Pigmentary glaucoma is a type of secondary open-angle glaucoma defined by the dispersion of pigment granules within the eye, which can obstruct the drainage system (trabecular meshwork) and cause increased intraocular pressure (IOP). This high pressure can damage the optic nerve, potentially resulting in vision loss. The condition typically develops between the ages of 20 and 50, and it is more common in men and those with myopia (nearsightedness).
Pigment dispersion syndrome (PDS) is the precursor to pigmentary glaucoma, which occurs when pigment granules are released from the iris into the anterior chamber of the eye. This dispersion can be asymptomatic at first, but it can progress to pigmentary glaucoma if the pigment obstructs the trabecular meshwork, preventing the outflow of aqueous humor and raising IOP. Symptoms of pigmentary glaucoma include blurred vision, halos around lights, eye pain, and intermittent episodes of high IOP.
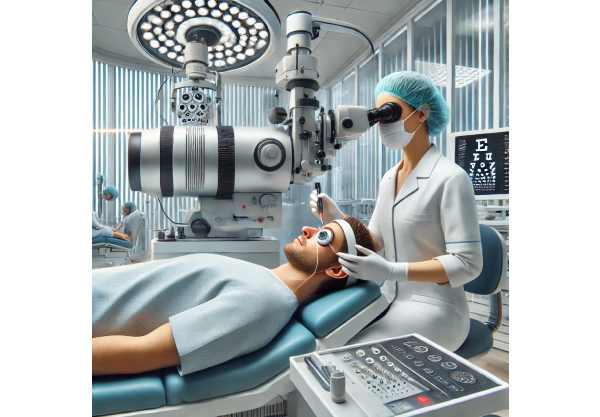
A comprehensive eye examination is required to diagnose pigmentary glaucoma, which includes gonioscopy to examine the anterior chamber angle, tonometry to measure IOP, and optical coherence tomography (OCT) to evaluate the optic nerve and retinal nerve fiber layer. A thorough medical history, as well as a slit-lamp examination, are required to identify specific pigment deposits on the corneal endothelium, lens, and trabecular meshwork.
Traditional Pigmentary Glaucoma Treatments
The management and treatment of pigmentary glaucoma center on lowering intraocular pressure in order to prevent optic nerve damage and preserve vision. Standard treatment methods usually include a combination of medical, laser, and surgical approaches tailored to the severity of the condition.
Medical Management: The initial treatment for pigmentary glaucoma frequently consists of topical medications that lower IOP. These medications include:
- Prostaglandin Analogues: Drugs like latanoprost and bimatoprost increase the outflow of aqueous humor via the uveoscleral pathway, lowering IOP.
- Beta-Blockers: Medications such as timolol inhibit beta-adrenergic receptors in the ciliary body, reducing aqueous humor production.
- Alpha Agonists: Drugs like brimonidine reduce aqueous humor production while increasing uveoscleral outflow.
- Carbonic Anhydrase Inhibitors: Both topical (dorzolamide) and oral (acetazolamide) formulations suppress aqueous humor production by inhibiting the carbonic anhydrase enzyme.
Laser Therapy: Laser treatments can help manage pigmentary glaucoma, especially when medical treatment is insufficient.
- Laser Trabeculoplasty: SLT and ALT target the trabecular meshwork to improve aqueous outflow. SLT is frequently preferred for its low risk of thermal damage and repeatability.
- Laser Peripheral Iridotomy: This procedure makes a small hole in the peripheral iris, allowing aqueous humor to flow directly from the posterior to the anterior chamber, thereby reducing iris bowing and pigment release.
Surgical Intervention: If medications and laser therapy fail to provide adequate IOP control, surgery may be required.
- Trabeculectomy: This filtration surgery opens up a new drainage pathway for aqueous humor, lowering IOP by allowing fluid to exit the eye via a bleb formed beneath the conjunctiva.
- Glaucoma Drainage Devices: Implants like the Ahmed or Baerveldt devices offer an alternative route for aqueous humor drainage that avoids the trabecular meshwork.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures, such as the implantation of the iStent or the use of the Trabectome, seek to reduce IOP with less tissue disruption and faster recovery times than traditional surgeries.
Monitoring and Follow-Up: Regular follow-up visits are essential for monitoring IOP, assessing optic nerve health, and adjusting treatment as necessary. Visual field testing and OCT scans are critical for monitoring disease progression and assessing the efficacy of treatment interventions.
Latest Advances in Pigmentary Glaucoma
Recent advances in medical research and technology have resulted in significant improvements to the treatment and management of pigmentary glaucoma. These cutting-edge approaches aim to increase therapeutic efficacy, reduce complications, and improve patients’ quality of life. Below, we look at some of the most effective and innovative treatments for pigmentary glaucoma.
Gene Therapy and Genetic Research
Gene therapy and genetic research are promising approaches to treating pigmentary glaucoma. These novel approaches seek to address the underlying genetic factors that contribute to the disease, with the potential for long-term and even curative results.
CRISPR/Cas9 Gene Editing: CRISPR-Cas9 is a revolutionary gene-editing technology that enables precise modification of specific genetic sequences. Researchers are looking into the ability of CRISPR-Cas9 to correct genetic mutations linked to pigment dispersion and glaucoma. Preclinical studies have yielded promising results, suggesting that future clinical applications could provide long-term relief for patients with a genetic predisposition to pigmentary glaucoma.
Gene Therapy: Viral vectors can deliver functional copies of defective genes to affected cells. In the case of pigmentary glaucoma, gene therapy aims to restore normal gene function while decreasing pigment dispersion. Current clinical trials are assessing the safety and efficacy of this approach in conditions such as pigment dispersion syndrome and other inherited ocular disorders.
Advanced Drug Delivery Systems
Drug delivery system innovations have created new solutions for managing pigmentary glaucoma, providing patients with better protection and comfort.
Sustained-release Implants: Sustained-release implants, like the bimatoprost implant (Durysta), provide long-term drug delivery to the eye. These implants are inserted into the anterior chamber and gradually release medication, reducing the need for daily eye drops and increasing patient compliance.
Nanoparticle-Based Delivery: Nanoparticle-based drug delivery systems provide targeted and sustained release of medications, improving therapeutic efficacy and reducing side effects. Researchers are investigating the use of nanoparticles to deliver anti-glaucoma drugs directly to the trabecular meshwork, which could result in more effective IOP reduction and pigment dispersion control.
Minimal Invasive Glaucoma Surgery (MIGS)
Advancements in surgical techniques have resulted in the development of minimally invasive glaucoma surgeries (MIGS), which reduce surgical trauma, improve recovery, and improve outcomes for patients with pigmentary glaucoma.
iStent Inject: The iStent Inject is a small implant inserted into the trabecular meshwork to improve aqueous outflow. This device has been shown to effectively reduce IOP with less surgical trauma and shorter recovery times than traditional surgeries.
Hydrus Microstent: The Hydrus Microstent is a flexible, scaffold-like device that dilates and supports the trabecular meshwork, thereby increasing aqueous outflow. Clinical trials have shown that this minimally invasive approach reduces IOP significantly and increases patient satisfaction.
The Kahook Dual Blade (KDB): The KDB is a new surgical tool for performing goniotomy, a procedure that removes a portion of the trabecular meshwork to improve aqueous outflow. The KDB enables precise and controlled tissue removal, lowering IOP effectively and safely.
Laser Technologies
Laser technology advancements have created new options for treating pigmentary glaucoma that are more effective and safe.
Micropulsed Laser Trabeculoplasty (MLT): MLT is a more recent type of laser trabeculoplasty that employs a low-energy micropulse laser to target the trabecular meshwork. This technique reduces thermal damage and inflammation, resulting in effective IOP reduction with fewer side effects than conventional laser treatments.
PSLT (pattern scanning laser trabeculoplasty): PSLT employs a pattern-scanning laser to provide precise and controlled energy to the trabecular meshwork. This technology enables more consistent and uniform treatment, which improves the efficacy and safety of laser trabeculoplasty for pigmentary glaucoma patients.
Neuroprotection and Preservation of Retinal Ganglion Cells (RGC)
Neuroprotective strategies seek to protect retinal ganglion cells (RGCs) from degeneration, opening up new possibilities for managing pigmentary glaucoma and maintaining vision.
Brimonidine: Brimonidine, an alpha-2 adrenergic agonist, has neuroprotective properties in addition to its IOP-lowering effects. According to studies, brimonidine can improve RGC survival and visual outcomes in glaucoma patients, making it an important adjunct therapy for pigmentary glaucoma.
Ciliary Neurotrophic Factor (CNTF) is a neurotrophic factor that promotes the survival and function of RGCs. Researchers are investigating the ability of CNTF, delivered via gene therapy or other methods, to protect and regenerate RGCs in glaucoma patients. Early-stage clinical trials have yielded promising results, with additional research underway to optimize delivery methods and dosing.






