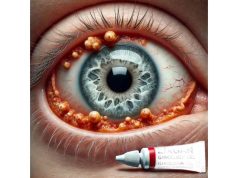
Ocular hypertension is a condition characterized by high intraocular pressure (IOP) in the eye, which increases the risk of developing glaucoma, a serious eye disease that can cause vision loss and blindness. Unlike glaucoma, ocular hypertension does not initially damage the optic nerve or cause vision changes. However, people with ocular hypertension are more likely to develop glaucoma over time. The balance of aqueous humor production and drainage determines intraocular pressure. When this balance is disturbed, pressure within the eye can rise.
The exact cause of ocular hypertension is not always known, but it can be linked to factors such as increased aqueous humor production, decreased drainage through the trabecular meshwork, certain medications, eye trauma, and other medical conditions. Regular eye exams are essential for detecting ocular hypertension, especially since the condition frequently manifests without obvious symptoms. During these exams, an ophthalmologist measures IOP with tonometry, assesses the drainage angle, and examines the optic nerve and visual field for signs of glaucoma.
Early detection and treatment of ocular hypertension are critical for preventing the progression to glaucoma and maintaining vision. Patients with ocular hypertension need close monitoring and, in some cases, treatment to lower intraocular pressure and reduce the risk of optic nerve damage.
The primary goal of managing and treating ocular hypertension is to lower intraocular pressure in order to reduce the risk of developing glaucoma. Standard treatment methods include pharmacological therapies, laser treatments, and surgical interventions, depending on the severity of the condition and the patient’s specific needs.
Pharmacologic Treatments
Pharmacological treatments are the first line of defense against ocular hypertension. These medications reduce intraocular pressure by either decreasing aqueous humor production or increasing its outflow.
Prostaglandin Analogs: Prostaglandin analogs, such as latanoprost, bimatoprost, and travoprost, are frequently used to increase aqueous humor outflow via the uveoscleral pathway. These medications are typically administered as eye drops and are extremely effective in lowering IOP with few systemic side effects.
Beta Blockers: Beta blockers, such as timolol and betaxolol, inhibit beta-adrenergic receptors in the ciliary body, reducing aqueous humor production. These medications are also available as eye drops, and they are frequently used in conjunction with prostaglandin analogs to improve IOP reduction.
Alpha Agonists: Alpha agonists, like brimonidine and apraclonidine, reduce aqueous humor production while increasing uveoscleral outflow. These medications are typically used as a supplement to prostaglandin analogs and beta blockers.
Carbonic Anhydrase Inhibitors: Carbonic anhydrase inhibitors, including dorzolamide and brinzolamide, reduce aqueous humor production by inhibiting the enzyme carbonic anhydrase. These drugs can be given as eye drops or orally, depending on the patient’s response and tolerance.
Laser Treatments
Laser treatments provide a non-invasive method for lowering intraocular pressure in patients with ocular hypertension. These procedures aim to improve aqueous humor drainage through the trabecular meshwork or to open up new drainage pathways.
Selective Laser Trabeculoplasty (SLT): A low-energy laser targets and stimulates trabecular meshwork cells, increasing aqueous humor outflow. This procedure is typically performed in an outpatient setting and has a good safety profile, with little discomfort and a low risk of complications.
Argon Laser Trabeculoplasty (ALT) is an older laser technique that improves aqueous humor outflow by targeting the trabecular meshwork. While effective, ALT is less commonly used than SLT due to the increased risk of tissue damage and side effects.
Surgical Interventions
Patients with ocular hypertension who do not respond well to medication or laser treatment may require surgical intervention. These procedures seek to create new drainage pathways or improve existing ones in order to reduce intraocular pressure.
Trabeculectomy: A trabeculectomy is a common surgical procedure that involves removing a portion of the trabecular meshwork and sclera to create a new drainage pathway for aqueous humor. This procedure can effectively lower IOP, but it is associated with risks such as infection, bleeding, and scarring, all of which can have an impact on long-term outcomes.
Glaucoma Drainage Devices: Glaucoma drainage devices, such as shunts and implants, divert aqueous humor from the anterior chamber to an external reservoir, lowering intraocular pressure. These devices are especially useful for patients suffering from refractory ocular hypertension or secondary glaucoma.
** Minimally Invasive Glaucoma Surgery (MIGS)**: MIGS procedures, including the iStent, Xen Gel Stent, and Trabectome, provide less invasive alternatives to traditional glaucoma surgeries. These methods involve implanting tiny devices to improve aqueous humor outflow with fewer complications and shorter recovery times.
Breakthrough Innovations in Ocular Hypertension Treatment
Recent advances in the treatment of ocular hypertension have significantly improved patient outcomes, providing new hope to those at risk of developing glaucoma. Innovative therapies, advanced diagnostic tools, and novel pharmacological approaches are revolutionizing the treatment of ocular hypertension.
Genetic Therapy
Gene therapy is a new field with promising applications in the treatment of ocular hypertension. This method entails delivering specific genes to the eye to alter the production or drainage of aqueous humor. Researchers are investigating the use of viral vectors to introduce genes that increase or decrease the production of aqueous humor. Early-phase clinical trials have yielded promising results, indicating that gene therapy may provide a long-term solution for managing ocular hypertension with fewer side effects than traditional medications.
Stem Cell Therapy
Stem cell therapy represents a regenerative approach to treating ocular hypertension. Mesenchymal stem cells (MSCs) have demonstrated the ability to repair and regenerate the trabecular meshwork, the primary drainage pathway for aqueous humor. Researchers hope that injecting MSCs into the eye will restore normal trabecular meshwork function, improve aqueous humor outflow, and lower intraocular pressure. Preclinical studies have shown that stem cells can integrate into the trabecular meshwork, improving its function. Clinical trials are currently underway to determine the safety and efficacy of stem cell therapy in ocular hypertension patients.
Nanotechnology
Nanotechnology is transforming the delivery of drugs and therapeutic agents to the eye. Nanoparticles can be engineered to deliver anti-glaucoma medications directly to the trabecular meshwork, increasing efficacy while reducing systemic side effects. For example, nanoparticles loaded with prostaglandin analogs or other IOP-lowering agents can provide medication release over time, reducing the need for frequent eye drops. Furthermore, nanotechnology-based approaches are being developed to deliver gene therapy vectors and stem cells to the trabecular meshwork, increasing the precision and efficacy of these therapies.
Artificial Intelligence, Machine Learning
The diagnosis and treatment of ocular hypertension are incorporating artificial intelligence (AI) and machine learning (ML). AI algorithms can analyze imaging data from optical coherence tomography (OCT) and other diagnostic tools to detect early signs of high intraocular pressure and predict the likelihood of developing glaucoma. Machine learning models can help develop personalized treatment plans based on patient-specific information, thereby improving outcomes and lowering the risk of complications. These technologies improve diagnostic accuracy and treatment effectiveness.
Advanced Imaging Techniques
Advanced imaging techniques improve the ability to detect and monitor ocular hypertension. Optical coherence tomography angiography (OCTA) is a non-invasive imaging technique that produces detailed images of the retinal vasculature without the use of dye injections. OCTA can detect early changes in the retinal blood vessels, allowing for more timely diagnosis and intervention. Furthermore, ultra-widefield imaging techniques are being used to capture comprehensive views of the retina, which will aid in the detection of peripheral lesions associated with ocular hypertension.
Novel Pharmaceutical Agents
New pharmacological agents are being developed to target specific pathways involved in the development of ocular hypertension. For example, rho kinase inhibitors like netarsudil have been shown to improve aqueous humor outflow through the trabecular meshwork by relaxing the actin cytoskeleton. These agents have a novel mechanism of action for lowering intraocular pressure and can be used alone or with other medications. Other novel agents, including adenosine receptor agonists and endothelin receptor antagonists, are being studied for their ability to lower intraocular pressure and prevent the progression of ocular hypertension to glaucoma.
Personalized Medicine
Personalized medicine approaches are being investigated to tailor treatment plans to individual patients’ genetic and molecular profiles. Understanding the specific genetic and molecular factors that contribute to ocular hypertension in each patient allows clinicians to develop more targeted and effective treatment strategies. Personalized medicine has the potential to improve treatment outcomes while lowering the risk of side effects, providing a more precise approach to managing ocular hypertension.
Telemedicine & Remote Monitoring
Telemedicine and remote monitoring technologies are expanding access to care for patients with ocular hypertension. Telemedicine platforms support virtual consultations, allowing patients to receive expert advice and follow-up care without the need for in-person visits. Remote monitoring devices, such as smartphone-based imaging tools, enable patients to track their intraocular pressure while receiving real-time feedback from their healthcare providers. These technologies improve care continuity and intervention timing, resulting in better overall treatment outcomes.
Integrative Medicine
Integrative medicine approaches are gaining popularity because of their potential benefits in treating ocular hypertension. Acupuncture, herbal medicine, and dietary changes are being studied for their ability to lower intraocular pressure, boost immune function, and improve overall well-being. Integrative therapies can supplement traditional treatments, offering a more comprehensive approach to ocular hypertension management.