What is retinoschisis?
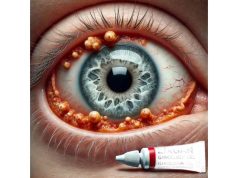
Retinoschisis is an eye condition characterized by the splitting of retinal layers, which causes vision impairment. The term “retinoschisis” comes from Greek, which means “splitting of the retina.” This condition can be either congenital (juvenile retinoschisis) or acquired (senile retinoschisis). Juvenile retinoschisis is a hereditary disorder that primarily affects men due to its X-linked recessive inheritance pattern. This type of retinoschisis usually appears in childhood or adolescence and can cause progressive vision loss if left untreated.
The retina is a light-sensitive layer of tissue at the back of the eye that is responsible for converting light into neural signals sent to the brain. Retinoschisis occurs when retinal layers split, most commonly between the nerve fiber layer and the outer plexiform layer. This separation can cause cystic changes and degenerative alterations in the retina, affecting the individual’s visual acuity and field of view.
Retinoschisis symptoms vary according to the severity and location of the retinal splitting. Common symptoms include blurred vision, difficulty with central or peripheral vision, and, in some cases, the presence of floaters. In severe cases, retinoschisis can result in complications such as retinal detachment, which can jeopardize vision. A comprehensive eye examination, including optical coherence tomography (OCT) and electroretinography (ERG), is usually required to diagnose the extent of retinal involvement and guide treatment strategies.
Standard Retinoschisis Care and Treatment
Managing and treating retinoschisis requires a variety of strategies aimed at maintaining vision and avoiding complications. Given the nature of the condition, treatment options range from regular monitoring to surgical intervention, depending on the disease’s severity and progression.
- Observation and Monitoring: Many people with retinoschisis, particularly those with mild cases or few symptoms, require regular observation and monitoring. Periodic examinations are typically performed by eye care professionals to monitor changes in the structure and function of the retina. This approach allows for timely intervention if the condition worsens or complications develop.
- Protective Eyewear: Patients, particularly children with juvenile retinoschisis, should wear protective eyewear to avoid eye trauma. Physical injuries can exacerbate retinal splitting or cause retinal detachment, so protecting the eyes from impact is an important preventive measure.
- Vision Aids: Low vision aids and devices can be useful for people who have significant vision impairment due to retinoschisis. These aids include magnifying glasses, specialized reading lamps, and electronic devices that improve patients’ visual capabilities and help them maintain a high quality of life.
- Laser Therapy: In some cases, laser photocoagulation can be used to treat retinal detachment-prone areas. This procedure involves using laser energy to create small burns around the retinal tears, which help to seal the edges and prevent future separation. Laser therapy can help to stabilize the retina and reduce the risk of more serious complications.
- Vitrectomy: A vitrectomy is a surgical procedure that removes the vitreous gel from the eye and replaces it with a saline solution or gas bubble. This method is especially beneficial for patients with advanced retinoschisis or who develop retinal detachment. By removing the vitreous gel, the surgeon can relieve traction on the retina and make it easier to reattach. Vitrectomy is a complex and risky procedure, but it is frequently required to preserve vision in severe cases.
- Scleral Buckling: Scleral buckling is another surgical option for treating retinoschisis complications, such as retinal detachments. This procedure entails wrapping a silicone band around the eye’s exterior to indent the sclera (white part) and bring the retinal layers back together. Scleral buckling can help reattach the retina and stabilize its structure.
- Pharmacological Treatments: There are currently no approved medications for treating retinoschisis. However, research is underway to investigate potential pharmacological interventions to help manage the condition. Anti-VEGF (vascular endothelial growth factor) drugs, which are commonly used to treat other retinal conditions, are being studied for their potential use in treating retinoschisis-related complications.
- Genetic Counseling and Testing: Genetic counseling and testing are critical for people diagnosed with juvenile retinoschisis. Identifying the specific genetic mutations that cause the condition can aid in understanding inheritance patterns and risk assessment for family members. Genetic counseling offers important information for family planning and early detection in at-risk individuals.
Advanced Retinoschisis Treatment Techniques
The treatment landscape for retinoschisis has changed dramatically in recent years, thanks to breakthroughs in genetic research, advanced imaging technologies, and novel therapeutic approaches. These cutting-edge innovations aim to improve the management of retinoschisis, giving patients new hope for better outcomes and a higher quality of life.
Gene Therapy: Addressing the Root Cause
Gene therapy is one of the most promising areas of medical innovation for retinoschisis. Given that juvenile retinoschisis is caused by mutations in the RS1 gene, gene therapy seeks to correct these genetic flaws at the molecule level. Researchers are looking into different gene delivery methods to get functional copies of the RS1 gene into retinal cells.
- Adeno-Associated Viral (AAV) Vectors: AAV vectors are popular in gene therapy because of their safety and ability to deliver genetic material to target cells. In retinoschisis, AAV vectors are designed to carry the RS1 gene and deliver it to retinal cells, where it can express the protein required to restore normal retinal function. Preclinical studies have yielded promising results, and clinical trials are currently underway to determine the efficacy and safety of AAV-mediated gene therapy for retinoschisis.
- CRISPR-Cas9 Gene Editing: CRISPR-Cas9 technology enables precise genome editing, potentially correcting RS1 gene mutations directly. CRISPR-Cas9 allows researchers to target and repair the defective gene, potentially providing a long-term solution for retinoschisis. While still in the experimental stage, CRISPR-Cas9 shows great promise for treating genetic retinal disorders.
Advanced Imaging Technologies for Better Diagnosis and Monitoring
Accurate diagnosis and monitoring of retinoschisis are critical for successful treatment. Advanced imaging technologies have transformed the ability to visualize retinal structures in detail, facilitating early detection and ongoing assessment of the condition.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. OCT has become a standard tool for diagnosing and monitoring retinoschisis, allowing clinicians to see through the retinal layers and detect any splitting or cystic changes. Enhanced OCT technologies, such as swept-source OCT and OCT angiography, provide even more detail and depth of analysis, boosting diagnostic accuracy and treatment planning.
- Ultra-Widefield Imaging: Traditional retinal imaging techniques have limited field of view and frequently miss peripheral retinal changes. The Optos system, for example, uses ultra-widefield imaging to capture images of the entire retina in one scan. This comprehensive view enables better detection of peripheral retinoschisis and its complications, resulting in more effective management.
Pharmacological Innovation: New Therapeutic Approaches
While no specific drugs have been approved for retinoschisis, ongoing research is looking into potential pharmacological treatments to help mitigate the condition’s effects and prevent complications.
- Anti-VEGF Therapy: Anti-VEGF agents, such as bevacizumab and ranibizumab, have shown promise in treating a variety of retinal conditions by preventing abnormal blood vessel growth. Researchers are looking into the use of anti-VEGF therapy to treat retinoschisis complications like retinal neovascularization and macular edema. Early research indicates that these agents may help stabilize retinal structures and improve visual outcomes.
- Neuroprotective Agents: Neuroprotective drugs aim to prevent retinal cell degeneration and increase their survival. Compounds such as N-acetylcysteine (NAC) and minocycline are being investigated for their neuroprotective properties in retinoschisis. These agents may help preserve retinal function and slow disease progression, making them a potential adjunctive treatment for patients with retinoschisis.
Surgical Innovation: Improving Outcomes
Surgical interventions for retinoschisis have also advanced significantly, with new techniques and technologies improving the safety and efficacy of the procedures.
- Microincision Vitrectomy Surgery (MIVS): MIVS involves performing vitrectomy with smaller instruments and incisions, which reduces eye trauma and promotes faster recovery. This technique is especially beneficial for pediatric patients with juvenile retinoschisis because it reduces the risk of complications while improving surgical outcomes.
- Robotic-Assisted Surgery: Robotic systems are being developed to aid in delicate retinal surgeries by increasing precision and control. These systems can perform intricate maneuvers with greater precision than human hands, potentially increasing the success rate of complex procedures like vitrectomy and retinal reattachment. Robotic surgery represents a significant advancement in the surgical treatment of retinoschisis.