What is neurofibroma of the orbit?
Neurofibroma of the orbit is a benign tumor that develops from nerve sheath cells in the orbital cavity, which is the bony socket that houses the eye. This condition is commonly associated with Neurofibromatosis Type 1 (NF1), a genetic disorder that causes the development of numerous neurofibromas throughout the body. Orbital neurofibromas can affect people of any age, but they are most commonly diagnosed in childhood or early adulthood. These tumors can vary greatly in size and growth rate, often causing symptoms that impair vision and ocular function.
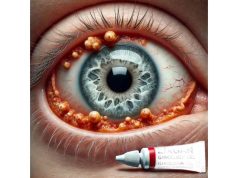
Patients with orbital neurofibromas may experience proptosis (eye bulging), diplopia (double vision), ptosis (eyelid drooping), and, in some cases, vision loss as a result of optic nerve compression. Tumors can also cause disfigurement and discomfort, reducing the patient’s quality of life. A clinical examination, imaging studies such as an MRI or CT scan, and, in some cases, a biopsy are used to confirm the nature of the tumor. Understanding the biological behavior and potential complications of orbital neurofibroma is critical for its successful management and treatment.
Neurofibroma of the Orbit: Management and Treatment
Because of the complexity and potential complications of orbital neurofibroma, management and treatment necessitate a multidisciplinary approach. Standard treatment focuses on symptom relief, vision preservation, and, if possible, tumour removal.
Observation and Monitoring
In cases where the neurofibroma is small and asymptomatic, a conservative approach with regular observation and monitoring may be adopted:
- Periodic Imaging: Regular MRI or CT scans are used to track the tumor’s growth and detect changes in size or morphology.
- Clinical Assessments: Routine eye exams and visual function tests can help track any changes in vision or ocular motility.
Surgical Intervention
Surgery is frequently considered for symptomatic neurofibromas that cause significant pain, functional impairment, or cosmetic issues. Surgery options include:
- Full Resection: The goal is to completely remove the tumor while preserving as much normal tissue and function as possible. However, complete resection can be difficult due to the tumor’s proximity to critical structures such as the optic nerve and extraocular muscles.
- Debulking Surgery: In cases where complete removal is not possible, debulking surgery aims to reduce the tumor’s size in order to alleviate symptoms and improve function.
Pharmacologic Management
Although there is no specific pharmacological treatment for neurofibroma, medications can be used to manage associated symptoms or complications:
- Pain Management: Analgesics and anti-inflammatory medications can help relieve tumor-related pain and discomfort.
- Steroid: Corticosteroids may be prescribed in some cases to reduce inflammation and swelling around the tumor, especially if there is associated edema that impairs vision.
Radiation Therapy
Radiation therapy is typically reserved for cases where surgical options are limited or the tumor is aggressively growing. Stereotactic radiosurgery (SRS) and proton beam therapy are advanced radiation techniques that deliver precise doses to tumors while limiting exposure to healthy tissues.
Genetic Counseling and Support
Given the genetic basis of NF1, genetic counseling is critical for affected people and their families. Counseling can help you understand inheritance patterns, potential risks, and family planning implications.
Cutting-Edge Innovations in Neurofibroma of the Orbit Treatment
Recent advances in the treatment of orbital neurofibroma have opened up new avenues for managing this challenging condition. These innovations include novel pharmacological therapies, advanced surgical techniques, and ground-breaking technologies aimed at improving patient outcomes.
Targeted Molecular Therapies
Targeted molecular therapies are a promising area of innovation in the treatment of orbital neurofibroma. These therapies seek to disrupt specific molecular pathways involved in tumor growth and proliferation:
- MEK Inhibitors: MEK inhibitors, such as selumetinib, have shown great promise in treating neurofibromas caused by NF1. These drugs inhibit the MEK enzyme, which disrupts the abnormal cell signaling pathways that drive tumor growth. Clinical trials have shown that selumetinib can shrink tumors and improve symptoms in patients with NF1-related neurofibromas, providing a non-surgical option for managing the condition.
- mTOR inhibitors: Drugs like sirolimus and everolimus target the mTOR pathway, which is another important regulator of cell growth and proliferation in neurofibromas. These inhibitors have demonstrated the potential to reduce tumor size and stabilize disease progression in NF1 patients.
Advanced Imaging Techniques
Advances in imaging technologies have significantly improved the diagnosis and management of orbital neurofibromas.
- High-Resolution MRI: Newer MRI techniques, such as high-resolution and contrast-enhanced MRI, can produce detailed images of orbital structures and neurofibromas. These advancements enable more precise measurements of tumor size, location, and impact on surrounding tissues, which aids in surgical planning and monitoring.
- Functional Imaging: Techniques such as functional MRI (fMRI) and diffusion tensor imaging (DTI) provide information about the functional impact of neurofibromas on neural pathways and ocular structures. These tools can help determine the risk of vision loss and guide treatment decisions.
Minimal Invasive Surgical Techniques
Innovative surgical techniques have improved the safety and efficacy of tumor resection while minimizing complications.
- Endoscopic Surgery: Endoscopic techniques enable surgeons to access and remove neurofibromas through smaller incisions, lowering surgical trauma and recovery time. Endoscopic techniques improve visualization of the tumor and surrounding structures, allowing for more precise and effective resection.
- Image-guided Surgery: Intraoperative imaging systems, such as MRI and CT, provide real-time images during surgery, allowing surgeons to navigate complex anatomy and ensure complete tumor removal. These systems improve resection accuracy while lowering the risk of damaging critical structures.
Personalized Medical Approaches
Personalized medicine is playing an increasingly important role in the treatment of orbital neurofibroma. Personalized medicine can improve treatment outcomes by tailoring therapies to each patient’s and tumor’s unique characteristics:
- Genetic Profiling: Genetic testing and profiling can help identify specific mutations and molecular targets in neurofibromas. This data can be used to guide the selection of targeted therapies as well as predict treatment response, allowing for more effective patient management.
- Biomarker Identification: Researchers are working to identify biomarkers that indicate tumor behavior and response to treatment. These biomarkers can assist in monitoring disease progression and adjusting treatment plans accordingly.
Immunotherapy
Immunotherapy, which uses the body’s immune system to fight cancer, is being investigated as a possible treatment for orbital neurofibroma.
- Immune checkpoint inhibitors: Immune checkpoint inhibitors, such as PD-1 and CTLA-4, have shown promise in treating a variety of cancers. Their ability to target neurofibromas by enhancing the immune response against tumor cells is being studied.
- Adoptive Cell Therapy: This method entails programming a patient’s immune cells to recognize and attack tumor cells. Early research indicates that adoptive cell therapy may be a viable option for treating neurofibromas, particularly those that are resistant to conventional treatments.
Nanotechnology-Based Treatments
Nanotechnology provides innovative solutions for delivering treatments directly to tumor cells, increasing efficacy while reducing side effects:
- Nanoparticle Drug Delivery: Anti-cancer drugs can be engineered into nanoparticles and delivered directly to neurofibroma cells. This targeted delivery system increases drug concentration at the tumour site while reducing exposure to healthy tissues.
- Theranostic Nanoparticles: These multifunctional nanoparticles have both therapeutic and diagnostic capabilities, allowing for real-time monitoring of treatment response and therapy adjustments as needed.
Future Directions in Research
Ongoing research is exploring new avenues for treating orbital neurofibroma, with several promising directions:
- Gene Therapy: Gene therapy seeks to correct the underlying genetic defects that contribute to neurofibromatosis and neurofibroma development. Gene therapy, which delivers functional copies of defective genes or silences harmful mutations, has the potential to provide a long-term solution for neurofibromas.
- Stem Cell Treatment: Stem cell-based therapies have the potential to regenerate damaged tissues and restore normal functionality. Researchers are looking into using stem cells to repair and replace affected orbital structures, which could provide hope for patients with advanced disease.