Neovascular Glaucoma (NVG) is a severe type of secondary glaucoma characterized by the formation of new, abnormal blood vessels on the iris and drainage angle of the eyeball. These new blood vessels may obstruct the eye’s drainage system, resulting in elevated intraocular pressure (IOP). This increase in IOP can damage the optic nerve, leading to vision loss. NVG is frequently associated with ischemic retinal diseases, such as diabetic retinopathy and central retinal vein occlusion, which cause the release of vascular endothelial growth factor. VEGF promotes the formation of new blood vessels in response to retinal hypoxia.
Patients with NVG may experience symptoms such as redness, pain, blurred vision, and visible new blood vessels on the iris. The condition can progress quickly, making timely diagnosis and intervention critical to preserving vision and avoiding further ocular complications. A comprehensive eye examination is usually required to make a diagnosis, which includes gonioscopy to evaluate the angle of the anterior chamber, tonometry to measure IOP, and imaging studies such as optical coherence tomography (OCT) to assess retinal health. Understanding the underlying causes and mechanisms of NVG is critical for creating effective treatment plans and improving patient outcomes.
Standard Neovascular Glaucoma Treatments
Managing and treating Neovascular Glaucoma necessitates a multifaceted approach that addresses both the underlying cause of neovascularization and the high intraocular pressure. Standard treatment methods include medical, laser, and surgical interventions.
Medical Management
Medical management aims to control intraocular pressure and inflammation. This frequently requires the use of:
- Topical Medications: These include beta-blockers, alpha agonists, carbonic anhydrase inhibitors, and prostaglandin analogs, which all help to lower IOP. Combination eye drops can also help with pressure control.
- Systemic Medication: Acetazolamide, for example, is an oral carbonic anhydrase inhibitor that can lower IOP by reducing aqueous humor production. In acute cases, intravenous mannitol can be used to rapidly reduce IOP.
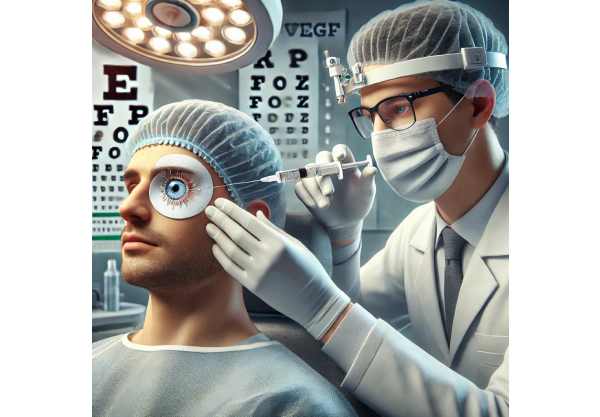
- Anti-VEGF injections: Intravitreal injections of anti-VEGF agents such as bevacizumab, ranibizumab, or aflibercept are used to reduce neovascularization by inhibiting VEGF activity. These injections help to regress new blood vessels and can lower inflammation and IOP.
Laser Treatments
Laser treatments help manage NVG by focusing on abnormal blood vessels and improving aqueous outflow:
- Panretinal Photocoagulation (PRP): This laser treatment is intended to treat the underlying ischemic retinal disease. By inducing burns in the peripheral retina, PRP reduces the stimulus for VEGF production and subsequent neovascularization.
- Cyclophotocoagulation: This procedure uses a laser to target and reduce the ciliary body’s production of aqueous humor, lowering IOP.
Surgical Interventions
When medical and laser treatments fail to control IOP, surgical interventions are considered.
- Trabeculectomy: This surgical procedure opens a new drainage pathway for aqueous humor to leave the eye, lowering IOP. Trabeculectomy is frequently used in conjunction with anti-VEGF injections to improve results.
- Glaucoma Drainage Devices (GDD): These devices, such as the Ahmed or Baerveldt implants, are intended to improve aqueous humor drainage and lower IOP. GDDs are especially useful in situations where traditional surgeries have failed.
- Cyclodestructive Procedures: Cyclocryotherapy and cyclophotocoagulation are two techniques for reducing aqueous humor production by targeting and destroying parts of the ciliary body.
Innovative Neovascular Glaucoma Treatments
Recent advances in the treatment of Neovascular Glaucoma have greatly improved the prognosis for patients suffering from this difficult condition. These innovations include novel pharmacological therapies, advanced surgical techniques, and cutting-edge technologies that aim to improve the efficacy and safety of NVG management.
Extended-Release Drug Delivery System
One of the most promising developments in NVG treatment is the creation of extended-release drug delivery systems. These systems are designed to provide sustained release of medications, which improve treatment adherence and efficacy.
- Anti-VEGF Implants with Sustained Release Implants containing ranibizumab, such as the Port Delivery System (PDS), deliver anti-VEGF medication continuously over several months. This reduces the need for frequent intravitreal injections while also ensuring consistent drug levels, thereby improving neovascularization control.
- Biodegradable implants: These implants slowly release medications as they dissolve over time. For example, Dexamethasone intravitreal implants (Ozurdex) have long-term anti-inflammatory effects, which aid in the management of ocular inflammation and neovascularization.
Genetic Therapy
Gene therapy is a developing field that has the potential to transform NVG treatment. By introducing or modifying genes within the eye, gene therapy can target the underlying causes of neovascularization and IOP elevation.
- VEGF Inhibition: Researchers are looking into gene therapies that deliver anti-VEGF genes to the eye, resulting in long-term suppression of VEGF activity. This approach could provide a more long-term solution than repeated anti-VEGF injections.
- Neuroprotection: Gene therapies that promote the survival and function of retinal ganglion cells are being studied in order to prevent optic nerve damage and preserve vision in NVG patients.
Advances in Glaucoma Drainage Devices
Recent developments in glaucoma drainage devices have improved their efficacy and safety, resulting in better outcomes for NVG patients:
- Microstents: Devices such as the iStent and Hydrus Microstent are small implants that improve aqueous outflow via the eye’s natural drainage channels. These microstents are less invasive than traditional glaucoma surgeries and can be implanted alongside cataract surgery, lowering the overall surgical burden.
- Next-Generation Implants: Newer implants, such as the Xen Gel Stent, are intended to produce a controlled outflow of aqueous humor while reducing the complications associated with traditional drainage devices. These implants have a safer profile, with less risk of hypotony and implant migration.
Minimal Invasive Glaucoma Surgery (MIGS)
MIGS has changed the face of glaucoma surgery by providing less invasive options with shorter recovery times and fewer complications:
- Trabecular Meshwork Surgery: Procedures such as trabeculotomy and goniotomy focus on the trabecular meshwork to improve aqueous outflow. These techniques cause minimal eye trauma, making them appropriate for NVG patients with mild to moderate disease.
- Superchoroidal Devices: Devices like the CyPass Micro-Stent provide an alternate route for aqueous humor to drain into the suprachoroidal space, effectively lowering IOP with minimal invasiveness.
Advanced Imaging and Diagnostic Tools
Improved imaging techniques have improved the diagnosis and management of NVG, allowing for more precise treatment planning.
- Optical Coherence Tomography Angiography (OCTA): OCTA produces detailed images of retinal and choroidal blood vessels without the use of dye injections. This technology enables the early detection of neovascularization and helps to monitor the efficacy of anti-VEGF therapies.
- Ultrasound Biomicroscopy (UBM): UBM provides high-resolution imaging of the anterior segment, allowing for accurate evaluation of the drainage angle and ciliary body. This is especially useful for planning surgical procedures and determining the efficacy of glaucoma drainage devices.
Personalized Medical Approaches
Personalized medicine is becoming increasingly important in the treatment of NVG, with tailored therapies based on individual patient characteristics.
- Pharmacogenomics: Genetic testing can identify patients who are more likely to respond to certain medications, allowing for more individualized treatment plans. This approach maximizes therapeutic efficacy while minimizing side effects.
- Biomarker identification: The search for biomarkers that predict disease progression and treatment response in NVG patients is ongoing. These biomarkers can help guide treatment decisions and provide more accurate disease monitoring data.
Telemedicine & Remote Monitoring
The combination of telemedicine and remote monitoring technologies has improved access to care and disease management for NVG patients:
- Remote IOP Monitoring: Devices such as the Triggerfish contact lens sensor track IOP fluctuations throughout the day. This real-time data enables healthcare providers to make informed treatment adjustments.
- Teleophthalmology: Virtual consultations and remote imaging enable routine monitoring of NVG patients, reducing the need for frequent in-person visits. This is especially beneficial for patients with mobility issues or who live in remote areas.
Future Directions for NVG Research
Ongoing research is exploring new avenues for treating NVG, with a few promising directions:
- Nanoparticle-Based Therapies: Nanoparticles can deliver medications directly to specific tissues, increasing drug delivery efficiency and lowering systemic side effects. This technology has the potential to transform the treatment of ocular diseases, including NVGs.
- Stem Cell Therapy: Stem cell-based treatments seek to regenerate damaged retinal and optic nerve tissues, with the goal of restoring vision in NVG patients. While still in the experimental stage, this approach shows great promise for the future.
- Combination Therapies: Combining multiple treatment modalities, such as anti-VEGF injections, laser therapy, and minimally invasive surgery, can provide synergistic benefits and improve overall treatment outcomes for NVG patients.






