Squamous cell carcinoma (SCC) of the eyelid is a malignant tumor that develops from squamous cells, which are flat cells that line the skin’s surface. It is the second most common type of eyelid cancer, trailing only basal cell carcinoma, accounting for 5-10% of all cases. SCC of the eyelid usually begins in the epidermal layer of the skin and has the potential to invade deeper tissues and metastasize to regional lymph nodes or distant sites if not treated promptly.
The condition primarily affects older adults, particularly those with fair skin, a history of prolonged sun exposure, or risk factors such as immunosuppression or prior radiation therapy. Clinically, SCC of the eyelid can appear as a persistent, non-healing ulcer, a raised nodule, or a flat, scaly lesion. The affected area may be prone to bleeding, crusting, and discomfort. In some cases, the pigmented lesion may resemble other skin conditions, complicating the diagnosis.
The diagnosis of SCC of the eyelid requires a thorough clinical examination by an ophthalmologist or dermatologist, as well as a biopsy of the lesion to confirm the presence of malignant cells. Imaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI), can be used to determine the extent of local invasion and rule out metastasis. Early detection and treatment are critical for preventing significant morbidity and maintaining visual function.
Management and treatment of squamous cell carcinoma of the eyelid
The goal of managing and treating squamous cell carcinoma of the eyelid is to remove the tumor completely, prevent recurrence, and maintain the eyelid’s function and appearance. The size, location, and extent of the tumor, as well as the patient’s overall health and preferences, all influence the treatment decision. Standard treatment options include surgical excision, Mohs micrographic surgery, cryotherapy, and radiation therapy.
Surgical Excision
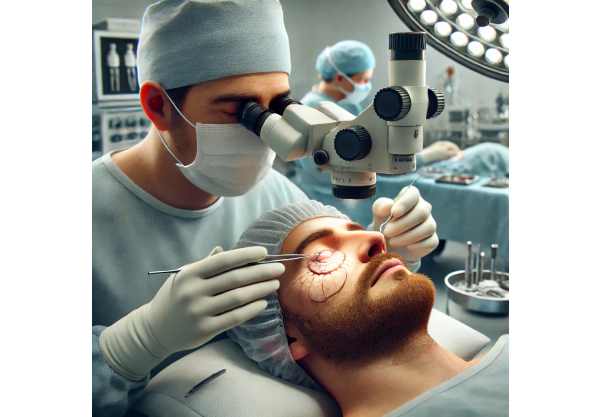
The most common treatment for eyelid skin cancer is surgical excision. The tumor is completely removed, along with a margin of healthy tissue, to ensure that all cancerous cells are eliminated. Histological examination of the excised tissue confirms the presence of clear margins. Depending on the tumor’s size and location, reconstructive surgery may be required to restore the eyelid’s normal appearance and function. This can include skin grafts, local flaps, and complex oculoplastic procedures.
Mohs Micrographic Surgery
Mohs micrographic surgery is the gold standard for treating eyelid SCC, especially for tumors with ill-defined borders, recurrent cases, or those located in cosmetically or functionally sensitive areas. This technique entails precisely removing the tumor layer by layer, with immediate microscopic examination of each layer to ensure complete cancer removal while preserving as much healthy tissue as possible. Mohs surgery has a high cure rate and reduces the risk of recurrence, making it an excellent treatment option for eyelid SCC.
Cryotherapy
Cryotherapy, also known as cryosurgery, is a minimally invasive treatment that destroys cancerous cells using extreme cold. Liquid nitrogen or other cryogenic agents are applied to the tumor, freezing and killing the malignant cells. Cryotherapy is frequently used for small, superficial tumors or as a supplement to other treatment options. While the procedure is relatively simple and quick, it may take several sessions to completely remove the tumor.
Radiation Therapy
Radiation therapy is an alternative treatment for patients who are not candidates for surgery due to medical comorbidities or have tumors that are difficult to remove surgically. This technique employs high-energy radiation to target and destroy cancer cells. External beam radiation therapy and brachytherapy (internal radiation) are both widely used techniques. Radiation therapy can effectively control tumors, but it can also cause skin changes, eyelid inflammation, and, in rare cases, secondary malignancies.
Topical Chemotherapy
Topical chemotherapy with agents such as 5-fluorouracil (5-FU) or imiquimod may be used to treat superficial SCC or as an adjunct to surgical treatment. These medications are administered directly to the tumor in order to target cancerous cells. Topical chemotherapy may be beneficial for patients who are unable to undergo surgery or prefer a non-invasive treatment option. However, it is typically reserved for smaller, well-defined tumors.
Photodynamic Therapy
Photodynamic therapy (PDT) is a novel treatment approach that involves applying a photosensitizing agent to the tumor and then exposing it to a specific wavelength of light. This process activates the agent, which generates reactive oxygen species that selectively kill cancer cells. PDT is a minimally invasive treatment option for superficial SCC or as a supplement to other treatments. It preserves healthy tissue and has a positive cosmetic outcome.
Innovative Approaches to Treating Squamous Cell Carcinoma of the Eyelid
Recent advances in medical research and technology have resulted in the development of novel approaches to managing and treating squamous cell carcinoma of the eyelid. These cutting-edge innovations aim to increase treatment efficacy, lower recurrence rates, and improve cosmetic and functional outcomes. Here are some of the most promising advancements in the treatment of eyelid SCC:
Immunotherapy
Immunotherapy is a revolutionary approach to cancer treatment that uses the body’s immune system to recognize and destroy cancer cells. Immune checkpoint inhibitors such as pembrolizumab and nivolumab have shown promise in advanced or metastatic cases of eyelid SCC. These agents target specific proteins on cancer cells to prevent them from evading the immune system. Clinical trials are currently underway to assess the efficacy and safety of immunotherapy for eyelid SCC, with preliminary findings indicating that it may help control tumor growth and improve patient survival.
Targeted Therapy
Targeted therapy is the use of drugs that target specific molecular pathways involved in cancer growth and progression. Agents that target the epidermal growth factor receptor (EGFR) pathway, such as cetuximab and erlotinib, have been studied in SCC. These therapies inhibit signals that promote cancer cell proliferation and survival. While still in the experimental stage for eyelid SCC, targeted therapy shows promise as a supplement to traditional treatments, especially for patients with advanced or refractory disease.
Gene and Molecular Profiling
Advances in genetic and molecular profiling have enabled a better understanding of the specific mutations and alterations that cause SCC of the eyelid. Researchers can identify potential targets for personalized treatment by examining the tumor’s genetic makeup. For example, next-generation sequencing (NGS) can identify actionable mutations that may be responsive to specific targeted therapies or immunotherapies. This personalized approach ensures that patients receive the most effective treatments based on the unique characteristics of their tumor, potentially improving outcomes while reducing unnecessary side effects.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning (ML) are increasingly being used in oncology, providing new tools for diagnosing and treating SCC of the eyelid. AI algorithms can use large datasets of clinical and imaging data to identify patterns and predict disease progression. Machine learning models can help with treatment planning by evaluating variables such as tumor size, location, and patient characteristics to recommend the best treatment strategies. These technologies have the potential to improve diagnostic accuracy, treatment planning efficiencies, and patient outcomes.
Nanotechnology
Nanotechnology provides innovative solutions for the treatment of eyelid SCC by developing nano-sized drug delivery systems. These systems can encapsulate therapeutic agents, protecting them from degradation and allowing for targeted delivery to the tumor site. Nanoparticles can be engineered to release drugs in a controlled manner, increasing efficacy while reducing systemic side effects. Researchers are working to develop nanotechnology-based treatments for eyelid SCC in order to improve drug delivery and therapeutic outcomes.
Combination Therapies
Combination therapies, which use multiple treatment modalities at the same time, are being researched for their potential to improve outcomes in patients with SCC of the eyelid. For example, combining immunotherapy with radiation therapy or targeted therapy may provide synergistic benefits by addressing different aspects of tumor growth and resistance. Research is ongoing to identify the most effective combinations, as well as the best timing and sequence of treatments.
Photodynamic Therapy Enhancements
Photodynamic therapy (PDT) is being improved to increase its efficacy and expand its applications for eyelid SCC. Novel photosensitizers, improved light delivery systems, and combinations with other treatments are all under consideration. For example, combining PDT with immune checkpoint inhibitors may improve the immune response to cancer cells, resulting in a more comprehensive treatment strategy. These enhancements seek to maximize PDT’s therapeutic benefits while minimizing side effects.
Genetic Editing Technologies
Gene editing technologies, such as CRISPR-Cas9, open up new possibilities for treating eyelid SCC by targeting and modifying specific genes involved in cancer development. This method has the potential to correct genetic mutations, block oncogenes, and activate tumor suppressor genes. While still in its early stages of development, gene editing shows promise for developing personalized treatments that can effectively target the genetic drivers of SCC and prevent tumor progression.
3D Printing and Bioprinting
3D printing and bioprinting technologies are being investigated for their potential to revolutionize reconstructive surgery for patients with SCC of the eyelid. These technologies allow for the creation of customized implants and tissue scaffolds that precisely match the patient’s anatomy. For example, 3D-printed implants can be used to reconstruct the eyelid following tumor removal, resulting in optimal functional and cosmetic outcomes. Bioprinting, which involves printing living cells and tissues, has the potential to produce bioengineered skin grafts for reconstructive use.






