Styes, also known as hordeolums, are a common and often painful eyelid condition. It develops when one of the small oil glands near the base of the eyelashes or within the eyelid becomes infected or inflamed, resulting in a red, swollen bump. Styes are generally harmless and resolve on their own, but they can cause significant discomfort and inconvenience to the affected individual.
Types of Styes
There are two primary types of styes, categorized by their location on the eyelid.
- External Stye: This type of stye appears on the outer part of the eyelid and is usually caused by an infection of the Zeis glands (sebaceous glands) or the Moll glands (sweat glands). An external stye typically appears as a tender, red bump on the eyelid margin that resembles a pimple. It can have a yellow or white head, which indicates the presence of pus.
- Internal Stye: An internal stye forms within the eyelid, typically due to an infection of the meibomian glands, which produce the oil component of the tear film. These glands are located in the tarsal plate, the eyelid’s dense connective tissue. Internal styes are more painful than external styes and can result in significant swelling and discomfort. Internal styes, in contrast to external styes, which are visible on the surface of the eyelid, may be difficult to see without everting the eyelid.
Causes of Styes
Styes are primarily caused by bacterial infections, particularly by Staphylococcus aureus, a type of bacteria that lives on the skin and mucous membranes. While these bacteria are typically harmless, they can cause infections if they enter the oil glands of the eyelid. Several factors can increase the likelihood of developing a stye.
- Poor Eyelid Hygiene: Failure to clean the eyelids properly can cause bacteria to build up at the base of the eyelashes, increasing the risk of infection. This is especially important for people who use makeup, particularly eyeliner and mascara, because these products can harbor bacteria if not properly removed.
- Touching the Eyes with Unclean Hands: Frequent contact or rubbing of the eyes with dirty hands can introduce bacteria into the eyelids, resulting in infection. This is a common problem, particularly among children who may be less concerned with hygiene practices.
- Blepharitis: Blepharitis is a chronic inflammation of the eyelid margins that is frequently associated with bacterial overgrowth, seborrheic dermatitis, and meibomian gland dysfunction. Individuals with blepharitis are more likely to develop styes due to the ongoing irritation and risk of bacterial infection.
- Previous Styes: Having had a stye in the past can increase the risk of developing another, especially if the underlying causes of the initial infection are not treated. Recurrent styes may indicate the need for improved eyelid hygiene or the treatment of underlying conditions such as blepharitis.
- Skin Conditions: People with rosacea or seborrheic dermatitis are more likely to develop styes. These conditions frequently involve chronic inflammation and can harm the skin around the eyes, making it more vulnerable to infections.
- Stress and Fatigue: While not direct causes, stress and fatigue can deplete the immune system, making the body more susceptible to infections, including those that cause styes.
- Use of Contaminated Eye Products: Using expired or contaminated eye makeup, contact lenses, or contact lens cases can introduce bacteria into the eyelids, raising the risk of infection. Sharing eye products with others can spread bacteria and cause styes.
- Contact Lens Wear: Improper contact lens handling, such as not washing hands before inserting or removing lenses or failing to properly clean the lenses, can introduce bacteria into the eyelids and increase the risk of developing a stye.
Symptoms of A Stye
The symptoms of a stye can vary depending on the type and severity of the infection, but common signs and symptoms are:
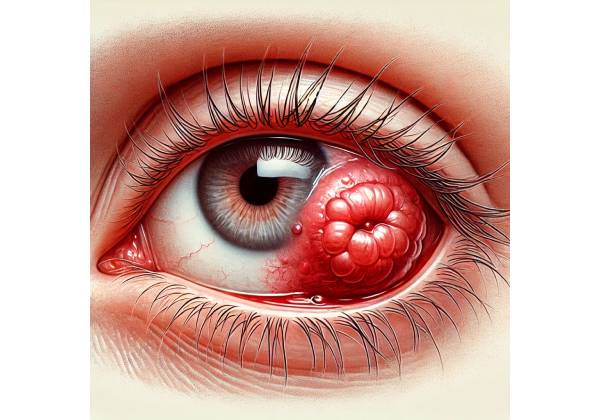
- Red, Swollen Bump: The most visible sign of a stye is a red, swollen bump on the eyelid. This bump can appear on the outer edge of the eyelid (external stye) or within the eyelid (internal stye). The bump may gradually grow in size over a few days and be tender to the touch.
- Pain and Discomfort: Styes are usually painful, especially when touched or blinking. The pain is usually limited to the area around the stye, but it can occasionally spread to the eye and face.
- Tearing and Watery Eyes: The presence of a stye may cause the eye to produce excessive tears, resulting in watery eyes. This is the body’s reflexive response to the stye irritation.
- Crusting Around the Eyelid: Styes can cause a discharge that dries and forms crusts along the eyelid margin. This crusting occurs more frequently in the morning after sleeping, as the discharge accumulates overnight.
- Itching or Burning Sensation: Some people with styes may feel itching or a burning sensation in the affected eyelid. This can be particularly bothersome and may result in rubbing the eyes, exacerbating the condition.
- Light Sensitivity: In some cases, styes can cause photophobia, or sensitivity to light. This symptom is usually mild but can be uncomfortable when exposed to bright light.
- Feeling of a Foreign Body in the Eye: Even if a stye is on the eyelid, it can give the impression that something is in the eye. This foreign body sensation can be irritating, causing the affected person to blink excessively.
- Swelling of the Entire Eyelid: In more severe cases, the stye’s swelling can spread beyond the immediate area of the bump, causing generalized swelling of the entire eyelid. This can make it difficult to fully open your eyes.
- Pus Drainage: In some cases, the stye may come to a head and discharge pus. This drainage can relieve pain and pressure, but it must be managed carefully to avoid spreading the infection.
Complications of A Stye
While styes are usually self-limiting and resolve within a week or two, they can occasionally cause complications, especially if not treated properly. Possible complications include:
- Chalazion: A chalazion is a firm, painless lump that develops when the inflammation from a stye spreads to the surrounding tissues or the meibomian gland becomes clogged. A chalazion, unlike a stye, does not cause redness or pain. However, it can last for a long time and may necessitate medical attention if not resolved on its own.
- Preseptal Cellulitis is a rare but serious complication in which an infection from a stye spreads to the surrounding tissues of the eyelid, resulting in preseptal cellulitis. This condition is characterized by swelling, redness, and pain throughout the eyelid and surrounding areas. To prevent infection from spreading, it is necessary to seek immediate medical attention and receive antibiotic treatment.
- Recurrent Styes: Some people may develop recurrent styes, especially if the underlying causes, such as blepharitis or poor eyelid hygiene, are not treated. Recurrent styes can cause chronic inflammation of the eyelids and may necessitate ongoing treatment to prevent future episodes.
- Scarring: In rare cases, particularly if a stye is repeatedly manipulated or treated incorrectly, the eyelid may become scarred. This can have an impact on the appearance of the eyelid and may necessitate surgical intervention in severe cases.
- Corneal Abrasion: Although uncommon, a large or improperly treated stye can result in a corneal abrasion, which is a scratch on the surface of the cornea. This can happen if the stye rubs against the cornea while blinking or if the patient rubs their eye too much. Corneal abrasions can cause pain and increase the risk of infection, necessitating prompt treatment.
Risks of Developing a Stye
Several factors can increase an individual’s risk of developing a stye, including:
- Age: Styes can happen at any age, but they are more common in children and young adults, most likely due to inconsistent eyelid hygiene practices.
- Contact Lens Wear: People who wear contact lenses, particularly those who do not practice good hygiene, are at a higher risk of developing styes.
- Chronic Skin Conditions: People with chronic skin conditions such as rosacea, seborrheic dermatitis, or acne are more likely to develop styes as a result of ongoing skin inflammation and irritation.
- Immunosuppression: People with weakened immune systems, whether from underlying health conditions or medications, are more vulnerable to infections, including those that cause styes.
- Stress and Fatigue: High levels of stress and fatigue can weaken the immune system, making it easier for infections to spread, including those that cause styes.
Diagnosing Styes: Tests and Examinations
A stye is typically easy to diagnose and can be detected during a comprehensive eye examination by an ophthalmologist or optometrist. Several diagnostic methods are used to confirm the presence of a stye while ruling out other possible causes of eyelid swelling or discomfort.
Clinical Examination
An eye care professional’s clinical examination is the primary method for diagnosing a stye. During the examination, the ophthalmologist or optometrist will carefully examine the affected eyelid, looking for the telltale signs of a stye, such as a red, swollen bump along the eyelid margin or within it. The examiner may also notice pus or a small, white or yellow head on the stye, indicating that the infection is limited.
In the case of an internal stye, the eye care professional may need to evert (flip) the eyelid in order to see the inner surface of the eyelid and the meibomian glands better. This allows for the detection of swelling or infection that may not be obvious from the outside.
The clinical examination also includes assessing the overall health of the eye and eyelids, as well as looking for signs of complications like generalized eyelid swelling (preseptal cellulitis) or evidence of a more serious infection.
Patient History
As part of the diagnostic process, the eye care professional will obtain a thorough patient history. This includes inquiring about the onset and duration of symptoms, any prior history of styes or other eyelid conditions, and any potential risk factors, such as recent use of contaminated eye makeup, contact lens wear, or underlying skin conditions like rosacea or blepharitis.
The patient history assists the clinician in determining the potential causes of the stye and whether any underlying factors need to be addressed to prevent recurrence. Understanding the patient’s hygiene practices, such as how they clean their eyelids or handle contact lenses, can help identify the potential source of the infection.
Slit Lamp Examination
A slit-lamp examination is a common diagnostic tool for evaluating a stye. The slit lamp is a type of microscope that provides a magnified view of the eye and its surrounding structures, such as the eyelids, eyelashes, and meibomian glands.
A slit-lamp examination allows the eye care professional to closely examine the stye, determining its size, location, and the presence of any associated inflammation or discharge. The slit lamp also allows for a thorough examination of the meibomian glands, which are commonly involved in internal styes. This examination can reveal whether the stye is causing blockage or dysfunction in these glands.
In addition to examining the stye, the slit-lamp examination can help the eye care professional look for other conditions that may cause similar symptoms, such as blepharitis, conjunctivitis, or chalazion.
Differential Diagnosis
Differentiating a stye from other eyelid conditions is a critical step in the diagnostic process. While styes are generally easy to diagnose based on their appearance and symptoms, other conditions can mimic styes and necessitate different treatment strategies. Some of the conditions that could be considered in the differential diagnosis are:
- Chalazion: A chalazion, unlike a stye, is caused by a blockage in the meibomian gland, not an infection. A chalazion is a firm, painless lump that grows slowly and is usually located deeper within the eyelid. Chalazia can develop from an untreated or chronic stye, but they require different treatment.
- Preseptal Cellulitis is a more serious condition that causes infection of the eyelid and surrounding tissues. Preseptal cellulitis, as opposed to a stye, causes widespread swelling, redness, and tenderness of the entire eyelid. It requires immediate medical attention and antibiotic treatment.
- Blepharitis: Blepharitis is a chronic inflammation of the eyelid margins that is frequently associated with bacterial overgrowth and seborrheic dermatitis. While blepharitis is not a stye, it can raise the risk of developing one due to ongoing irritation and the possibility of infection.
- Sebaceous Carcinoma: Although uncommon, sebaceous carcinoma is a malignant tumor that appears as a persistent, non-healing lump on the eyelid, similar to a stye or chalazion. If a stye does not resolve with treatment or recurs frequently, additional testing may be required to rule out this serious condition.
Culture and Sensitivity Tests
If a stye is particularly severe, recurrent, or does not respond to standard treatment, the eye care professional may perform a culture and sensitivity test. This entails collecting a sample of pus or discharge from the stye and sending it to a laboratory to determine the specific bacteria causing the infection. The lab can also test the bacteria’s sensitivity to various antibiotics, allowing for more targeted and effective treatment.
While culture and sensitivity testing are not routine for simple, uncomplicated styes, they can be useful in managing more complex cases or when antibiotic resistance is a concern.
Best Practices for Stye Management
To alleviate symptoms, promote healing, and prevent recurrence, effective stye management requires a combination of self-care measures, medical treatments, and preventive strategies. The approach to managing a stye is determined by its severity, whether it is external or internal, and how well it responds to early treatments.
Self-Care & Home Remedies
Most people can successfully manage a stye at home using simple self-care techniques. This includes:
- Warm Compresses: Using a warm compress on the affected eyelid is one of the most effective home remedies for a sty. The warmth increases blood circulation to the area, reducing swelling and promoting pus drainage. To use a warm compress, soak a clean cloth in warm (but not hot) water, wring it out, and gently place it on the closed eyelid for 10 to 15 minutes. This procedure should be repeated three to four times per day until the stye starts to heal.
- Eyelid Hygiene: Keeping your eyelids clean is critical for treating and preventing styes. Gently washing the eyelid with a mild, non-irritating soap or a specially formulated eyelid cleanser can help remove any crusts, debris, or bacteria that may be causing the infection. This should be done on a daily basis, especially if the patient has a history of recurring styes.
- Avoid Squeezing or Popping the Stye: It is critical to avoid squeezing, popping, or attempting to drain the stye yourself, as this can worsen the infection and cause complications. Squeezing the stye may cause the infection to penetrate deeper into the eyelid or spread to other areas.
- Discontinue Use of Eye Makeup and Contact Lenses: During a stye outbreak, it is best to avoid wearing eye makeup and contacts. Eye makeup can harbor bacteria, potentially exacerbating the infection, whereas contact lenses can irritate the eye and introduce additional bacteria. Using glasses during this time can lower the risk of aggravating the stye.
Medical Treatments
If a stye does not improve with home care, or if it is unusually large, painful, or recurring, medical attention may be required. Some of the medical options are:
- Antibiotic Ointments and Drops: For persistent or severe styes, an eye doctor may recommend antibiotic ointments or drops to help fight the infection. These medications are typically applied directly to the affected eyelid, which helps to reduce bacterial load and accelerate healing. In some cases, oral antibiotics may be prescribed, especially if the stye has resulted in a more widespread infection, such as preseptal cellulitis.
- Steroid Injections: In some cases, especially when a stye causes significant inflammation or discomfort, a steroid injection may be used to reduce swelling and accelerate the stye’s resolution. Steroid injections are usually reserved for more severe cases and given by an eye care professional.
- Incision and Drainage: If a stye does not respond to other treatments or causes severe pain and swelling, an eye care professional may recommend a minor surgical procedure to drain it. This procedure, known as incision and drainage, entails making a small cut in the stye to allow pus to drain. The procedure is typically performed in a clinical setting using local anesthesia and provides immediate relief from symptoms.
- Treatment of Underlying Conditions: If a stye is associated with underlying conditions such as blepharitis, rosacea, or meibomian gland dysfunction, treating those conditions is critical to preventing recurrence. Long-term management strategies may include regular eyelid hygiene, medicated eyelid scrubs, or systemic treatments for skin conditions.
Preventive Strategies
Styes can be prevented by adopting habits that reduce the risk of infection while also promoting overall eye health. The key preventive strategies are:
- Maintaining Good Eyelid Hygiene: Cleaning the eyelids on a regular basis helps to prevent the buildup of oils, debris, and bacteria, which can cause styes. This is especially important for people who have had styes before or who have chronic eyelid conditions such as blepharitis.
- Avoiding Touching the Eyes: Limiting contact with the eyes, particularly with unwashed hands, can significantly reduce the risk of introducing bacteria into the eyelids. Simple but effective preventive measures include maintaining good hand hygiene and refraining from rubbing one’s eyes.
- Replace Eye Makeup on a Regular Basis: Old or contaminated eye makeup can harbor bacteria that cause infections. Replace eye makeup, particularly mascara and eyeliner, every three to six months. Avoiding the use of expired or shared makeup products is also essential.
- Proper Contact Lens Care: To avoid eye infections, contact lens wearers must maintain proper hygiene. This includes washing your hands before handling lenses, using the proper cleaning solution, and replacing contact lens cases on a regular basis. Sleeping in contact lenses, unless specifically designed for overnight wear, can also reduce the risk of styes and other eye infections.
Most styes can be effectively managed by combining self-care practices, medical treatments, and preventive strategies, reducing the risk of recurrence. Patients with persistent or recurrent styes require ongoing care and monitoring from an eye care professional.
Trusted Resources and Support
Books
- “The Eyelid Margin: Practical Observations on Blepharitis, Styes, and Chalazia” by Peter V. Brunner: This book provides a comprehensive overview of common eyelid conditions, including styes, offering practical advice for both patients and healthcare providers.
- “Eye Care for All: Preventing and Treating Common Eye Conditions” by Dr. Ruchi Saxena: A practical guide that covers a wide range of eye conditions, including styes, with tips on prevention, treatment, and maintaining overall eye health.
Organizations
- American Academy of Ophthalmology (AAO): The AAO offers a wealth of information on various eye conditions, including styes. Their website provides access to educational resources, patient guides, and a directory of certified ophthalmologists.
- National Eye Institute (NEI): Part of the U.S. National Institutes of Health, the NEI provides extensive research-based information on eye health and diseases, including styes, along with resources for patients and professionals.










