A hordeolum—commonly known as a stye—is a prevalent eyelid problem characterized by a painful, red bump near the edge of the eyelid, often resulting from a bacterial infection. While most styes resolve on their own, persistent or severe cases may require medical intervention, and rare instances might even need surgical treatment. Recent advancements have also introduced new therapies and smarter self-care techniques. In this comprehensive, SEO-optimized guide, we’ll explore what causes styes, how to treat them effectively, the latest innovations, and practical steps you can take to speed up recovery and minimize recurrence.
Table of Contents
- Understanding Hordeolum and Its Prevalence
- Proven Home Remedies and Standard Medical Treatments
- Procedures and Minimally Invasive Interventions
- Latest Technological and Pharmaceutical Advances
- Ongoing Research and Future Trends
- Frequently Asked Questions
- Disclaimer
Understanding Hordeolum and Its Prevalence
A hordeolum (stye) is an acute, localized infection or inflammation of the eyelid’s oil glands (most often the glands of Zeis or Meibomian glands), typically caused by Staphylococcus aureus bacteria. Styes can be external (affecting glands at the base of the eyelashes) or internal (involving deeper oil glands within the eyelid).
What Causes a Stye?
- Bacterial infection, usually from skin flora entering a blocked gland
- Poor eyelid hygiene or touching/rubbing the eyes with unwashed hands
- Use of old or contaminated eye makeup
- Blepharitis (chronic eyelid inflammation)
- Chronic skin conditions such as rosacea or seborrheic dermatitis
Common Signs and Symptoms
- Red, tender, swollen bump on the eyelid margin
- Pain, tearing, and mild crusting
- Sometimes a small, yellowish point indicating pus
How Common Are Styes?
Hordeola are one of the most frequent eyelid complaints, affecting all age groups and both sexes equally. Many people experience at least one stye in their lifetime. They tend to be more common in individuals with a history of eye rubbing, poor hygiene, or underlying skin conditions.
Risk Factors
- Touching eyes with dirty hands
- Wearing contact lenses or makeup overnight
- Chronic blepharitis or rosacea
- Diabetes (slightly increased risk)
Impact on Daily Life
While rarely serious, styes can be annoying, unsightly, and sometimes interfere with vision if they swell enough to press on the eye.
Practical Early Action Tips
- Don’t squeeze or pop a stye—this can spread infection
- Wash hands frequently, especially before touching the face or eyes
- Remove makeup every night and avoid sharing cosmetics
Understanding these basics sets the foundation for recognizing styes early and managing them safely at home or with medical help when needed.
Proven Home Remedies and Standard Medical Treatments
Most hordeola resolve on their own within a week, but the right self-care can accelerate healing and reduce discomfort. Let’s review the most trusted therapies and when to seek medical help.
Effective Home Care Strategies
- Warm Compresses:
Apply a clean, warm (not hot) washcloth to the closed eyelid for 10–15 minutes, 3–4 times a day. This encourages drainage, relieves pain, and can speed up resolution. - Gentle Eyelid Cleansing:
Use diluted baby shampoo or a commercial eyelid cleanser with a cotton swab to gently clean the lid margins and lashes. - Discontinue Eye Makeup/Contact Lenses:
Pause use until the stye is fully resolved to prevent irritation or re-infection. - Pain Relief:
Over-the-counter pain relievers like acetaminophen or ibuprofen can help with discomfort.
Over-the-Counter Options
- Lubricating Eye Drops:
Artificial tears may help with irritation. - Antibiotic Ointments:
Available in some regions without prescription—apply only if recommended by a pharmacist or healthcare provider.
Medical Treatments When Needed
- Prescription Antibiotics:
Topical antibiotics (e.g., erythromycin or bacitracin ointments) may be prescribed for persistent or severe cases, especially if signs of secondary infection are present. - Oral Antibiotics:
Rarely required, but may be used for very large styes, recurrent cases, or in those with complicating risk factors (such as diabetes or immune suppression).
Practical Prevention Tips
- Replace old cosmetics regularly and never share them
- Keep eyelids clean, especially for those with chronic blepharitis
- Address underlying skin or lid inflammation with ongoing care
Home remedies and standard therapies are highly effective, but always monitor for worsening symptoms, spreading redness, or fever—signs that you need medical evaluation.
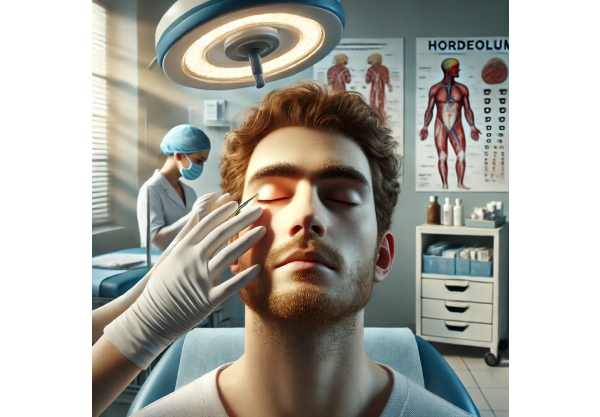
Procedures and Minimally Invasive Interventions
While most styes clear up with conservative care, a small percentage require procedural or surgical management, especially if the bump persists, grows, or becomes particularly painful.
When Is Intervention Needed?
- No improvement after 1–2 weeks of home care and antibiotics
- Increasing pain, swelling, or signs of spreading infection
- Visual disturbance from significant swelling
- Large internal styes or those developing into a chalazion (a chronic, non-infectious lump)
Key Office Procedures
- Incision and Drainage (I\&D):
A brief, in-office procedure where the doctor numbs the eyelid and makes a tiny incision to release the trapped pus. Rapid relief and healing typically follow. - Steroid Injection:
For persistent lumps (chalazia), a small steroid injection may reduce inflammation and speed resolution, especially when surgery isn’t ideal.
Minimally Invasive Technologies
- Thermal Pulsation Devices:
Tools such as LipiFlow are being investigated for their ability to unclog glands and support lid hygiene, especially in chronic or recurrent cases. - Laser Therapy:
Some eye specialists use laser to target and open blocked glands, though this remains relatively uncommon and experimental.
Care After Procedures
- Apply warm compresses as instructed
- Use prescribed antibiotic ointment
- Avoid touching, rubbing, or exposing the area to irritants
Potential Complications to Watch For
- Excessive bleeding, persistent pain, or swelling
- Signs of orbital cellulitis (painful swelling extending beyond the lid)
- Recurrent styes—may warrant evaluation for underlying causes like blepharitis
For most, these interventions are simple, safe, and effective—offering fast recovery when conservative methods aren’t enough.
Latest Technological and Pharmaceutical Advances
Recent years have seen exciting developments in the treatment and prevention of hordeola, especially for those with recurrent or complicated cases.
Next-Generation Therapies
- Antibiotic-Coated Eyelid Wipes:
Newer over-the-counter products combine gentle cleansing with targeted antibacterial action, promoting lid hygiene and reducing infection risk. - Probiotic-Based Cleansers:
Early studies suggest that restoring a healthy balance of bacteria on the skin and eyelids may prevent styes in those prone to chronic recurrence. - Advanced Topical Antibiotics:
New formulations offer better penetration and longer-lasting effects for stubborn or deep-seated infections.
Technology for Diagnosis and Home Monitoring
- Smartphone Imaging:
AI-powered apps now assist in documenting and tracking eyelid lesions, supporting remote diagnosis and follow-up. - Teleophthalmology:
Virtual consultations have become increasingly common, offering rapid specialist input for persistent or unclear cases.
Regenerative and Alternative Strategies
- Lid Margin Gland Regeneration:
Research into regenerating meibomian gland function (for chronic stye sufferers) is showing early promise. - AI-Driven Predictive Models:
Artificial intelligence is being harnessed to predict who is at highest risk of stye recurrence, allowing for earlier intervention.
Real-World Advice for Patients
- Ask your eye care provider about the latest lid hygiene technologies
- Consider participating in research studies if you experience frequent or hard-to-treat styes
Innovation is expanding treatment options—making life more comfortable and styes less disruptive.
Ongoing Research and Future Trends
The field of eyelid disease management is advancing rapidly, with a strong focus on preventing recurrent hordeola and enhancing treatment for stubborn or complicated cases.
Key Areas of Research
- Long-Term Prevention:
Studies are exploring daily lid hygiene regimens, probiotic supplementation, and new topical therapies for those with chronic eyelid inflammation. - Rapid Point-of-Care Diagnostics:
New tools aim to help doctors and patients differentiate between styes, chalazia, and more serious conditions instantly. - Gene-Based Risk Assessment:
Investigations into genetic factors could help identify individuals at higher risk of recurrent styes or related conditions. - Laser and Light-Based Therapies:
Ongoing clinical trials are testing devices that use targeted light or laser to clear blocked glands and promote healing. - Telemedicine Expansion:
With more care moving online, remote monitoring and management protocols are becoming standard for eyelid disorders.
What’s Ahead for Patients?
- More personalized treatment plans based on risk factors and microbiome profiles
- At-home devices for maintaining eyelid health and preventing recurrence
- Expanded use of digital health platforms for rapid diagnosis and care coordination
How You Can Stay Informed
- Subscribe to reputable eye health websites or patient organizations
- Participate in clinical research if you have a history of chronic or complicated styes
As research continues, patients can look forward to safer, more convenient, and more effective options for preventing and treating hordeola.
Frequently Asked Questions
What is the fastest way to get rid of a stye?
Applying warm compresses several times daily is the quickest home remedy. For stubborn cases, your doctor may prescribe antibiotic ointment or perform a minor procedure to drain the stye.
Are styes contagious?
A stye itself isn’t directly contagious, but the bacteria causing it can be spread through sharing towels or makeup. Good hygiene prevents transmission.
When should I see a doctor for a stye?
Seek medical help if the stye lasts longer than 7–10 days, becomes very painful, swells rapidly, affects vision, or if you develop fever or spreading redness.
Can I pop a stye at home?
No—never try to pop or squeeze a stye, as this can worsen infection or cause complications. Let it drain naturally or seek professional care.
Why do I keep getting styes?
Recurring styes are often linked to chronic blepharitis, poor eyelid hygiene, or underlying skin conditions. Keeping lids clean and addressing these issues reduces recurrence risk.
What is the difference between a stye and a chalazion?
A stye is an acute, painful infection of an eyelid gland. A chalazion is a chronic, usually painless lump that forms when a gland remains blocked after inflammation.
Are there new treatments for styes?
Emerging therapies include antibiotic-coated lid wipes, probiotic cleansers, and advanced home devices. Ask your eye doctor about the latest options for persistent or recurrent styes.
Disclaimer
The information provided in this article is for educational purposes only and does not substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with any questions regarding a medical condition.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or any platform you prefer. Your support allows us to keep producing quality, accessible health content. Don’t forget to follow us for updates—thank you for helping others learn more about eye health and self-care!






