What is the definition of phacoanaphylactic endophthalmitis?
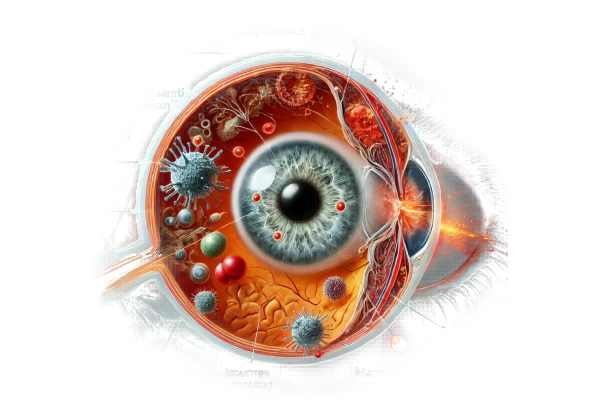
Phacoanaphylactic endophthalmitis, also known as lens-induced uveitis, is an uncommon but severe inflammatory condition of the eye. It occurs as an immune response to lens proteins exposed to the intraocular environment, usually as a result of trauma or surgery that disrupts the lens capsule. This exposure causes an autoimmune reaction in which the body mounts an inflammatory response against its own lens proteins, resulting in endophthalmitis, an inflammation of the internal coats of the eye. Understanding the pathophysiology, causes, and clinical manifestations of phacoanaphylactic endophthalmitis is critical for early diagnosis and treatment.
Pathophysiology
The lens of the eye is normally encapsulated, and its proteins are isolated from the immune system. When the lens capsule ruptures, lens proteins enter the intraocular space. The immune system, which has not previously encountered these proteins, recognizes them as foreign antigens and initiates an immune response. This response activates both the innate and adaptive immune systems, resulting in the recruitment of inflammatory cells like macrophages and lymphocytes.
The inflammation primarily affects the uvea, which includes the iris, ciliary body, and choroid, but it can spread to the vitreous and retina. This inflammatory cascade causes the typical signs and symptoms of phacoanaphylactic endophthalmitis, which include pain, redness, and vision loss.
Causes
Phacoanaphylactic endophthalmitis is typically associated with:
Trauma: Penetrating eye injuries that disrupt the lens capsule may expose lens proteins to the immune system, triggering an inflammatory response.
Surgery: Intraocular surgeries, particularly cataract extraction or intraocular lens implantation, can occasionally rupture the lens capsule, exposing lens proteins.
Spontaneous Rupture: Although uncommon, spontaneous rupture of the lens capsule can occur, especially in cases of advanced cataracts or in eyes with pre-existing conditions that weaken capsule integrity.
Symptoms
The symptoms of phacoanaphylactic endophthalmitis can vary in severity, but they typically include:
Pain: Patients frequently experience severe ocular pain as a result of the intense inflammatory response.
Redness: The affected eye is usually red and inflamed, with conjunctival hyperemia.
Vision Loss: The condition is characterized by rapid and significant vision loss as a result of both inflammation and potential secondary complications such as glaucoma or retinal involvement.
Photophobia: Light sensitivity is common, as the inflamed eye reacts to bright light.
Floaters: Patients may notice floaters caused by inflammatory cells and debris in the vitreous.
Swelling: The extensive inflammation may cause swelling of the eyelids and surrounding tissues.
Differential Diagnosis
Other causes of intraocular inflammation and infection, such as:
Infectious Endophthalmitis: This is the most common type of endophthalmitis, which is caused by a bacterial or fungal infection after surgery or trauma. Infectious endophthalmitis frequently presents with similar symptoms, but it has a distinct etiology and requires separate treatment.
Autoimmune Uveitis: A variety of autoimmune diseases can cause uveitis, which is an inflammation of the uveal tract. While these conditions can look similar, they are not caused by lens protein exposure and may have systemic symptoms.
Lens Particle Uveitis: This condition occurs when lens particles enter the eye, usually after surgery. It is less severe than phacoanaphylactic endophthalmitis and does not elicit as strong an immune response.
Complications
If left untreated, phacoanaphylactic endophthalmitis can cause a number of serious complications, including:
Glaucoma: Inflammation-induced increased intraocular pressure can progress to secondary glaucoma, resulting in additional vision loss.
Retinal Detachment: Severe inflammation can cause traction on the retina, potentially resulting in retinal detachment that necessitates surgical intervention.
Permanent Vision Loss: Chronic inflammation and the resulting damage to intraocular structures can lead to irreversible vision loss.
Phthisis Bulbi: In severe cases, the eye can atrophy and shrink, resulting in a condition known as phthisis bulbi.
Psychological and Social Implications
The onset of severe symptoms and the possibility of significant vision loss can have serious psychological and social consequences. Patients may experience anxiety, depression, and a loss of independence as a result of poor vision. This can have an impact on their ability to work, drive, and perform daily tasks. Early detection and treatment are critical not only for maintaining vision, but also for mitigating the psychological and social consequences.
Prognosis
The prognosis for phacoanaphylactic endophthalmitis is determined by the timing of diagnosis and the efficacy of treatment. Early intervention with appropriate therapy can result in a positive outcome, with inflammation reduced and vision preserved. However, delaying treatment can lead to serious complications, including permanent vision loss. Regular follow-up and monitoring are required to effectively manage the condition and prevent recurrences.
Techniques to Diagnose Phacoanaphylactic Endophthalmitis
A comprehensive clinical evaluation is required to diagnose phacoanaphylactic endophthalmitis, which includes a patient history, physical examination, and specialized diagnostic testing. Accurate and timely diagnosis is critical for distinguishing this condition from other causes of endophthalmitis and initiating appropriate treatment.
Clinical Examination
Patient History: A thorough medical history is required to identify potential triggers such as recent eye trauma or surgery. Patients may experience sudden onset of pain, redness, and vision loss, usually following a known inciting event.
Slit Lamp Examination: A thorough slit lamp examination allows for visualization of the anterior segment of the eye, revealing signs of inflammation such as keratic precipitates, anterior chamber cells, flare, and iris nodules. This examination can also detect any residual lens material or lens capsule disruption.
Fundoscopy: A dilated fundus examination is done to evaluate the posterior segment of the eye. This can reveal vitritis (vitreal inflammation), retinal vasculitis, and other signs of intraocular inflammation.
Imaging Techniques
Ultrasound B-Scan: When media opacities (such as dense corneal edema or hypopyon) prevent adequate visualization of the posterior segment, a B-scan ultrasound can provide useful data. This imaging technique can detect vitreous opacities, retinal detachment, and other posterior segment abnormalities.
Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve. It is useful for detecting macular edema, retinal thickening, and other structural changes caused by inflammation.
Lab Tests
Anterior Chamber Paracentesis: In some cases, sampling the aqueous humor with an anterior chamber paracentesis can yield diagnostic information. The fluid can be examined for inflammatory cells, and microbiological cultures can aid in ruling out infectious causes of endophthalmitis.
Vitreous Tap and Biopsy: In cases of significant vitreous involvement, a vitreous tap or biopsy may be required. To differentiate between phacoanaphylactic and infectious endophthalmitis, the vitreous sample can be tested for inflammatory markers, lens proteins, and pathogens.
Blood Tests: Systemic blood tests, such as a complete blood count (CBC) and inflammatory markers (e.g., C-reactive protein and erythrocyte sedimentation rate), can help assess overall inflammatory status and rule out systemic infection.
Differential Diagnosis
Infectious Endophthalmitis: Distinguishing between phacoanaphylactic and infectious endophthalmitis is critical, and microbiological cultures and sensitivity testing are usually required. Infectious endophthalmitis frequently presents with a more aggressive clinical course, necessitating targeted antimicrobial therapy.
Autoimmune Uveitis: Sarcoidosis, Behçet’s disease, and Vogt-Koyanagi-Harada disease can all result in intraocular inflammation. Systematic evaluation and laboratory tests can aid in the identification of these conditions and their appropriate management.
Lens Particle Uveitis: This condition results from the presence of lens particles in the anterior chamber after surgery. It is generally less severe than phacoanaphylactic endophthalmitis and can be distinguished by clinical history and examination results.
Phacoanaphylactic Endophthalmitis Treatment
The treatment for phacoanaphylactic endophthalmitis focuses on reducing inflammation, avoiding complications, and preserving vision. A multidisciplinary approach is frequently required, involving ophthalmologists, immunologists, and, on occasion, infectious disease specialists. Here are the primary treatment strategies:
Corticosteroids
Topical Corticosteroids: These are the primary treatment options for reducing anterior segment inflammation. Prednisolone acetate or dexamethasone eye drops are commonly used, with the dosage varying according to the severity of inflammation. Initially, frequent administration may be required, with the frequency decreasing as the condition improves.
Systemic Corticosteroids: In cases of severe or posterior segment involvement, systemic corticosteroids such as oral prednisone or intravenous methylprednisolone may be required. These aid in reducing the overall inflammatory response and managing more severe inflammation.
Periocular Steroid Injections: When topical or systemic steroids do not effectively control inflammation, periocular (sub-Tenon’s) steroid injections can be used. These deliver high concentrations of corticosteroids directly to the affected area.
Immunosuppressive Therapy
Immunosuppressive agents may be used in refractory cases, when corticosteroids are contraindicated or insufficient. Methotrexate, cyclosporine, and azathioprine are medications that can help control the immune system and reduce inflammation.
Surgical Intervention
Lens Removal (Lensectomy): If significant lens material remains or if the lens is causing ongoing inflammation, surgical removal of the lens (lensectomy) may be required. This procedure helps to eliminate the antigenic stimulus and can reduce inflammation.
Vitrectomy: A pars plana vitrectomy may be performed in cases of severe vitreous involvement or to remove inflammatory debris. This surgery involves removing the vitreous gel and cleaning the intraocular space to reduce inflammation and prevent complications.
Management of Complications
Glaucoma Management: Inflammation can cause increased intraocular pressure and lead to glaucoma. Beta-blockers, alpha agonists, and carbonic anhydrase inhibitors are examples of antiglaucoma medications. In severe cases, surgical intervention such as trabeculectomy or the implantation of drainage devices may be required.
Retinal Detachment Repair: If a retinal detachment occurs, immediate surgical intervention is required. Pneumatic retinopexy, scleral buckling, and vitrectomy with membrane peeling are some of the techniques used to reattach the retina and preserve vision.
Supportive Care
Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) or other analgesics can be used to alleviate inflammation-related pain and discomfort.
Patient Education: Educating patients about the condition, the importance of following treatment regimens, and recognizing signs of complications is critical for successful management.
Common Questions About Phacoanaphylactic Endophthalmitis
What is Phacoanaphylactic Endophthalmitis?
An immune response to lens proteins causes phacoanaphylactic endophthalmitis, an inflammatory condition of the eye. It typically occurs after trauma or surgery that disrupts the lens capsule, exposing lens proteins and causing inflammation.
How Is Phacoanaphylactic Endophthalmitis Diagnosed?
The diagnosis is based on a patient history, clinical examination, and diagnostic tests. To analyze inflammatory cells and rule out infection, key methods include slit lamp examination, fundoscopy, ultrasound B-scan, and, on occasion, anterior chamber paracentesis or vitreous biopsy.
What are the signs of phacoanaphylactic endophthalmitis?
Common symptoms include severe eye pain, redness, vision loss, photophobia, floaters, and swelling of the eyelids and surrounding tissues.
How Is Phacoanaphylactic Endophthalmitis Treated?
Corticosteroids are typically used to control inflammation, and options include topical, systemic, and periocular steroids. In severe cases, immunosuppressive therapy or surgical procedures such as lensectomy or vitrectomy may be necessary.
Can phacoanaphylactic endophthalmitis lead to permanent vision loss?
Yes, if left untreated or delayed, phacoanaphylactic endophthalmitis can cause permanent vision loss due to complications like glaucoma, retinal detachment, or ongoing inflammation that damages intraocular structures.
Is phacoanaphylactic endophthalmitis infectious?
No, phacoanaphylactic endophthalmitis is not caused by an infection, but by an immune response to lens proteins. However, it is important to distinguish it from infectious endophthalmitis, which has similar symptoms but requires different treatment.
How is phacoanaphylactic endophthalmitis prevented?
Preventing phacoanaphylactic endophthalmitis requires careful surgical techniques during eye surgeries to minimize lens capsule disruption and proper management of eye injuries to avoid lens protein exposure.
What should I do if I develop symptoms of phacoanaphylactic endophthalmitis?
If you have severe eye pain, redness, or vision loss, see an ophthalmologist right away, especially if you have had eye trauma or surgery. Early diagnosis and treatment are critical for maintaining vision.
What are the long-term effects of phacoanaphylactic endophthalmitis?
With prompt and effective treatment, many patients can regain their vision. However, some people may develop long-term complications, such as glaucoma or cataract formation, necessitating ongoing management and monitoring.
Does phacoanaphylactic endophthalmitis recur?
Recurrence is uncommon if the inciting lens material is completely removed. However, ongoing monitoring and follow-up care are required to ensure that any new or residual inflammation is addressed promptly.
Trusted Resources and Support
Books and Organizations
Books:
- “Ocular Inflammation and Uveitis” by Jack J. Kanski and Carlos E. Pavesio.
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling.
Organizations:
- The American Academy of Ophthalmology (AAO): Provides extensive information on ocular conditions, including phacoanaphylactic endophthalmitis.
- The Ocular Immunology and Uveitis Foundation: Provides information and support to patients suffering from ocular inflammatory diseases.
- National Eye Institute (NEI): A comprehensive source of information on eye health and disease.
Financial Aid Options
Insurance Coverage: Most health insurance policies cover the diagnosis and treatment of phacoanaphylactic endophthalmitis. Patients should check with their insurance providers to learn about the specifics of their coverage, such as co-pays and deductibles.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations frequently provide patient assistance programs to help with the cost of medications and treatments. Programs such as RxAssist provide information about available resources.
Non-Profit Organizations: Organizations such as the HealthWell Foundation and the Patient Advocate Foundation help patients pay for medical expenses, including treatments for ocular conditions like phacoanaphylactic endophthalmitis.
Government Programs: Medicaid and Medicare offer coverage to eligible individuals. These programs can help cover the costs of treating and caring for phacoanaphylactic endophthalmitis, ensuring that patients receive the medical care they require regardless of their financial situation.










