Juvenile open-angle glaucoma (JOAG) is a rare but sight-threatening form of glaucoma that appears in children, adolescents, and young adults—often between ages 3 and 40. Unlike adult-onset glaucoma, JOAG is characterized by earlier onset, more aggressive progression, and a stronger genetic influence. Timely diagnosis and a tailored, multi-faceted management plan are essential to preserve vision and quality of life. This comprehensive guide will help patients, families, and providers understand JOAG’s complexities, exploring established therapies, innovative surgical options, and breakthroughs shaping the future of care for young people with glaucoma.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
Condition Overview and Epidemiology
Juvenile open-angle glaucoma (JOAG) is a form of primary open-angle glaucoma that presents in individuals between childhood and early adulthood, typically ages 3–40. Unlike congenital glaucoma, which manifests at birth or within the first years of life, JOAG is often diagnosed in late childhood or adolescence.
Defining Features and Pathophysiology
- Characterized by increased intraocular pressure (IOP) due to resistance at the trabecular meshwork—the eye’s drainage system.
- The angle of the anterior chamber remains open, as in adult open-angle glaucoma.
- Progressive optic nerve damage and visual field loss can occur if untreated.
Epidemiology
- JOAG is rare: estimates suggest it represents about 0.2% to 1% of all glaucoma cases in Western countries.
- Both sexes can be affected, with some studies showing a slight male predominance.
- Family history and certain genetic mutations (e.g., MYOC gene) play a strong role.
Risk Factors
- Family history of juvenile or adult open-angle glaucoma
- Mutations in genes such as MYOC, CYP1B1, and others
- High myopia (nearsightedness)
- African, Hispanic, or Asian ancestry (increased risk in some populations)
- Thin corneas (lower corneal thickness is associated with greater risk)
Symptoms and Clinical Presentation
- Most children and teens are asymptomatic until significant vision is lost.
- Some may experience blurred vision, headaches, eye pain, or halos around lights.
- Routine eye exams often reveal elevated IOP, optic nerve cupping, or visual field defects.
Potential Complications
- Irreversible vision loss if not detected and treated early
- Emotional, educational, and social challenges due to visual impairment
Diagnosis
- Comprehensive eye exam: includes IOP measurement, gonioscopy, optic nerve imaging (OCT), and visual field testing.
- Genetic counseling and testing may be offered for families with a strong history.
Practical Advice
- Encourage regular pediatric eye exams, especially if there’s a family history.
- Discuss genetic testing and counseling with your ophthalmologist for at-risk families.
- Monitor for subtle signs—vision changes, eye discomfort, or frequent blinking—in children and teens.
Conventional and Pharmacological Therapies
The initial management of juvenile open-angle glaucoma centers on lowering intraocular pressure (IOP) to preserve optic nerve function and prevent further vision loss. Medical therapy is often the first line, particularly in early or mild cases.
First-Line Pharmacological Approaches
- Prostaglandin analogs (latanoprost, bimatoprost, travoprost):
- Once-daily drops that increase outflow of aqueous humor, often highly effective in JOAG.
- Beta-blockers (timolol, betaxolol):
- Decrease aqueous humor production; can be used in combination therapy.
- Alpha agonists (brimonidine):
- Both reduce aqueous production and increase outflow.
- Carbonic anhydrase inhibitors (dorzolamide, brinzolamide):
- Available as topical drops or, less commonly, oral agents.
- Rho kinase inhibitors (netarsudil):
- A newer class that lowers IOP via multiple mechanisms.
Therapy Principles and Dosage
- Start with the fewest number of medications necessary to reach the target IOP.
- Adherence is crucial, so once-daily regimens are preferred when possible.
- Side effects should be carefully monitored, especially in children.
When Medical Management Isn’t Enough
- JOAG often progresses despite optimal medical therapy, requiring surgical intervention.
- Medication burden, intolerance, and suboptimal response are common reasons to escalate treatment.
Supportive Measures and Practical Advice
- Teach and supervise children and teens in proper drop instillation techniques.
- Encourage family involvement to ensure adherence and follow-up.
- Maintain a medication diary or use reminder apps to track dosing schedules.
Potential Medication Side Effects
- Local: Eye redness, stinging, changes in iris or eyelash appearance
- Systemic: Fatigue, asthma exacerbation (with beta-blockers), dry mouth, headache
- Report any concerning reactions to the prescribing ophthalmologist promptly.
Monitoring
- Regular follow-up every 3–6 months for IOP checks, optic nerve imaging, and visual fields.
- Adjust treatment plan based on disease progression and tolerability.
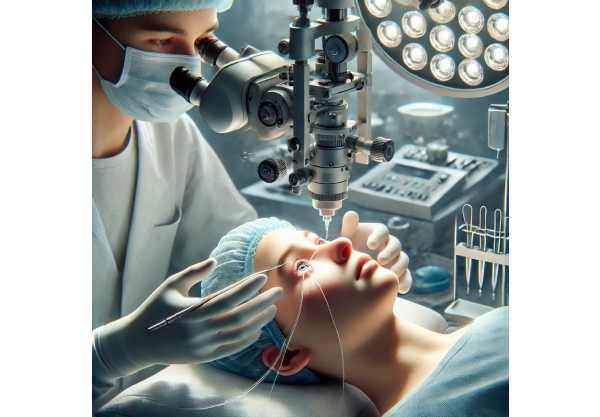
Surgical and Interventional Procedures
Many children and teens with JOAG require surgical intervention to achieve adequate pressure control, especially as the disease progresses or in cases of medication intolerance.
Indications for Surgery
- Inadequate IOP control with medications
- Progressive optic nerve damage despite treatment
- Medication side effects or poor adherence
Key Surgical Options
- Trabeculectomy:
- Creates a new drainage pathway for fluid; the gold standard for many years.
- Antimetabolites (mitomycin C) are often used to reduce scarring and increase success rates.
- Glaucoma Drainage Devices (GDD):
- Valved (Ahmed) or non-valved (Baerveldt) shunt devices are implanted to divert aqueous humor.
- Especially useful in eyes with previous failed surgeries or high risk of scarring.
- Minimally Invasive Glaucoma Surgery (MIGS):
- Devices like iStent, Hydrus, or Trabectome have shown promise in young patients.
- Less invasive, with faster recovery but may not be as effective in advanced cases.
- Goniotomy and Trabeculotomy:
- Incision or removal of trabecular meshwork to enhance drainage, especially in younger children.
- Can be done with traditional or ab-interno (microincisional) techniques.
- Cyclodestructive Procedures:
- For refractory cases, procedures like transscleral cyclophotocoagulation lower IOP by reducing fluid production.
Pre- and Postoperative Considerations
- Preoperative assessment includes thorough imaging, risk stratification, and counseling.
- Postoperative care involves close monitoring for infection, inflammation, and pressure spikes.
- Lifelong follow-up is essential as failure rates increase over time in younger patients.
Practical Tips for Families
- Involve children in age-appropriate discussions about their surgery and recovery.
- Prepare for time off school and support with homework or activities.
- Recognize the emotional impact of surgery and offer reassurance.
Emerging Innovations and Advanced Technologies
Glaucoma research is advancing rapidly, bringing hope for safer, more effective treatments tailored to the unique needs of young patients with JOAG.
Recent Breakthroughs and Technologies
- Gene Therapy and Molecular Medicine:
- Investigational therapies target known genetic mutations (MYOC, CYP1B1) to slow or halt disease progression.
- Cell-Based Regeneration:
- Studies are exploring stem cell–derived trabecular meshwork repair or replacement.
- AI and Precision Diagnostics:
- Artificial intelligence in OCT and visual field analysis can detect early changes and predict progression.
- Telemedicine and Digital Monitoring:
- Remote IOP monitoring, smartphone apps, and virtual visits make lifelong care more accessible and consistent.
- Drug-Delivery Implants:
- Biodegradable devices (e.g., bimatoprost ring, punctal plugs) release medication over months, improving adherence.
- Next-Generation MIGS Devices:
- Customizable implants and ab-interno approaches are designed for pediatric anatomy.
Personalized Medicine
- Integration of genetic, imaging, and clinical data allows tailored risk assessment and therapy for each patient.
- Pharmacogenomics may soon enable personalized medication selection to minimize side effects and maximize benefit.
Lifestyle and Support Innovations
- Adaptive devices and e-learning platforms help students with vision loss excel in school.
- Virtual reality and gamified rehab tools can make eye exercises and follow-up more engaging for children.
Practical Advice
- Ask your care team about clinical trial opportunities and emerging therapies.
- Consider telehealth for routine follow-ups, especially if travel is a barrier.
- Stay informed about new devices or monitoring tools designed for pediatric glaucoma.
Clinical Trials and Future Directions
Ongoing research continues to expand the therapeutic landscape for JOAG, offering hope for even better outcomes in the years ahead.
Current and Upcoming Clinical Trials
- Gene and Molecular Therapy Studies:
- Targeting MYOC and other mutations to correct underlying defects.
- Long-Acting Drug Delivery:
- Implants that deliver prostaglandins or novel drugs over months or years.
- Advanced Imaging Biomarkers:
- Studies validating new OCT and AI-powered techniques for earlier diagnosis and better monitoring.
- Minimally Invasive and Customizable Surgeries:
- Evaluation of new MIGS, stents, and surgical approaches adapted for children and teens.
- Patient-Reported Outcomes and Quality of Life:
- Research focusing on educational, social, and psychological impacts of JOAG.
How to Find and Join Clinical Trials
- Search clinicaltrials.gov and major eye institute websites.
- Ask your ophthalmologist about eligibility and trial locations.
- Consider joining patient advocacy organizations for updates and support.
The Future of JOAG Management
- Greater use of genetic data and AI will personalize care and potentially prevent progression before vision is lost.
- Advances in remote monitoring and drug delivery will ease lifelong disease management.
- Ongoing innovations in pediatric ophthalmology will further improve quality of life and vision outcomes.
Patient Empowerment and Community
- Participate in research when possible—patient input shapes future care.
- Seek support from peer and family networks to navigate emotional, academic, and daily life challenges.
Frequently Asked Questions
What causes juvenile open-angle glaucoma?
JOAG is often caused by genetic mutations affecting the eye’s drainage system, but can also result from abnormal development or secondary to other eye conditions. Family history increases risk, and routine screening is important for at-risk children.
What are the symptoms of juvenile open-angle glaucoma?
Most children and young adults have no symptoms until significant vision loss occurs. Warning signs may include blurry vision, headaches, eye pain, or increased blinking. Regular eye exams are crucial for early detection.
What is the best treatment for juvenile open-angle glaucoma?
Initial treatment involves medicated eye drops to lower intraocular pressure. Many patients require surgery, such as trabeculectomy, MIGS, or glaucoma drainage implants, especially when medication isn’t enough.
Can juvenile open-angle glaucoma be cured?
There is no cure, but with early detection and effective management, most children can preserve useful vision for life. Ongoing advances in genetics and surgery offer hope for improved outcomes.
Are there new therapies for juvenile open-angle glaucoma?
Yes. Innovations include gene therapy, sustained-release implants, and AI-powered diagnostics. Clinical trials are testing new drug delivery systems and minimally invasive surgeries specifically designed for young patients.
Is juvenile open-angle glaucoma inherited?
Yes, in many cases JOAG is linked to inherited genetic mutations. Genetic counseling and testing can help families assess risk and plan early screening for children and relatives.
How can families help manage juvenile open-angle glaucoma?
Ensure children follow their treatment plan, attend regular eye exams, and learn proper drop techniques. Emotional and educational support is important; resources from patient organizations can help.
Disclaimer:
This article is for informational purposes only and does not replace advice from your medical provider. For any concerns or symptoms related to juvenile open-angle glaucoma, always consult your eye care professional. Early diagnosis and adherence to treatment are essential for preserving vision.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your favorite social media network. Your support helps us continue providing trusted eye health information—thank you for spreading awareness!










