular pressure, assess optic nerve health, and adjust treatment as necessary.
Visual Rehabilitation: Children with glaucoma-related visual impairments may benefit from visual rehabilitation services such as low vision aids, educational support, and occupational therapy.
Parental Support and Education: Effective management requires educating parents and caregivers about the condition, treatment options, and the importance of adhering to therapy.
Frequently Asked Questions About Pediatric Glaucoma
What Causes Pediatric Glaucoma?
An abnormality in the eye’s drainage system causes pediatric glaucoma, which raises intraocular pressure. It can be congenital (present at birth) due to genetic or developmental abnormalities, or it can be the result of trauma, inflammation, or systemic disease.
How is Pediatric Glaucoma Diagnosed?
Pediatric glaucoma is diagnosed using a variety of clinical examinations, including visual acuity testing, intraocular pressure measurement, ophthalmoscopy, gonioscopy, and imaging techniques such as OCT and ultrasound biomicroscopy. In some cases, genetic testing may be required.
Is it possible to cure pediatric glaucoma?
While there is no cure for pediatric glaucoma, it can be effectively managed with timely diagnosis and treatment. The goal is to reduce intraocular pressure, protect the optic nerve, and preserve vision. Lifelong monitoring and treatment may be required.
What are the signs of pediatric glaucoma?
Pediatric glaucoma symptoms include excessive tearing, light sensitivity, enlarged eyes (buphthalmos), a cloudy cornea, frequent eye rubbing, and poor vision. Early symptoms can be subtle, so regular eye exams are essential for early detection.
What are the treatments for pediatric glaucoma?
Medications to lower intraocular pressure, surgical procedures like goniotomy, trabeculotomy, trabeculectomy, and glaucoma drainage devices, and laser treatments like cyclophotocoagulation are all options for treatment. The type and severity of glaucoma, as well as the child’s overall health, determine the course of treatment.
Is pediatric glaucoma hereditary?
Pediatric glaucoma may have a genetic component. Primary congenital glaucoma is frequently associated with mutations in genes such as CYP1B1. A family history of glaucoma can increase the risk, and affected families may benefit from genetic testing.
How Does Pediatric Glaucoma Affect Vision?
If left untreated, pediatric glaucoma can permanently damage the optic nerve, resulting in progressive vision loss and, potentially, blindness. Early diagnosis and treatment are critical for preserving vision.
What resources are available for children with pediatric glaucoma?
Regular ophthalmologic care, visual rehabilitation services, educational accommodations, and family support groups are all options for assistance. Effective management of the condition requires parental education and involvement.
Can lifestyle changes help treat pediatric glaucoma?
Lifestyle changes, such as keeping a healthy weight and avoiding activities that raise intraocular pressure, can help. Regular follow-up visits and adherence to treatment plans are critical for successful management.
Are there support groups for families whose children have pediatric glaucoma?
Yes, there are support groups and organizations that help families deal with pediatric glaucoma. These groups provide useful information, emotional support, and practical advice.
Trusted Resources and Support
Books and Organizations
Books:
- “Pediatric Ophthalmology and Strabismus”* by Kenneth W. Wright and Yi Ning J. Strube.
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care”* by Paul N. Schacknow and John R. Samples.
Organizations:
- The American Association for Pediatric Ophthalmology and Strabismus (AAPOS): Provides information and resources on pediatric eye conditions, including glaucoma.
- The Glaucoma Research Foundation offers education, support, and research funding for all types of glaucoma.
- National Eye Institute (NEI): The NEI, which is part of the National Institutes of Health (NIH), provides comprehensive information on eye health and diseases, including pediatric glaucoma.
Financial Aid Options
Insurance Coverage: Most health insurance policies cover the diagnosis and treatment of pediatric glaucoma. Parents should double-check the coverage details with their insurance provider.
Patient Assistance Programs: Pharmaceutical companies may provide patient assistance programs to help eligible patients cover the cost of medications. Programs like RxAssist provide information on such resources.
Non-Profit Organizations: The HealthWell Foundation and the Children’s Health Fund provide financial assistance for medical expenses, including treatments for pediatric glaucoma.
Government Programs: Medicaid and the Children’s Health Insurance Program (CHIP) offer coverage to low-income families. These programs can help cover the costs of treating and caring for children with glaucoma.






