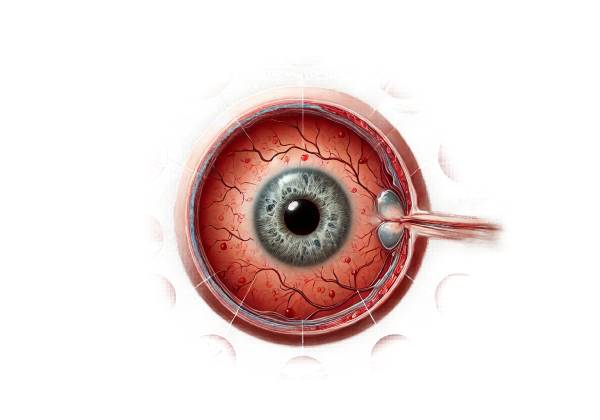
Retinopathy of Prematurity (ROP) is a potentially blinding eye disorder that primarily affects premature infants, particularly those born before 31 weeks of gestation and with a birth weight of less than 2.75 pounds (1250 grams). ROP is a disease of the retina, the light-sensitive layer of tissue at the back of the eye that is responsible for capturing visual information and sending it to the brain via the optic nerve. This condition is characterized by abnormal development of retinal blood vessels, which can lead to retinal detachment and, ultimately, blindness if not promptly diagnosed and treated.
Pathophysiology of Retinopathy of Prematurity
The development of the retina and its blood vessels begins early in fetal life and continues until full-term birth. In a normal pregnancy, the retinal blood vessels begin to grow at around 16 weeks of gestation and complete their development by 36 weeks. These blood vessels start at the optic nerve and gradually spread toward the edges of the retina, providing oxygen and nutrients necessary for the retina’s growth and function.
In premature infants, this process is disrupted because the retina has not fully developed at the time of birth. The incompletely vascularized retina in premature infants is exposed to an environment different from the womb, where it would have continued to mature under carefully controlled conditions. The exposure to higher levels of oxygen in neonatal intensive care units (NICUs) and other factors can lead to abnormal growth of retinal blood vessels. This abnormal vascularization is the hallmark of ROP.
The pathogenesis of ROP is typically divided into two phases:
- Phase 1: Vascular Arrest and Regression: In the first phase, the premature birth interrupts the normal process of retinal vascularization. The abrupt change from the intrauterine to the extrauterine environment, particularly exposure to supplemental oxygen, can cause the blood vessels in the retina to stop growing and even regress. The absence of sufficient vascularization leaves the peripheral retina without adequate oxygen supply, which in turn triggers a cascade of events leading to the second phase.
- Phase 2: Pathological Neovascularization: As the retina becomes increasingly hypoxic (low in oxygen), it releases vascular endothelial growth factor (VEGF), a protein that stimulates the growth of new blood vessels. However, these newly formed blood vessels are often abnormal, fragile, and prone to leakage and bleeding. This abnormal neovascularization can lead to fibrosis and scarring, which may pull on the retina and cause it to detach from the underlying layers, a serious complication that can result in permanent vision loss.
Classification and Staging of Retinopathy of Prematurity
ROP is classified based on the severity of the disease, the location of the abnormal blood vessel growth, and the extent of the retinal involvement. The International Classification of Retinopathy of Prematurity (ICROP) system is commonly used by ophthalmologists to categorize the disease into five stages:
- Stage 1: Mildly Abnormal Blood Vessel Growth: In this stage, there is a thin line of demarcation between the normal and avascular (non-vascularized) retina. The blood vessel growth is slightly abnormal but not severe enough to require treatment. Most infants with Stage 1 ROP will experience spontaneous regression of the disease without the need for intervention.
- Stage 2: Moderately Abnormal Blood Vessel Growth: In Stage 2, the demarcation line has evolved into a ridge, with the abnormal blood vessels beginning to invade the peripheral retina. Although the condition is more pronounced than in Stage 1, many cases still regress without treatment. However, close monitoring is essential to detect any progression to more severe stages.
- Stage 3: Severely Abnormal Blood Vessel Growth (Plus Disease): Stage 3 is characterized by extraretinal fibrovascular proliferation, where the abnormal blood vessels begin to extend into the vitreous, the gel-like substance filling the eye. This stage is further divided into “Plus Disease” and “No Plus Disease.” Plus Disease refers to the presence of additional signs of severity, such as increased dilation and tortuosity of the blood vessels in the posterior retina, as well as iris neovascularization. Stage 3 with Plus Disease is a critical point where treatment may be necessary to prevent retinal detachment and preserve vision.
- Stage 4: Partial Retinal Detachment: In Stage 4, the fibrovascular tissue begins to pull the retina away from its underlying layers, leading to partial retinal detachment. This stage is subdivided into 4A (macula is attached) and 4B (macula is detached). The macula is the central part of the retina responsible for sharp, detailed vision. Stage 4 is a serious condition that often requires surgical intervention to prevent further detachment and vision loss.
- Stage 5: Total Retinal Detachment: Stage 5 represents the most advanced form of ROP, where the retina is completely detached from the back of the eye. This stage is associated with a very poor visual prognosis, and even with surgical intervention, restoring vision is often not possible.
In addition to staging, ROP is also classified based on the location of the disease within the retina, which is divided into three zones:
- Zone I: This is the innermost zone, centered on the optic nerve. It includes the macula and is the most critical area for vision. ROP in Zone I is considered more severe and is associated with a higher risk of progression to advanced stages.
- Zone II: This zone extends from the edge of Zone I to the ora serrata (the anterior edge of the retina). ROP in Zone II is less severe than in Zone I but still requires close monitoring.
- Zone III: The outermost zone, located at the peripheral edge of the retina. ROP in Zone III is usually milder and has a higher likelihood of spontaneous regression.
The extent of the retinal involvement is also categorized into clock hours, with the retina divided into 12 clock hours. The more clock hours involved, the more extensive the disease.
Risk Factors for Retinopathy of Prematurity
Several risk factors contribute to the development of ROP in premature infants. The most significant risk factors include:
- Gestational Age and Birth Weight: The most critical risk factors for ROP are gestational age and birth weight. The lower the gestational age and birth weight, the higher the risk of developing ROP. Infants born before 28 weeks of gestation or weighing less than 2.2 pounds (1000 grams) are at the highest risk.
- Oxygen Therapy: While oxygen is essential for the survival of premature infants, especially those with respiratory distress, excessive or uncontrolled oxygen therapy can increase the risk of ROP. The relationship between oxygen levels and ROP is complex, and careful monitoring of oxygen saturation levels is necessary to minimize the risk.
- Respiratory Distress Syndrome (RDS): Premature infants with RDS often require mechanical ventilation and supplemental oxygen, both of which are associated with an increased risk of ROP.
- Sepsis and Infections: Infections, particularly sepsis, can exacerbate the risk of ROP by triggering inflammatory responses that may contribute to abnormal blood vessel growth in the retina.
- Blood Transfusions: The need for blood transfusions in premature infants has been associated with an increased risk of ROP, although the exact mechanism is not fully understood.
- Apnea and Bradycardia: Episodes of apnea (temporary cessation of breathing) and bradycardia (slow heart rate) are common in premature infants and have been linked to an increased risk of ROP.
Epidemiology of Retinopathy of Prematurity
ROP is a leading cause of childhood blindness worldwide, particularly in countries with advanced neonatal care that allows for the survival of very premature infants. The incidence of ROP varies widely depending on the level of neonatal care and the population studied. In high-income countries, where neonatal care is well-developed, ROP is more common due to the increased survival of extremely premature infants. In these settings, the incidence of ROP can be as high as 50-70% among infants born before 28 weeks of gestation.
In middle- and low-income countries, the incidence of ROP is also rising due to improvements in neonatal care. However, the lack of standardized screening and treatment protocols in these regions can lead to higher rates of severe ROP and blindness. The World Health Organization (WHO) and other global health organizations have recognized the need for improved screening and treatment programs in these settings to reduce the burden of ROP-related blindness.
ROP remains a significant public health concern, and efforts to prevent, screen, and treat this condition are crucial to reducing the incidence of blindness among premature infants. Understanding the risk factors, pathophysiology, and epidemiology of ROP is essential for healthcare providers and researchers working to improve outcomes for these vulnerable patients.
Diagnostic Methods
The diagnosis of Retinopathy of Prematurity (ROP) involves a series of examinations and imaging techniques designed to identify and monitor the progression of the disease. Early and accurate diagnosis is critical for initiating timely treatment and preventing the severe complications of ROP, including retinal detachment and blindness.
Ophthalmologic Screening
Ophthalmologic screening is the cornerstone of ROP diagnosis. Premature infants at risk for ROP should undergo regular eye examinations starting shortly after birth. The American Academy of Pediatrics (AAP), the American Academy of Ophthalmology (AAO), and the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) have established guidelines for the timing and frequency of these screenings based on the infant’s gestational age and birth weight.
- Indirect Ophthalmoscopy: This is the standard method for diagnosing ROP. During the examination, an ophthalmologist uses an indirect ophthalmoscope, a light source, and a handheld lens to visualize the retina. The examination is performed after dilating the infant’s pupils with eye drops to allow a clear view of the retina. Indirect ophthalmoscopy enables the ophthalmologist to assess the entire retina, including the peripheral areas where ROP typically begins. The examination focuses on identifying the stage, zone, and extent of retinal involvement, as well as the presence of Plus Disease, which indicates more severe disease and a higher risk of progression.
Retinal Imaging
In addition to traditional ophthalmoscopic examinations, retinal imaging techniques are increasingly used to document and monitor the progression of ROP. These imaging techniques provide detailed and objective documentation of retinal findings, which can be useful for remote consultations, follow-up, and research purposes.
- Digital Retinal Photography: Digital retinal cameras, such as the RetCam, are commonly used to capture high-resolution images of the retina. These images can be stored, shared with other specialists, and compared over time to assess changes in the disease’s progression. Retinal photography is particularly valuable in telemedicine settings, where images can be reviewed by experts who may not be physically present with the patient.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique that uses light waves to create cross-sectional images of the retina. Although OCT is more commonly used in adults with retinal diseases, its application in infants with ROP is growing. OCT provides detailed images of the retinal layers, allowing for the detection of subtle abnormalities and early signs of retinal detachment that may not be visible through ophthalmoscopy alone. OCT is especially useful for evaluating the macula and other critical areas of the retina.
Fluorescein Angiography
Fluorescein angiography is a specialized imaging technique that involves injecting a fluorescent dye into the bloodstream and taking photographs of the retina as the dye circulates through its blood vessels. This technique is useful for identifying abnormal blood vessel growth, leakage, and areas of non-perfusion (lack of blood flow) in the retina. While fluorescein angiography is not routinely performed in all cases of ROP, it can provide valuable information in complex cases, particularly when planning for surgical interventions.
Telemedicine and Remote Screening
Telemedicine has become an important tool in the screening and diagnosis of ROP, especially in regions with limited access to pediatric ophthalmologists. In telemedicine programs, trained personnel at the bedside capture retinal images using digital cameras, which are then transmitted to a remote specialist for interpretation. This approach expands access to expert care and allows for early detection and intervention in areas where in-person examinations may not be feasible.
Genetic Testing
While not a standard part of ROP diagnosis, genetic testing may be considered in certain cases, particularly when there is a suspicion of an underlying genetic predisposition to abnormal retinal development. Genetic testing can identify mutations associated with familial exudative vitreoretinopathy (FEVR) or other conditions that mimic ROP but may require different management strategies. Identifying genetic factors can also provide valuable information for counseling families about the risk of recurrence in future pregnancies.
Retinopathy of Prematurity Management
The management of Retinopathy of Prematurity (ROP) focuses on preventing the progression of the disease to avoid severe complications like retinal detachment and blindness. Treatment decisions are based on the stage, zone, and severity of the disease, with the goal of preserving vision while minimizing the risks associated with treatment.
Laser Photocoagulation
Laser photocoagulation is the most common and effective treatment for ROP, particularly for Stage 3 with Plus Disease. This procedure involves using a laser to create burns in the avascular (non-vascularized) areas of the peripheral retina. The laser burns help to reduce the production of vascular endothelial growth factor (VEGF), which is responsible for the abnormal blood vessel growth seen in ROP. By doing so, laser photocoagulation halts the progression of the disease and reduces the risk of retinal detachment.
Laser treatment is typically performed in an operating room under general anesthesia to ensure the infant remains still and comfortable during the procedure. The treatment is often done in a single session but may require multiple sessions depending on the extent of the disease. While laser photocoagulation is highly effective, it does cause some loss of peripheral vision due to the destruction of retinal tissue. However, this is a necessary trade-off to preserve central vision and prevent blindness.
Anti-VEGF Therapy
Anti-VEGF therapy has emerged as a promising treatment option for ROP, particularly in cases involving Zone I disease or when laser photocoagulation is not feasible. Anti-VEGF drugs, such as bevacizumab (Avastin), work by inhibiting the action of VEGF, thereby reducing abnormal blood vessel growth. The drug is administered as an intravitreal injection (directly into the eye) under sterile conditions.
The use of anti-VEGF therapy has several advantages, including the ability to treat more extensive areas of the retina without causing the same degree of peripheral vision loss as laser treatment. Additionally, anti-VEGF therapy can be used in eyes with significant hemorrhage or media opacity that would make laser treatment difficult. However, the long-term effects of anti-VEGF therapy in premature infants are still being studied, and there is some concern about potential systemic side effects, given that VEGF plays a role in normal development.
Anti-VEGF therapy is often used in conjunction with laser photocoagulation, particularly in severe cases where a combined approach may provide the best outcomes. Follow-up is critical after anti-VEGF treatment to monitor for recurrence of disease, which can occur weeks to months after the initial injection.
Surgical Interventions
In advanced stages of ROP (Stages 4 and 5), where retinal detachment has occurred or is imminent, surgical intervention may be necessary to preserve or restore vision. The two primary surgical options are:
- Scleral Buckling: This procedure involves placing a silicone band (buckle) around the outside of the eye to indent the wall of the eye inward, relieving the traction on the retina caused by the fibrous tissue. Scleral buckling is most effective in cases of Stage 4A ROP, where the macula is still attached. This procedure can prevent further retinal detachment and may allow the retina to reattach in some cases.
- Vitrectomy: Vitrectomy is a more complex surgical procedure used in Stage 4B and Stage 5 ROP, where the retina is either partially or completely detached. The surgery involves removing the vitreous gel and the fibrous tissue pulling on the retina, allowing the retina to flatten back into place. While vitrectomy can be successful in reattaching the retina, the visual outcomes are often poor in advanced cases due to irreversible damage to the retina.
Follow-Up and Long-Term Care
Follow-up care is crucial for all infants treated for ROP, as the disease can recur or progress even after initial treatment. Infants require regular ophthalmologic examinations to monitor the retina’s status and to detect any signs of new or worsening disease. In cases where ROP has been treated successfully, long-term follow-up is still necessary to monitor for complications such as myopia (nearsightedness), strabismus (misalignment of the eyes), amblyopia (lazy eye), and late-onset retinal detachment.
In addition to regular eye examinations, infants who have undergone treatment for ROP may require visual rehabilitation services, including corrective lenses, patching therapy, or other interventions to optimize visual outcomes. Early intervention and ongoing monitoring are key to ensuring the best possible visual development in these children.
Trusted Resources and Support
Books
- “Retinopathy of Prematurity: A Guide to Understanding and Management” by Frank R. Martin and Michael F. Chiang: This comprehensive book provides detailed information on the diagnosis, management, and outcomes of ROP, making it a valuable resource for both healthcare providers and families.
- “Understanding Retinopathy of Prematurity” by American Academy of Ophthalmology: This guide offers a clear and concise overview of ROP, including its causes, risk factors, and treatment options.
Organizations
- The American Academy of Pediatrics (AAP): A leading organization providing guidelines, research, and resources on the care and management of premature infants, including ROP.
- The National Eye Institute (NEI): A government organization offering extensive resources on eye diseases, including ROP, with information for both healthcare professionals and the public.
- ROPARD Foundation: A non-profit organization dedicated to supporting research and providing information on ROP and associated retinal diseases.










