Traumatic endophthalmitis is a serious and vision-threatening ocular condition caused by the introduction of infectious agents into the eye after a penetrating injury. This condition is characterized by inflammation of the intraocular tissues, particularly the vitreous and aqueous humors. The etiological agents are typically bacteria or fungi that enter through a trauma-induced open wound. The sudden onset of symptoms, such as severe pain, decreased vision, redness, and swelling of the eye, necessitates immediate medical attention to avoid permanent vision loss or even loss of the eye.
The pathogenesis of traumatic endophthalmitis involves the invasion of microorganisms into the intraocular environment, where they multiply and cause a strong inflammatory reaction. This inflammation can destroy ocular structures, causing significant morbidity. The type and severity of the injury, the presence of foreign bodies, delayed medical treatment, and inadequate wound management all increase the risk of developing traumatic endophthalmitis. Prompt diagnosis and treatment are critical for improving visual outcomes and maintaining the integrity of the eye.
The clinical presentation, patient history, and diagnostic tests such as vitreous and aqueous taps for microbiological cultures and sensitivities all contribute to the diagnosis of traumatic endophthalmitis. Imaging studies, such as ultrasound and optical coherence tomography (OCT), can help determine the extent of intraocular involvement. Understanding the complex interaction of infectious agents and the host immune response is critical for developing effective treatment strategies and improving prognosis in patients with traumatic endophthalmitis.
Cutting-Edge Innovations in Traumatic Endophthalmitis Treatment
Traumatic endophthalmitis requires a multifaceted approach that includes surgery, antimicrobial therapy, and supportive care. The primary goals are to eliminate the infection, reduce inflammation, and maintain visual function. Standard treatments for traumatic endophthalmitis include the following:
Surgical Intervention
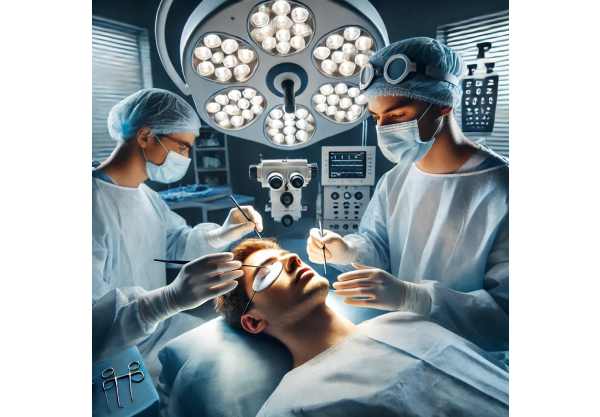
Surgical intervention is frequently required to treat traumatic endophthalmitis, especially in cases with significant intraocular involvement. The main surgical procedures are:
- Pars Plana Vitrectomy (PPV): This procedure removes the vitreous humor and replaces it with a balanced salt solution or other suitable vitreous substitutes. PPV helps to remove infectious agents, inflammatory cells, and debris from the eye. It also enables the delivery of intravitreal antibiotics directly to the site of infection. Early vitrectomy is associated with improved visual results and fewer complications.
- Primary Wound Repair: Immediate surgical repair of the penetrating injury is required to prevent further contamination and promote healing. This includes carefully closing the wound, removing any remaining foreign bodies, and stabilizing the ocular structures.
Antimicrobial Therapy
Antimicrobial therapy is a key component of traumatic endophthalmitis treatment. The suspected or identified causative organisms, as well as their antimicrobial sensitivities, guide antibiotic or antifungal selection. Key features of antimicrobial therapy include:
- Intravitreal Injections: Antibiotics, such as vancomycin and ceftazidime, are commonly used to achieve high intraocular concentrations and effectively eliminate infection. The gram stain and culture results from vitreous samples determine the agents used.
- Systemic Antibiotics: Systemic antibiotics, either orally or intravenously, are frequently used in conjunction with intravitreal therapy to ensure adequate coverage and prevent infection from spreading throughout the body. Broad-spectrum antibiotics such as fluoroquinolones and third-generation cephalosporins are popular treatments.
- Topical and Periocular Antibiotics: Topical antibiotic drops and periocular injections can supplement intravitreal and systemic therapy by maintaining high local antibiotic concentrations and controlling surface infections.
Anti-inflammatory Therapies
Controlling inflammation is critical for reducing tissue damage and improving visual outcomes. Anti-inflammatory therapy usually includes:
- Corticosteroids: Corticosteroids, both systemic and intravitreal, can be used to treat intraocular inflammation. However, their use must be carefully balanced against the risk of exacerbating the infection, and they are usually given after adequate antimicrobial therapy has begun.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs) Topical NSAIDs can be used to treat pain and inflammation on the ocular surface, and they are frequently combined with other anti-inflammatory medications.
Supportive Care
Supportive care is essential in the overall management of traumatic endophthalmitis. This includes:
- Pain Management: Adequate pain relief is required for patient comfort, which may include the use of systemic analgesics and topical anesthetics.
- Closed Monitoring: Regular follow-up visits are essential for monitoring treatment response, adjusting therapy as needed, and detecting complications early on. This frequently requires multiple ocular examinations and imaging studies.
Groundbreaking Approaches to Traumatic Endophthalmitis
Recent advances in the treatment of traumatic endophthalmitis have significantly improved patient outcomes by providing more precise, effective, and minimally invasive options. These innovations cover a wide range of topics, including diagnostic tools, antimicrobial delivery systems, and new therapeutic approaches.
Advanced Diagnostic Techniques
Accurate and timely diagnosis is essential for successful treatment of traumatic endophthalmitis. Innovations in diagnostic techniques have improved the ability to detect and characterize infections quickly and accurately:
- PCR and NGS: These molecular techniques enable the rapid identification of pathogens from vitreous and aqueous samples, providing accurate results even when traditional cultures fail. PCR detects specific bacterial or fungal DNA, whereas NGS analyzes all microbial DNA in the sample. These methods significantly shorten the time to diagnosis and enable targeted antimicrobial treatment.
- Optical Coherence Tomography (OCT) and Ultrasound Biomicroscopy: Advanced imaging modalities such as OCT and ultrasound biomicroscopy allow for detailed visualization of intraocular structures, assisting in determining the extent of infection and guiding surgical planning. OCT can detect subtle changes in the retinal layers, whereas ultrasound biomicroscopy produces high-resolution images of the anterior segment.
Innovations in Antimicrobial Delivery
The effective delivery of antimicrobial agents to the site of infection is critical for the successful treatment of traumatic endophthalmitis. Recent advances in drug delivery systems have increased the efficacy and safety of antimicrobial therapy:
- Nanoparticle Delivery Systems: Nanotechnology has enabled the creation of nanoparticle-based delivery systems capable of encapsulating antibiotics and delivering them directly to the site of infection. These nanoparticles can penetrate ocular tissues more effectively, allowing for longer-term drug release and reducing the need for frequent administration. This targeted approach maximizes therapeutic efficacy while reducing systemic side effects.
- Drug-Eluting Implants: Drug-eluting implants are intraocular devices that release antibiotics over time. These implants ensure consistent and prolonged drug delivery, preserving therapeutic levels within the eye and reducing the need for subsequent injections. Biodegradable implants, which gradually dissolve and release the encapsulated drug, and non-biodegradable implants, which can be removed after treatment is completed, are two examples.
- Intraocular Lenses (IOLs) with Antimicrobial Coatings: For patients who need cataract surgery after traumatic endophthalmitis, IOLs with antimicrobial coatings are an innovative solution. These lenses are coated with antibiotics or antifungal agents that are gradually released into the eye, reducing infection recurrence and improving postoperative outcomes.
Novel Therapeutic Approaches
Beyond traditional antimicrobial therapy, novel therapeutic approaches are being investigated to improve the treatment of traumatic endophthalmitis.
- Phage Therapy: Bacteriophage therapy uses viruses to specifically target and kill bacteria. Phages can be engineered to target bacteria that are resistant to antibiotics, providing a potential solution to the growing antimicrobial resistance problem. Intraocular bacteriophage injection has shown promise in preclinical studies, and ongoing research aims to bring this approach into clinical use.
- Gene Editing Technologies: CRISPR-Cas9 and other gene editing technologies are under investigation for their ability to directly target and disrupt pathogen genetic material. These technologies, which selectively edit the genes responsible for virulence or antibiotic resistance, could provide a new way to combat infections that are difficult to treat with conventional antibiotics.
- Stem Cell Therapy: Researchers are looking into stem cell therapy as a way to repair and regenerate damaged ocular tissues after traumatic endophthalmitis. Stem cells can differentiate into different types of ocular cells, which promotes healing and restores function. While still in the experimental stage, this approach shows promise for improving visual outcomes and lowering complications in patients with severe ocular trauma.
Artificial Intelligence, Machine Learning
AI and machine learning are transforming the diagnosis and treatment of traumatic endophthalmitis.
- Predictive Analytics: Artificial intelligence algorithms can use large datasets of clinical and imaging data to predict the risk of endophthalmitis after ocular trauma. These predictive models can inform early intervention strategies, thereby preventing infection and improving outcomes.
- Automated Diagnosis: Machine learning algorithms can accurately detect early signs of endophthalmitis using imaging data such as OCT and ultrasound images. Automated diagnostic systems can assist clinicians in making timely and accurate diagnoses, allowing for faster treatment.
- Personalized Treatment Plans: AI-powered platforms can use patient-specific data, such as genetic information, to create personalized treatment plans. This personalized approach can optimize antimicrobial selection, dosing, and treatment duration, increasing therapy efficacy while minimizing side effects.






