Sjögren’s syndrome is a chronic autoimmune disease characterized by lymphocytic infiltration and destruction of exocrine glands, particularly the salivary and lacrimal glands, which causes dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca). Although Sjögren’s syndrome can affect multiple organs, ocular manifestations are among the most common and debilitating aspects of the disease, with a significant impact on a patient’s quality of life.
Understanding the Fundamentals of Sjögren’s Syndrome
Sjögren’s syndrome can be a primary condition (primary Sjögren’s syndrome) or a complication of another autoimmune disease (e.g., rheumatoid arthritis, systemic lupus erythematosus). Chronic inflammation of the lacrimal and salivary glands is the syndrome’s defining feature, caused by an abnormal immune response in which the body’s immune system incorrectly targets its own tissues.
The disease primarily affects women, with a female-to-male ratio of about 9:1, and it usually appears in middle-aged adults, but it can occur at any age. Sjögren’s syndrome affects approximately 0.1% to 0.6% of the population, making it one of the most common autoimmune disorders.
Pathophysiology Of Ocular Manifestations
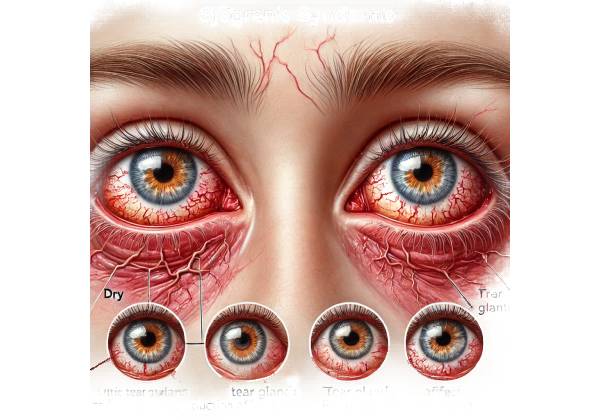
Sjögren’s syndrome ocular manifestations, particularly keratoconjunctivitis sicca (KCS), are the direct result of autoimmune-mediated lacrimal gland destruction. The lacrimal glands produce the aqueous component of the tear film, which is necessary for ocular surface health, comfort, and clear vision.
In Sjögren’s syndrome, lymphocytes, primarily T-cells, infiltrate the lacrimal glands, causing glandular dysfunction and decreased tear production. This reduction in tear secretion causes aqueous-deficient dry eye, the disease’s most visible ocular feature.
Tear Film and its Importance
To understand the impact of Sjögren’s syndrome on the eyes, one must first understand the role of the tear film. The tear film is a complex, multi-layered structure that covers the ocular surface and serves several important functions:
- Lubrication: The tear film lubricates the eye’s surface, allowing the eyelids to move smoothly and comfortably while blinking.
- Protection: The tear film contains antimicrobial proteins and enzymes that help the eye fight infections and remove debris.
- Nutrient Supply: The tear film supplies essential nutrients to the avascular cornea, including oxygen, ensuring its transparency and health.
- Optical Clarity: A stable tear film is critical for keeping a smooth ocular surface, which is required for clear vision. Any disruption in the tear film can cause visual disturbances like blurring and glare.
The tear film consists of three layers:
- Lipid Layer: The meibomian glands produce the outermost layer, which protects the underlying aqueous layer from evaporation.
- Aqueous Layer: The lacrimal glands produce the middle layer, which provides moisture as well as proteins, enzymes, and electrolytes.
- Mucin Layer: The conjunctiva’s goblet cells produce the innermost layer, which helps anchor the aqueous layer to the ocular surface and ensures even distribution of the tear film.
Ocular Signs of Sjögren’s Syndrome
Sjögren’s syndrome ocular manifestations are primarily caused by reduced production of the aqueous component of the tear film, which results in aqueous-deficient dry eye. However, the disease can also affect other aspects of the tear film and the ocular surface, resulting in a variety of symptoms and complications.
Keratoconjunctivitis Sicca (Dry Eye Disease)
Keratoconjunctivitis sicca (KCS), or dry eye disease, is the most common ocular manifestation of Sjögren’s syndrome. Chronic dryness of the eyes caused by a lack of tear production is its defining characteristic. A lack of adequate tears causes desiccation of the ocular surface, resulting in discomfort, visual disturbances, and an increased risk of ocular surface injury.
The symptoms of KCS include:
- Dryness and Grittiness: Patients frequently report a sensation of dryness, burning, or grittiness in their eyes, as if something is stuck in them.
- Redness and Irritation: Chronic dryness and inflammation can cause redness and irritation in the conjunctiva, which is the clear tissue that covers the white part of the eye.
- Blurred Vision: The unstable tear film can cause fluctuating vision, with patients frequently reporting intermittent blurring that improves after blinking.
- Photophobia: Patients with KCS frequently experience photophobia, which occurs when the damaged ocular surface becomes more sensitive to light exposure.
- Increased Tear Production: Interestingly, some patients with Sjögren’s syndrome may experience reflex tearing, in which the eyes produce excessive tears in response to dryness and irritation. However, these tears are usually of poor quality and do not sufficiently lubricate the eye.
Complications of Keratoconjunctivitis Sicca
If left untreated, keratoconjunctivitis sicca can cause a number of complications that jeopardize ocular health and vision.
- Corneal Erosions: Prolonged dryness can cause micro-abrasions or erosions on the corneal surface, resulting in pain, light sensitivity, and an increased risk of infection.
- Corneal Ulcers: Severe cases of dry eye can lead to corneal ulcers, which are erosions of the cornea’s deeper layers. Corneal ulcers are a serious condition that can cause scarring and permanent vision loss if not treated promptly.
- Infectious Keratitis: Sjögren’s syndrome’s impaired tear film and disrupted ocular surface raise the risk of infectious keratitis, a bacterial or fungal infection of the cornea. This condition requires immediate medical attention to avoid permanent eye damage.
- Filamentary Keratitis: Filamentary keratitis is a condition in which strands of mucus and dead epithelial cells adhere to the corneal surface. These filaments cause significant discomfort and can worsen dry eye symptoms.
- Conjunctival Scarring: Chronic inflammation of the conjunctiva can cause scarring and shrinkage of the conjunctival tissue, which reduces tear production and worsens dry eye symptoms.
Meibomian Gland Dysfunction
In addition to the lacrimal glands, Sjögren’s syndrome can affect the meibomian glands, which produce the lipid layer of the tear film. Meibomian gland dysfunction (MGD) is a common comorbidity in Sjögren’s syndrome patients, exacerbating dry eye symptoms.
The symptoms of MGD include:
- Foamy or Frothy Tears: In MGD, the tear film’s lipid composition changes, making the tears appear foamy or frothy.
- Lid Margin Inflammation: MGD frequently causes inflammation of the eyelid margins, also known as blepharitis. Patients may experience redness, swelling, and crusting around the eyelid edges.
- Evaporative Dry Eye: The deficient lipid layer in MGD causes increased evaporation of the aqueous layer, resulting in evaporative dry eye. This worsens the symptoms of dry eye disease and destabilizes the tear film.
Other Ocular Manifestations
Sjögren’s syndrome can affect other parts of the eye, but the most common ocular manifestations are keratoconjunctivitis sicca and meibomian gland dysfunction.
- Episcleritis: Episcleritis is an inflammatory condition that affects the episclera, which is the thin layer of tissue that connects the sclera (the white of the eye) to the conjunctiva. It causes redness and mild discomfort, and while it is generally harmless, it can be persistent and bothersome.
- Scleritis: Scleritis is a severe form of inflammation affecting the sclera. It causes severe pain, redness, and tenderness and, if left untreated, can lead to sclera thinning (scleromalacia) and vision loss.
- Uveitis: This is an inflammation of the uveal tract, which includes the iris, ciliary body, and choroid. Although uncommon, uveitis can occur in patients with Sjögren’s syndrome and cause eye pain, redness, photophobia, and blurred vision. Chronic uveitis can cause cataract formation, glaucoma, and macular edema, all of which can severely impair vision.
Effects on Quality of Life
The ocular manifestations of Sjögren’s syndrome can significantly affect a patient’s quality of life. Dry eye disease and other ocular conditions can cause chronic discomfort, visual disturbances, and complications, making daily activities like reading, driving, and working difficult. Furthermore, the psychological burden of living with a chronic, incurable disease can cause anxiety and depression, reducing overall well-being.
Diagnostic methods
Diagnosing the ocular manifestations of Sjögren’s syndrome necessitates a thorough evaluation by an eye care professional, which includes a detailed patient history, clinical examination, and a battery of specialized tests to determine the severity of dry eye disease and other ocular complications. Early and accurate diagnosis is critical for successfully managing symptoms and preventing further eye damage.
Clinical Examination
The first step in diagnosing the ocular manifestations of Sjögren’s syndrome is a thorough clinical examination that typically includes:
- Patient History: A thorough patient history is required to identify symptoms consistent with Sjögren’s syndrome, such as chronic dry eyes, dry mouth, and other systemic symptoms. In addition, the history should include questions about other autoimmune conditions, medication use, and any previous eye treatments or surgeries.
- Slit-Lamp Examination: A slit-lamp examination enables the ophthalmologist to closely examine the anterior segment of the eye, which includes the conjunctiva, cornea, tear film, and eyelids. During this examination, the clinician can look for signs of keratoconjunctivitis sicca, such as conjunctival redness, corneal erosions, filaments, and meibomian gland dysfunction, like thickened lid margins or frothy tears.
- Tear Film Break-Up Time (TBUT): This test determines the stability of the tear film. After administering a small amount of fluorescein dye to the eye, the patient is asked to blink, and the time it takes for dry spots to appear on the corneal surface is recorded. A shortened TBUT (less than 10 seconds) indicates an unstable tear film, which is a characteristic of dry eye disease.
- Ocular Surface Staining: Using dyes like fluorescein, rose bengal, or lissamine green can help highlight areas of corneal and conjunctival damage. These stains can reveal punctate epithelial erosions, which are small areas of damage on the cornea’s surface, as well as conjunctival staining, which indicates dry eye damage.
- Schirmer’s Test: Schirmer’s test is a common diagnostic tool for measuring tear production. During the test, a small strip of filter paper is placed inside the lower eyelid, and the amount of moisture absorbed by the paper over a set time (usually 5 minutes) is recorded. Tear production of less than 5 mm of moisture on the paper is considered indicative of severe aqueous tear deficiency, as seen in Sjögren’s Syndrome.
Specialized Diagnostic Tests
In addition to the clinical examination, several specialized diagnostic tests can provide more insight into the severity of the ocular manifestations of Sjögren’s syndrome and help guide management decisions:
- Tear Osmolarity Testing: This test measures the concentration of solutes in the tear film. Tear osmolarity is frequently elevated in patients with dry eye disease, including those with Sjögren’s syndrome, reflecting the increased concentration of salts and other substances caused by reduced tear production and increased evaporation. High tear osmolarity causes inflammation and damage to the ocular surface.
- Meibography: Meibography is an imaging technique for examining the meibomian glands in the eyelids. It provides detailed images of the gland structure, making it easier to detect gland dropout, atrophy, and other abnormalities associated with meibomian gland dysfunction. Meibography is especially useful for determining the role of evaporative dry eye in the overall disease burden in Sjögren’s syndrome.
- Confocal Microscopy: In vivo confocal microscopy is a non-invasive imaging technique that enables microscopic visualization of corneal and conjunctival cells. This test can detect signs of inflammation, nerve damage, and changes in the density of goblet cells (which produce mucin) in the conjunctiva, all of which are important for diagnosing and monitoring Sjögren’s syndrome.
- Autoantibody Testing: Although not an ocular test, autoantibody testing is an important part of the diagnostic process for Sjögren’s syndrome. Blood tests for specific autoantibodies, such as anti-Ro (SSA) and anti-La (SSB), can aid in the diagnosis of Sjögren’s syndrome. Elevated levels of these autoantibodies are common in patients with the disease and help to confirm the diagnosis when combined with ocular and systemic symptoms.
- Impression Cytology: Impression cytology is the process of collecting a small number of cells from the conjunctival surface using filter paper or a similar device. The sample is then examined under a microscope to determine the condition of the ocular surface. This test can detect a decrease in goblet cell density and other cellular changes associated with dry eye disease in Sjögren’s syndrome.
- Lip Biopsy: A minor salivary gland biopsy, typically performed on the lower lip, can provide histological confirmation of Sjögren’s syndrome. The biopsy looks for lymphocytic infiltration and glandular destruction, which are common in Sjögren’s syndrome. Although this test is most commonly used to diagnose systemic Sjögren’s syndrome, it may also be useful in cases with prominent ocular manifestations.
Imaging Techniques
Advanced imaging techniques are becoming increasingly important in diagnosing and monitoring the ocular manifestations of Sjögren’s Syndrome. These imaging modalities offer detailed views of the ocular surface and tear-producing glands, allowing for a more precise assessment of disease severity.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT is a non-invasive imaging technique that generates high-resolution cross-sectional images of the anterior segment of the eye. It can measure the thickness of the tear meniscus (the thin layer of tears that runs along the lower eyelid), detect structural changes in the cornea and conjunctiva, and examine the lacrimal and meibomian glands.
- Tear Meniscus Measurement: Using AS-OCT or other imaging modalities, the height of the tear meniscus can be measured to estimate tear volume. Patients with aqueous-deficient dry eye, such as those suffering from Sjögren’s syndrome, frequently have a shorter tear meniscus.
- Lacrimal Gland Imaging: Ultrasonography, magnetic resonance imaging (MRI), and computed tomography (CT) can all be used to examine the lacrimal glands in Sjögren’s syndrome. These imaging techniques can detect enlargement, atrophy, and other structural changes in the lacrimal glands that may be associated with the disease.
Sjögren’s Syndrome Ocular Manifestations Management
The goal of managing Sjögren’s syndrome’s ocular manifestations is to alleviate symptoms, protect the ocular surface, and avoid complications. Since there is no cure for Sjögren’s syndrome, treatment focuses on symptom management and improving the patient’s quality of life. A multidisciplinary approach, frequently involving both ophthalmologists and rheumatologists, is required for comprehensive treatment.
Artificial tears and lubricants
Artificial tears and lubricants are essential for treating keratoconjunctivitis sicca (dry eye disease) in Sjögren’s syndrome. These products supplement the deficient tear film by providing moisture and relief from dryness.
- Preservative-Free Artificial Tears: Patients are frequently advised to use preservative-free artificial tears because preservatives in eye drops can aggravate ocular surface irritation, especially with repeated use. These drops can be applied several times per day, depending on the severity of the symptoms.
- Lubricating Ointments and Gels: Lubricating ointments or gels may be prescribed for severe cases of dry eye, particularly at night. These thicker formulations provide longer-lasting moisture but can temporarily blur vision, so they are typically applied before bedtime.
- Lipid-Based Eye Drops: Lipid-based artificial tears are especially beneficial for patients with concurrent meibomian gland dysfunction (MGD) because they help restore the lipid layer of the tear film, thereby reducing tear evaporation.
Anti-inflammatory Treatments
Inflammation is a major factor in the development of dry eye disease in Sjögren’s syndrome. As a result, anti-inflammatory therapies are frequently required to control the underlying inflammation and increase tear production.
- Topical Cyclosporine A (Restasis): Cyclosporine A is an immunomodulatory agent that decreases ocular surface inflammation while increasing tear production. It is frequently prescribed for moderate to severe dry eye disease and is taken twice daily. Patients may have to use it for several months before seeing significant results.
- Lifitegrast (Xiidra): Lifitegrast is another anti-inflammatory eyedrop used to treat dry eye disease. It works by inhibiting the interaction of lymphocyte function-associated antigen 1 (LFA-1) and intercellular adhesion molecule-1 (ICAM-1), which are both involved in the inflammatory process. Lifitegrast can alleviate symptoms of dryness and discomfort.
- Corticosteroid Eye Drops: In cases of severe inflammation or acute flare-ups, short-term use of low-dose corticosteroid eye drops may be recommended. However, long-term steroid use is discouraged due to the risk of side effects such as increased intraocular pressure and cataract formation.
Punctal Occlusion
Punctal occlusion is a technique for increasing tear retention on the ocular surface by blocking the tear drainage ducts (puncta). This can happen either temporarily or permanently.
- Punctal Plugs: Punctal plugs are small devices that are inserted into the tear ducts to block tear drainage and are commonly used to achieve temporary punctal occlusion. These plugs are available in collagen (which dissolves over time) or silicone (which is more permanent but removable). Punctal plugs are particularly useful for patients who do not respond well to artificial tears alone.
- Permanent Punctal Occlusion: When more permanent tear retention is required, the puncta can be permanently closed using thermal or laser cautery. This procedure is usually reserved for patients with severe dry eye who have not responded to other treatments.
Autologous Serum Eye Drops
Autologous serum eye drops are a treatment option for patients with severe dry eye who have not responded to other treatments. These drops are created from the patient’s own blood, which is processed to separate the serum. The serum is high in growth factors, vitamins, and nutrients, which aid in healing and reducing inflammation on the ocular surface. Autologous serum eye drops can be especially beneficial for patients who have corneal erosions or ulcers.
Moisture Chamber Glasses
Moisture chamber glasses or goggles are specialized eyewear that traps moisture around the eyes, reducing evaporation and alleviating dry eye symptoms. These glasses are especially useful in low-humidity environments or when performing activities that exacerbate dryness, such as prolonged screen use or wind exposure.
Nutritional Supplements
Fish oil and flaxseed oil contain omega-3 fatty acids, which have anti-inflammatory properties and may improve tear film quality. Patients with Sjögren’s syndrome are frequently advised to include omega-3 supplements in their diet as part of their overall dry eye disease treatment plan.
Managing Meibomian Gland Dysfunction
Specific treatments for patients with meibomian gland dysfunction (MGD) aim to improve meibomian gland function while decreasing evaporative dry eye.
- Warm Compresses: Applying warm compresses on a regular basis can help soften the meibum (oil) in the meibomian glands, improving gland function and reducing lid margin inflammation.
- Lid Hygiene: Proper lid hygiene is essential for managing MGD-associated blepharitis. This includes gently cleansing the eyelid margins with a mild cleanser or commercially available lid wipes.
- Thermal Pulsation Therapy: In severe cases of MGD, thermal pulsation therapy (such as LipiFlow) may be recommended. This in-office procedure uses heat and gentle pressure to unclog the meibomian glands, which improves the lipid layer of the tear film.
Systematic Treatments
Given that Sjögren’s syndrome is a systemic autoimmune disease, systemic treatments may be required to control the disease process and alleviate ocular symptoms.
- Hydroxychloroquine is an immunomodulatory drug that is commonly used to treat autoimmune diseases such as Sjögren’s syndrome. It has the potential to reduce systemic inflammation while also indirectly improving ocular symptoms.
- Corticosteroids and Immunosuppressants: Systemic corticosteroids or immunosuppressants may be prescribed in cases of severe systemic involvement or when ocular symptoms persist despite other treatments. Rheumatologists typically manage these medications as part of a comprehensive treatment plan.
Patient Education and Lifestyle Modification
Educating patients about the chronic nature of Sjögren’s syndrome and the importance of sticking to their treatment plan is critical for effective management. Lifestyle changes, such as avoiding environmental triggers (e.g., wind, smoke, dry air), using humidifiers, staying hydrated, and taking frequent breaks during eye-strain activities, can all help manage symptoms.
Trusted Resources and Support
Books
- “The Sjögren’s Book” by Daniel J. Wallace: This comprehensive guide provides detailed information about Sjögren’s syndrome, including its ocular manifestations, treatment options, and patient support resources. It is a valuable resource for both patients and healthcare providers.
- “Sjögren’s Syndrome: Diagnosis and Therapeutics” by Alessia Alunno, Andrea Doria, and Nicola Montano: This book offers an in-depth look at the diagnosis, management, and treatment of Sjögren’s syndrome, with a focus on the latest therapeutic advancements. It is particularly useful for healthcare professionals and researchers.
Organizations
- Sjögren’s Foundation: The Sjögren’s Foundation is a leading organization dedicated to providing support, education, and resources for individuals living with Sjögren’s syndrome. Their website offers a wealth of information on the condition, including tips for managing dry eye symptoms and access to patient support groups.
- American Academy of Ophthalmology (AAO): The AAO provides extensive resources on eye health, including detailed information on the ocular manifestations of Sjögren’s syndrome. Their materials are designed for both patients and healthcare professionals, offering up-to-date guidelines and educational content.
- National Eye Institute (NEI): The NEI is a premier source of information on eye diseases and conditions, including Sjögren’s syndrome. Their website offers research updates, clinical trial information, and educational resources to help patients and healthcare providers manage ocular complications associated with the disease.










