Eyelid lacerations—cuts or tears in the eyelid tissue—require prompt, precise attention to preserve both function and appearance. These injuries, whether caused by accidents, sharp objects, animal bites, or other trauma, can range from minor superficial splits to deep wounds that threaten the health of the eye itself. Effective management blends immediate first aid, specialized surgical repair, and careful aftercare to reduce the risk of complications such as infection, scarring, or vision loss. This comprehensive guide explores the latest evidence-based therapies, step-by-step management, advanced surgical options, and exciting innovations that are shaping the future of eyelid laceration treatment.
Table of Contents
- Scope and Frequency of Eyelid Lacerations
- First Response and Medical Management
- Operative Repair and Advanced Procedures
- Cutting-Edge Technologies and Recent Advances
- Ongoing Clinical Studies and Anticipated Trends
- Frequently Asked Questions
- Disclaimer
Scope and Frequency of Eyelid Lacerations
Eyelid lacerations represent a significant percentage of facial injuries presenting to emergency rooms and ophthalmology clinics. Understanding who is most at risk, the range of presentations, and underlying anatomical concerns is the first step in delivering optimal care.
Definition and Anatomy
- Eyelid lacerations are tears that may involve the thin skin, muscle, cartilage (tarsus), and even the delicate structures such as the eyelid margin or tear drainage system (canaliculi).
- Injuries can range from minor, partial-thickness cuts to complex, full-thickness or avulsive wounds.
Epidemiology and Demographics
- Prevalence: Eyelid lacerations are more common in children, athletes, those working in construction/agriculture, and individuals exposed to sharp tools or animal bites.
- Incidence: They account for up to 10% of facial lacerations seen in urgent care or ER settings.
- Seasonal trends: Increases during sports seasons, holidays, or in environments with high activity or outdoor risk.
Common Causes
- Blunt trauma: Falls, sports injuries, motor vehicle accidents
- Sharp trauma: Glass, knives, metal, or environmental debris
- Animal and human bites: Dogs, cats, or altercations
- Penetrating objects: Pencils, scissors, or flying debris
Associated Ocular and Facial Injuries
- Globe rupture (eye injury)
- Orbital fractures
- Damage to the tear drainage system
- Concomitant facial, nasal, or forehead wounds
Risk Factors
- Lack of protective eyewear
- High-risk environments (construction, sports)
- Young age or uncoordinated movements in children
- Substance use or risky behavior
Classification of Eyelid Lacerations
- Simple lacerations: Involve only the skin and muscle, away from the eyelid margin.
- Marginal lacerations: Involve the eyelid edge (margin), require precise alignment.
- Canalicular lacerations: Involve the tear drainage ducts; urgent repair is vital.
- Full-thickness lacerations: Traverse the entire lid, potentially exposing the eye or underlying structures.
- Avulsive or tissue-loss injuries: When part of the eyelid is missing or severely damaged.
Initial Assessment and Red Flags
- Check for foreign bodies in the wound or under the lid.
- Look for fat prolapse (indicates deeper injury).
- Suspect globe injury if vision changes, irregular pupil, or severe pain are present.
- Active bleeding, severe swelling, or facial deformity require rapid attention.
Prevention Tips
- Always wear protective eyewear during high-risk activities.
- Childproof sharp objects at home.
- Educate children and workers about eye safety.
First Response and Medical Management
Timely and effective initial management of eyelid lacerations dramatically improves outcomes. First aid should focus on safety, minimizing contamination, and preparing for expert repair.
Immediate First Aid Steps
- Wash hands thoroughly before touching the area.
- Stop bleeding: Apply gentle pressure with a clean, dry cloth or gauze pad.
- Do NOT rub or squeeze the eyelid.
- Rinse the wound gently with sterile saline or clean water to remove dirt or debris.
- Cover with a sterile dressing—avoid adhesive bandages directly on the eyelid.
- Avoid ointments or creams until evaluated by a medical professional.
- Keep the patient calm and avoid movement that could worsen the injury.
When to Seek Emergency Care
- Suspected globe (eyeball) injury: vision loss, bloody tears, irregular pupil, severe pain.
- Heavy bleeding not controlled by pressure.
- Deep, gaping, or contaminated wounds.
- Injuries from animal or human bites (high infection risk).
- Associated facial or skull trauma.
Medical Evaluation Essentials
- Visual acuity testing
- Careful inspection of eyelid layers
- Assessment for canalicular (tear duct) involvement: look for blood at the inner corner or excessive tearing
- Fluorescein staining and slit lamp exam for eye surface injuries
Medical (Non-Surgical) Therapies
- Antibiotics: Topical ointments (e.g., erythromycin) for minor, non-infected wounds. Oral antibiotics for bite injuries, contaminated wounds, or immunocompromised patients.
- Tetanus prophylaxis: Ensure up-to-date tetanus vaccination, especially for dirty or bite-related wounds.
- Pain management: Acetaminophen or prescribed pain relievers; avoid NSAIDs if bleeding risk is high.
- Allergy precautions: Identify possible allergic reactions to topical medications.
- Eye shield: For severe injuries, an eye shield protects from further trauma before surgery.
Monitoring for Complications
- Redness, swelling, pus, fever—may indicate infection.
- Persistent bleeding or hematoma (blood collection).
- Signs of deeper injuries: double vision, restricted eye movement, or excessive tearing.
Advice for Patients and Caregivers
- Avoid eye makeup and contact lenses until cleared by a doctor.
- Clean hands before touching the area.
- Watch for symptoms of infection or unusual discharge.
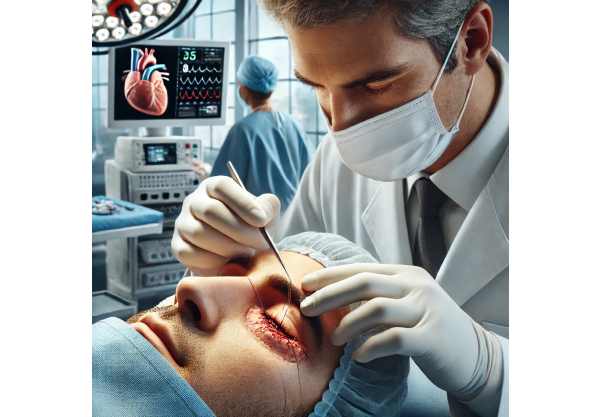
Operative Repair and Advanced Procedures
Surgical repair is often required for eyelid lacerations, especially when the wound is deep, involves the eyelid margin, or disrupts the tear drainage system.
Principles of Eyelid Laceration Surgery
- Precise anatomical alignment: Restoring the normal contour and function is critical to avoid visible scarring, notching, or eyelid dysfunction.
- Layered closure: Skin, muscle, tarsus, and conjunctiva are repaired separately to ensure strength and minimize complications.
- Microsurgical technique: Especially important for canalicular (tear duct) injuries.
Types of Eyelid Laceration Repairs
- Simple primary closure: For clean, linear, partial-thickness wounds away from the margin.
- Complex margin repair: Edges of the eyelid must be perfectly matched and sutured with very fine stitches.
- Canalicular laceration repair: Placement of a tiny silicone stent to keep the tear duct open during healing. Must be done by an oculoplastic or ophthalmic surgeon.
- Full-thickness or tissue-loss repair: May require tissue grafts (from the other eyelid or mouth) or flap reconstruction.
- Management of avulsive injuries: Reconstruction using local, regional, or even free tissue transfer in severe cases.
Suture Materials and Techniques
- Ultra-fine absorbable or non-absorbable sutures for delicate tissue
- “Figure-of-eight” or mattress sutures for eyelid margin alignment
- Special attention to suture removal timing (usually within 5–7 days) to prevent suture tracks and minimize scarring
Wound Care After Surgery
- Keep the area clean and dry; gentle cleansing with saline as instructed.
- Apply prescribed antibiotic ointment.
- Use cold compresses to reduce swelling.
- Elevate head while sleeping.
- Avoid strenuous activities or rubbing the eyes.
Complication Management
- Early recognition of infection or wound dehiscence (separation)
- Scar massage and silicone gel for excessive scarring
- Revision surgery if cosmetic or functional results are unsatisfactory
Key Advice
- Always follow up with your surgeon as scheduled.
- Notify your doctor of pain, discharge, fever, or vision changes.
Cutting-Edge Technologies and Recent Advances
The field of eyelid trauma care has benefited from significant technological advances, making repairs safer and results more natural.
Innovations in Surgical Repair
- Microsurgical tools and techniques: Allow highly precise, minimally traumatic repairs—even in tiny children or complex injuries.
- Fibrin glue: Sometimes used alongside or instead of sutures for faster, sutureless wound closure in select cases.
- Absorbable stents and micro-implants: For canalicular repairs, reducing the need for additional procedures to remove them.
- 3D imaging and planning: Helps surgeons plan complex reconstructions, improving both appearance and eyelid function.
- Laser-assisted wound closure: Under investigation for select clean, linear wounds to minimize suture use and improve healing.
Regenerative and Adjunctive Therapies
- Bioengineered skin substitutes: Used for wounds with tissue loss or burns.
- Stem cell-enriched tissue grafts: In early clinical studies for improved healing and reduced scarring.
- Topical growth factors: Promote rapid, high-quality healing and reduce visible scarring.
- Advanced wound dressings: Moisture-retentive and antimicrobial dressings for better outcomes.
Telemedicine and Digital Monitoring
- Remote wound monitoring: Secure apps and platforms allow follow-up for healing progress and rapid identification of complications.
- AI image analysis: Experimental tools analyze healing and help predict risk of poor scarring or need for revision.
Practical Guidance for Patients
- Ask about all available wound closure options, especially for visible areas.
- If you’re a candidate for research or a new device, clarify risks, benefits, and evidence.
Ongoing Clinical Studies and Anticipated Trends
Innovation in eyelid trauma care is ongoing, aiming for better function, aesthetics, and patient satisfaction.
Current Areas of Research
- Next-generation biomaterials: Developing suture materials and adhesives that are strong, flexible, and nearly invisible.
- Growth factor therapies: Optimizing dosing and delivery to maximize wound healing and minimize scarring.
- Personalized surgery: Using genetics, imaging, and AI to tailor surgical approach and aftercare to individual healing profiles.
- Non-surgical closure devices: Studies on advanced glues and adhesive strips for minor wounds.
- Patient-centric outcome tracking: Digital apps capturing functional and cosmetic results for real-world effectiveness.
Recent and Upcoming Clinical Trials
- New sutureless eyelid closure devices in comparison with standard stitches
- Absorbable, anti-scarring stents for canalicular laceration repair
- Application of stem cell gels and growth factors for major eyelid injuries
- Trials tracking satisfaction and outcomes with digital monitoring tools
What’s on the Horizon?
- Scarless healing and invisible wound closure
- 3D printing of custom tissue scaffolds for reconstruction
- Full integration of telehealth in trauma aftercare
Tips for Staying Informed
- Ask your care team about participation in clinical studies.
- Follow major eye surgery and trauma organizations for updates.
Frequently Asked Questions
What should I do immediately after an eyelid laceration?
Gently stop any bleeding with a clean cloth, rinse with saline or water, and avoid touching or rubbing the area. Cover with sterile gauze and seek prompt medical attention—do not apply ointment unless advised.
When is surgery needed for an eyelid laceration?
Surgery is recommended for deep, gaping, or margin-involved wounds, tears with tissue loss, or injuries affecting the tear ducts or eye surface. Most significant eyelid lacerations benefit from surgical repair to optimize healing and appearance.
Can eyelid lacerations heal without stitches?
Minor, superficial cuts may heal with conservative care, but most eyelid lacerations—especially near the margin—need precise stitching for best results and to prevent deformity or scarring.
What are the risks of improper eyelid laceration management?
Improper care can lead to scarring, notching, eyelid deformity, incomplete closure, infection, or tear drainage problems. In severe cases, eye injury or vision loss may occur.
How do I care for my eyelid after surgical repair?
Keep the area clean and dry, apply prescribed ointments, avoid rubbing, follow activity restrictions, and attend all follow-up visits. Report any pain, discharge, fever, or vision changes to your doctor.
Are there new techniques to minimize eyelid scarring?
Yes, advances include micro-suturing, fibrin glue, growth factors, bioengineered dressings, and laser-assisted closures. Discuss all options with your surgeon based on your specific injury.
Disclaimer
This resource is for educational purposes only and is not a substitute for professional medical advice. If you experience an eyelid laceration or any eye injury, seek prompt evaluation by a qualified medical professional. Early intervention is essential to preserve vision and eyelid function.
If you found this article helpful, please consider sharing it on Facebook, X (formerly Twitter), or your preferred social platform. Help others access trustworthy eye health information and support our mission to provide expert, accessible medical content.