Lacrimal duct obstruction is a condition that disrupts the normal flow of tears from the eye to the nose, resulting in symptoms such as excessive tearing, recurrent eye infections, and sometimes discomfort or blurred vision. This comprehensive guide provides an in-depth look at how lacrimal duct obstruction develops, who is at risk, and what modern treatments and innovations are available. Whether you are a patient, caregiver, or medical professional, this resource will help you understand standard therapies, surgical techniques, and cutting-edge advancements in managing this common yet impactful eye problem.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
Condition Overview and Epidemiology
Lacrimal duct obstruction occurs when the drainage system for tears—comprising the puncta, canaliculi, lacrimal sac, and nasolacrimal duct—becomes blocked or narrowed. Tears cannot drain properly, leading to excessive tearing (epiphora), recurrent conjunctivitis, and possible infections such as dacryocystitis.
Pathophysiology
- Blockages can occur at any point along the drainage pathway, most often in the nasolacrimal duct.
- Causes include congenital malformations, inflammation, trauma, infections, or age-related narrowing.
- Chronic obstruction leads to stagnant tears, bacterial overgrowth, and, in some cases, abscess formation.
Epidemiology
- Congenital nasolacrimal duct obstruction affects up to 20% of newborns but resolves spontaneously in most cases by age one.
- Acquired forms are more common in adults, especially those over 50.
- Females have a higher incidence than males, likely due to narrower bony nasolacrimal canals.
Risk Factors
- Age (older adults and infants are most affected)
- Chronic sinus disease or allergies
- Previous nasal or facial trauma
- Autoimmune diseases (e.g., sarcoidosis, Wegener’s granulomatosis)
- Prolonged use of topical eye medications
Clinical Presentation
- Persistent tearing and overflow of tears (epiphora)
- Chronic conjunctivitis or blepharitis
- Mucous discharge or pus from the puncta
- Redness and swelling near the inner corner of the eye (especially in dacryocystitis)
- Blurred vision if tear film is disturbed
Diagnosis
- Thorough history and eye exam
- Fluorescein dye disappearance test
- Irrigation/probing of the lacrimal system
- Dacryocystography or imaging for complex/refractory cases
Practical Advice
- If you or your child has constant tearing or recurrent eye infections, ask your eye doctor about possible lacrimal duct problems.
- Avoid rubbing the eyes, as this can worsen inflammation or introduce bacteria.
Conventional and Pharmacological Therapies
In many cases, especially in infants, non-surgical methods are the first line of treatment for lacrimal duct obstruction. Timely intervention can help resolve symptoms and prevent complications.
Conservative Management in Infants
- Massage (Crigler massage): Gentle downward pressure over the lacrimal sac several times a day to encourage duct opening.
- Warm compresses: Applied to the inner corner of the eye to reduce discomfort and encourage drainage.
- Observation: Up to 90% of congenital blockages resolve spontaneously by 12 months.
Pharmacological Approaches
- Topical antibiotics: Used if infection or mucopurulent discharge is present. Drops or ointment may be prescribed for short-term use.
- Anti-inflammatory drops: Sometimes prescribed to reduce swelling in the duct or surrounding tissues.
Supportive Care
- Careful lid hygiene to reduce infection risk.
- Avoiding irritants and allergens that can exacerbate symptoms.
- For adults, treating underlying sinus or nasal problems can sometimes improve drainage.
Monitoring and Follow-Up
- Infants not resolved by 12 months or with repeated infections need evaluation for procedural intervention.
- Adults with new-onset or persistent symptoms should seek evaluation for underlying causes, such as tumors or chronic sinus disease.
Practical Tips
- Consistency is key with massage; learn proper technique from your healthcare provider.
- Use antibiotics only as directed to avoid resistance or side effects.
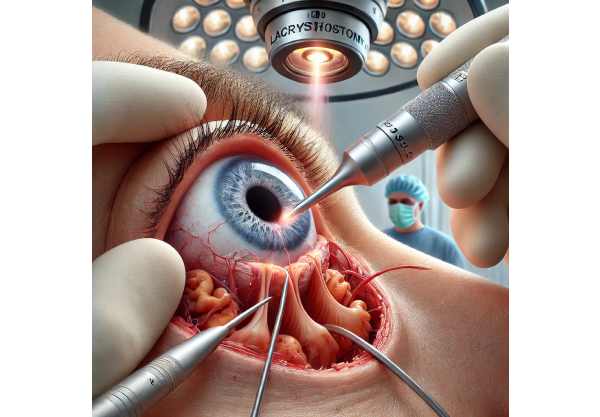
Surgical and Interventional Procedures
When non-surgical therapies are insufficient, various minimally invasive and surgical options are available for both children and adults.
Probing and Irrigation
- Most common initial procedure for infants and toddlers who fail conservative management.
- A thin probe is gently inserted into the duct to clear the blockage, sometimes combined with saline irrigation.
- High success rate in young children, often performed under light anesthesia.
Balloon Dacryoplasty
- Used for recurrent or complex blockages in children and adults.
- A small balloon catheter is threaded through the duct and inflated to open the passage.
- Can be combined with stenting for improved results.
Intubation with Silicone Tubes
- Thin, flexible tubes are placed within the duct to keep it open during healing.
- Left in place for several weeks to months and then removed in the clinic.
Dacryocystorhinostomy (DCR)
- Gold standard surgical treatment for adult nasolacrimal duct obstruction.
- Creates a new drainage channel between the lacrimal sac and nasal cavity.
- Can be performed externally (through a small skin incision) or endoscopically (through the nose).
- Endoscopic DCR offers faster recovery and no external scar.
Conjunctivodacryocystorhinostomy (CDCR)
- For patients with canalicular blockages (blockages closer to the eyelid), a glass or synthetic tube (Jones tube) bypasses the entire drainage system.
- Reserved for severe, refractory cases.
Adjunct and Revision Procedures
- Laser-assisted DCR for select patients.
- Revision DCR or stent replacement for failed prior surgeries.
- Abscess drainage if dacryocystitis is present.
Postoperative Care
- Nasal decongestants and antibiotic drops may be prescribed.
- Avoid blowing the nose forcefully after surgery.
- Follow all post-op instructions closely for best outcomes.
Practical Advice for Patients
- Discuss anesthesia options and expected recovery times with your surgeon.
- Notify your doctor immediately if you experience fever, severe pain, or vision changes after a procedure.
Emerging Innovations and Advanced Technologies
The field of lacrimal duct obstruction management continues to evolve, with a focus on minimizing invasiveness and enhancing long-term outcomes.
Minimally Invasive Endoscopic Techniques
- Advanced endoscopes allow direct visualization and precise repair of obstructions.
- Microdebriders and radiofrequency ablation devices are used for tissue removal with minimal trauma.
Biodegradable and Drug-Eluting Stents
- New stents dissolve over time, eliminating the need for removal.
- Drug-eluting versions release anti-inflammatory or antibiotic agents to reduce scarring and infection.
Laser and Image-Guided Surgery
- Lasers (diode, KTP, or Holmium\:YAG) provide precise, bloodless incisions and can be used in conjunction with endoscopic DCR.
- Intraoperative imaging helps surgeons avoid complications and improve success rates.
Artificial Intelligence and Teleophthalmology
- AI-assisted diagnosis and tear flow assessment can help select optimal candidates for various treatments.
- Telemedicine allows remote follow-up for post-op care and monitoring.
Biological and Regenerative Advances
- Research into tissue engineering aims to regenerate damaged duct tissue using stem cells or growth factors.
- Early clinical trials of bioengineered ducts are underway.
Patient-Focused Technology
- Smartphone-based tear flow measurement devices help patients and doctors track recovery and identify recurrence early.
- Digital platforms enable video-based coaching for parents learning infant lacrimal massage.
Practical Tips for Patients
- Ask your provider about new stent options and minimally invasive surgery.
- Consider telehealth for routine follow-ups, especially after simple procedures.
Clinical Trials and Future Directions
A robust pipeline of research is driving continual improvement in lacrimal duct obstruction care, focusing on less invasive treatments, greater comfort, and enhanced success.
Key Areas of Current Research
- Improved Drug Delivery: Topical agents and drug-eluting stents to reduce the need for surgery.
- Gene Therapy: Early work exploring whether genetic modification can restore duct patency in certain congenital cases.
- Biodegradable Materials: Safer, more comfortable alternatives for stents and tubes.
- Personalized Surgical Planning: AI-driven simulations to customize DCR approaches based on each patient’s anatomy.
Active and Upcoming Clinical Trials
- Novel endoscopic and laser-based techniques compared to traditional DCR.
- Efficacy of biodegradable and drug-eluting stents.
- Patient-reported outcomes in children and elderly patients following various procedures.
Getting Involved
- Check hospital research centers, academic medical centers, and clinicaltrials.gov for ongoing studies.
- Participation in clinical trials can provide early access to emerging treatments.
Trends on the Horizon
- Widespread adoption of office-based, sutureless procedures.
- Development of regenerative solutions for severe or recurrent cases.
- Use of real-time imaging and AI in both diagnosis and postoperative assessment.
Empowering Patients
- Stay informed through patient support groups and advocacy networks.
- Ask about the latest clinical trials if you’re facing recurrent or complex obstruction.
Frequently Asked Questions
What is lacrimal duct obstruction and what are its symptoms?
Lacrimal duct obstruction is a blockage in the tear drainage system, causing watery eyes, recurrent eye infections, and sometimes discharge. Symptoms include constant tearing and swelling near the inner corner of the eye.
How is lacrimal duct obstruction diagnosed?
Doctors diagnose it with a detailed eye exam, tear drainage tests, and sometimes imaging or probing of the tear duct system to locate the blockage.
Can lacrimal duct obstruction resolve on its own?
In infants, many cases resolve without intervention by age one. Persistent cases or adult-onset obstructions usually require treatment.
What are the best treatments for lacrimal duct obstruction?
Options include massage, antibiotics for infection, minimally invasive procedures (probing, balloon dilation), and surgery such as dacryocystorhinostomy (DCR) for adults.
Is surgery for lacrimal duct obstruction safe?
Yes—procedures like DCR are generally safe and effective. Minimally invasive techniques further reduce risks and speed recovery.
Are there new innovations in treating tear duct obstruction?
Emerging advances include laser surgery, biodegradable stents, drug-eluting devices, and image-guided endoscopic techniques.
When should I see a specialist for lacrimal duct problems?
If you or your child has constant tearing, recurrent eye infections, or swelling, see an ophthalmologist or oculoplastic surgeon for assessment.
Disclaimer:
This article is for educational purposes only and should not be used as a substitute for professional medical advice. If you or a loved one experiences persistent tearing, swelling, or infection, consult an eye care specialist promptly.
If you found this resource valuable, please share it on Facebook, X (formerly Twitter), or your preferred social channel. Your support helps us create and share trusted, up-to-date eye health guides for everyone. Thank you!






