What is Pterygium?
Pterygium is a benign growth of the conjunctiva, the clear tissue that lines the inside of the eyelids and protects the white part of the eye. This growth spreads to the cornea, the transparent front part of the eye, and can cause a range of symptoms such as redness, irritation, and vision problems. Pterygium, also known as “surfer’s eye,” is associated with excessive exposure to ultraviolet (UV) light, wind, and dust, all of which irritate the eye’s surface.
A pterygium typically appears as a triangular, fleshy mass of variable size. In mild cases, it may not cause significant discomfort or vision problems; however, as it grows, it can distort the cornea, causing astigmatism or even obscuring vision if it grows above the pupil. Although the condition is usually not cancerous, it can be bothersome and cosmetically unappealing, prompting people to seek treatment.
Pterygium is more common in people who live in sunny climates or spend a lot of time outside without proper eye protection. Wearing UV-protective sunglasses and hats can help protect your eyes from direct sunlight. Understanding pterygium, its causes, and symptoms is critical for early detection and effective treatment, allowing people to maintain good ocular health and avoid complications.
Standard Methods for Pterygium Management
The severity of the symptoms and the extent of the growth determine the management and treatment of pterygium. In many cases, pterygium can be treated conservatively to alleviate symptoms and prevent further progression. However, more severe cases may necessitate surgical intervention.
Conservative Treatments
Conservative treatment is often adequate for mild cases of pterygium, where the growth is small and does not cause significant symptoms. This usually includes:
- Lubricating Eye Drops: Artificial tears can relieve the dryness and irritation caused by pterygium. They have a soothing effect and relieve the sensation of grittiness or foreign bodies in the eye.
- Anti-inflammatory Medications: Topical corticosteroids or nonsteroidal anti-inflammatory drops may be prescribed to alleviate inflammation and redness. To avoid potential side effects, these medications are typically prescribed for short periods of time.
- UV Protection: Wearing UV-blocking sunglasses and wide-brimmed hats can help prevent future growth and protect the eyes from environmental irritants.
Surgical Treatments
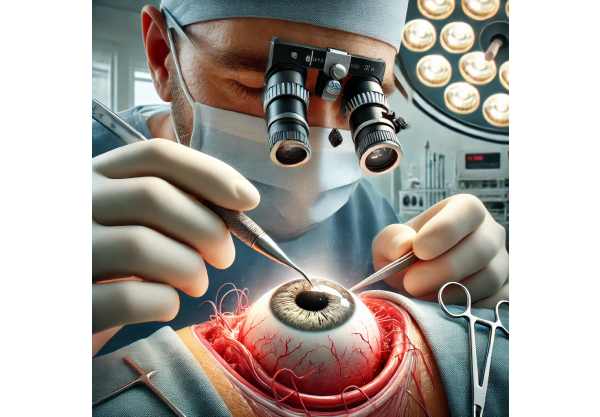
When pterygium causes severe discomfort, vision problems, or cosmetic issues, surgical removal may be required. There are several surgical techniques available, and the choice is based on the size and location of the pterygium, as well as the patient’s overall eye health.
- Excision with Conjunctival Autograft: This is the most common and effective surgical method for pterygium removal. The pterygium is carefully excised, and a graft of the patient’s own conjunctival tissue is taken from a healthy part of the eye and used to cover the pterygium removal site. This method significantly lowers the risk of recurrence.
- Amniotic Membrane Transplantation: In some cases, an amniotic membrane graft may replace a conjunctival autograft. The amniotic membrane contains anti-inflammatory and anti-scarring properties that aid in healing and reduce the likelihood of recurrence.
- Bare Sclera Technique: This older method simply removes the pterygium, exposing the underlying sclera (white part of the eye). However, this technique has a higher recurrence rate than grafting techniques.
Post-operative Care
Postoperative care is critical for successful outcomes, which includes the use of topical antibiotics and anti-inflammatory medications to prevent infection and inflammation. Patients should also avoid activities that may irritate the eye and use UV protection to avoid recurrence.
Innovative Approaches to Pterygium Treatment
Recent advances in pterygium treatment have significantly improved surgical outcomes and decreased the rate of recurrence, which is a common issue in managing this condition. These innovations include new surgical techniques, advanced medical therapies, and enhanced preventive measures.
Minimal Invasive Surgical Techniques
Minimally invasive approaches have transformed pterygium surgery, providing patients with less discomfort and shorter recovery times. These techniques frequently use smaller incisions and more precise pterygium excision, which reduces eye trauma.
- Sutureless and Glue-Free Techniques: Sutures are frequently used in traditional pterygium surgery to secure the graft in place, which can be uncomfortable and slow recovery. Newer techniques eliminate the need for sutures by securing the conjunctival autograft with tissue adhesives such as fibrin glue. This method reduces postoperative discomfort and accelerates the healing process.
- Microincision Surgery: Advances in surgical instruments have allowed for the development of microincision techniques, which involve making extremely small cuts to remove the pterygium. This minimally invasive approach reduces tissue damage and improves recovery.
Amniotic Membrane and Stem Cell Therapies
The use of biological materials such as amniotic membrane and stem cells has shown promise for improving pterygium surgery outcomes.
- Amniotic Membrane Transplantation (AMT): The placental amniotic membrane is naturally anti-inflammatory and anti-scarring. Its use in pterygium surgery reduces inflammation, promotes healing, and lowers the likelihood of recurrence. AMT can be especially useful for recurrent pterygium cases or those with extensive tissue damage.
- Stem Cell Therapy: Research into stem cell therapy for pterygium treatment is currently underway. Stem cells have the ability to regenerate damaged tissue and restore the normal ocular surface anatomy. While still in the experimental stages, stem cell-based treatments may provide a future solution for severe or recurring pterygium.
Pharmaceutical Advances
Pharmacological advances have resulted in the development of new medications and therapies to help with pterygium treatment and recurrence prevention.
- Anti-VEGF Therapy: Vascular endothelial growth factor (VEGF) aids in the formation of new blood vessels, which can promote pterygium growth. Anti-VEGF medications, which are commonly used to treat age-related macular degeneration, are being studied as pterygium treatments to inhibit abnormal blood vessel growth and reduce recurrence.
- Mitomycin C: Mitomycin C is an antimetabolite medication used to reduce scarring and recurrence following pterygium surgery. It is applied topically during surgery to prevent fibroblast proliferation, which is a major factor in pterygium recurrence. Due to the potential for side effects, careful application and monitoring are required.
Laser-Assisted Techniques
Pterygium treatment is incorporating laser technology to improve precision and reduce recurrence rates.
- Excimer Laser: The excimer laser can precisely ablate the pterygium tissue and smooth the corneal surface, lowering the risk of recurrence. This technique provides greater control and accuracy than traditional surgical methods.
- Phototherapeutic Keratectomy (PTK): PTK is a laser procedure that corrects superficial corneal irregularities caused by pterygium. It can work in tandem with surgical excision to improve corneal clarity and visual outcomes.
Gene Therapy and Molecular Research
Gene therapy and molecular research are emerging fields that show promise for treating pterygium by addressing the condition’s underlying genetic and molecular mechanisms.
- Gene Editing Technologies: Methods such as CRISPR-Cas9 are being investigated to modify genes involved in pterygium development and progression. This approach has the potential to prevent the development or recurrence of pterygium by addressing the underlying genetic causes.
- Molecular Pathways: Understanding the molecular pathways that drive pterygium growth and recurrence is essential for developing targeted therapies. The research aims to identify key molecules and signaling pathways that contribute to pterygium pathogenesis, paving the way for new treatments.
Preventive Strategies
Preventive strategies are critical for reducing the incidence and recurrence of pterygium. Advances in public health awareness and protective measures have contributed significantly to the management of this condition.
- Enhanced UV Protection: UV-blocking sunglasses and protective eyewear are becoming more widely available, providing better protection from the harmful effects of UV radiation. Public health campaigns emphasize the importance of eye protection, particularly for people working in high-risk environments.
- Environmental Modifications: Taking steps to reduce exposure to dust, wind, and other environmental irritants in the workplace and recreational settings can help prevent the development of pterygium. Implementing measures such as providing protective barriers and encouraging the use of protective eyewear can significantly lower the risk.






