Vitreopapillary traction (VPT) is a rare but serious ocular condition that causes abnormal adhesion between the vitreous body and the optic nerve head, also known as the optic disc or papilla. This condition can cause a variety of visual disturbances and, if not treated, may result in significant visual impairment. Understanding vitreopapillary traction necessitates a thorough examination of the eye’s anatomy, the mechanisms that contribute to this condition, and the symptoms that patients may experience.
Structure of the Vitreous Body and Optic Nerve
To understand vitreopapillary traction, you must first understand the anatomy of the eye, specifically the vitreous body and the optic nerve.
The vitreous body:
The vitreous body, also known as vitreous humor, is a clear gel-like substance that fills the space between the eye’s lens and retina. The vitreous body, which is primarily made up of water, collagen fibers, and hyaluronic acid, helps to keep the eye in shape and provides structural support to the retina. It connects to the retina at several locations, including the macula (the central part of the retina responsible for detailed vision), the peripheral retina, and the optic nerve head.
The optic nerve:
The optic nerve is a bundle of over a million nerve fibers that carry visual information from the retina to the brain. The optic nerve head, also known as the optic disc, is where the optic nerve exits the eye. It is located in the back of the eye and is responsible for relaying images captured by the retina to the visual cortex of the brain.
Pathophysiology of Vitreopapillarary Traction
Vitreopapillary traction occurs when the vitreous humor, which is normally loosely attached to the optic nerve head, causes an abnormal pulling force on the optic disc. This traction can cause structural changes in the optic nerve head, distortion of the surrounding retina, and other visual symptoms.
The vitreous body naturally degenerates with age, a process known as vitreous syneresis. This process involves the liquefaction and shrinkage of the vitreous gel, which results in a partial or complete separation of the vitreous from the retina, known as posterior vitreous detachment (PVD). In most cases, PVD is a normal, benign process that has no significant consequences. In some cases, the vitreous remains abnormally attached to the optic nerve head, resulting in vitreopapillary traction.
The Mechanisms of Vitreopapillary Traction:
The primary mechanism for VPT is the incomplete detachment of the vitreous from the optic nerve head during PVD. When the vitreous fails to detach completely, it exerts a mechanical pulling force on the optic disc, causing deformation of the optic nerve head and surrounding retina. This tractional force can disrupt the normal anatomy and function of the retina, resulting in a variety of visual disturbances.
In addition to age-related changes, other factors may play a role in VPT development. These include high myopia (nearsightedness), which alters the structural relationships within the eye, and conditions like diabetic retinopathy or retinal vein occlusion, which can result in secondary vitreoretinal adhesions.
Symptoms Of Vitreopapillary Traction
The symptoms of vitreopapillary traction vary according to the severity of the condition and the magnitude of the tractional forces applied to the optic nerve head. Some patients may be asymptomatic, especially in the early stages of VPT, whereas others may have severe visual disturbances. Common symptoms associated with vitreopapillary traction are:
1. Visual distortion (metamorphopsia):
Metamorphopsia, in which patients perceive straight lines as wavy or distorted, is one of the most distinguishing features of VPT. This symptom results from the mechanical distortion of the retina caused by the vitreous’ traction on the optic nerve head. Metamorphopsia can have a significant impact on tasks that require accurate vision, such as reading or recognizing faces.
2. Blurred vision:
Patients with VPT may notice gradual blurring of their central vision. This blurring can be mild or severe, depending on the magnitude of the tractional forces and the level of retinal involvement. Individuals with blurred vision may have difficulty engaging in daily activities that require clear, sharp vision.
3. Visual field defects:
In some cases, VPT can cause visual field defects, which are areas of the visual field that are missing or obscured. These defects result from a disruption in normal retinal function and may manifest as dark spots (scotomas) or areas of vision loss in the central or peripheral visual fields.
4. Photopsia (Flashes of Light):
Patients with VPT may report seeing flashes of light, particularly in their peripheral vision. These flashes, known as photopsia, occur when the vitreous exerts tractional forces on the optic nerve head, mechanically stimulating the retina.
5. Floaters:
Patients with VPT frequently report seeing floaters, which are small, shadowy shapes that drift across the visual field. Floaters are typically caused by the aggregation of collagen fibers within the vitreous and may become more visible as the vitreous degrades.
Causes and Risks of Vitreopapillary Traction
Several factors can raise the risk of developing vitreopapillary traction. This includes:
1. Age:
Age is the most important risk factor for VPT. As people age, their vitreous humor naturally degenerates, increasing the risk of incomplete detachment from the optic nerve head and the development of VPT.
**2. **High myopia (nearsightedness)
Individuals with high myopia have a higher risk of developing VPT. The elongated shape of the myopic eye can cause structural changes within the eye, making the vitreous more susceptible to abnormal adhesion to the optic nerve head.
3. Diabetic retinopathy:
Diabetic retinopathy, a retina-related diabetes complication, can cause secondary vitreoretinal adhesions to form. These adhesions can exacerbate vitreopapillary traction and speed up the progression of VPT.
4. Retinal vein occlusion:
Retinal vein occlusion, which is defined as a blockage of blood flow in the retinal veins, can result in retinal ischemia and abnormal vitreoretinal adhesions. These adhesions may increase the risk of VPT.
5. Previous eye surgery:
People who have had cataract surgery or other intraocular procedures may be more likely to develop VPT. Surgical manipulation of the eye can hasten vitreous degeneration and raise the risk of incomplete vitreous detachment from the optic nerve head.
**6. *Inflammatory Eye Conditions*
Chronic inflammation of the eye, such as uveitis, can contribute to the development of VPT by changing the consistency of the vitreous humor and its attachment to the optic nerve head.
Risks of Vitreopapillary Traction
If left untreated, vitreopapillary traction can cause a number of serious complications, including permanent vision loss. The complications include:
1. Optic disc edema:
Vitreopapillary traction can cause optic disc edema, which is the swelling of the optic nerve head. This swelling can worsen vision and indicate a more serious underlying problem.
2. Macular edema:
The vitreous’s traction on the optic nerve head can extend to the macula, resulting in macular edema. The accumulation of fluid within the macula causes additional visual distortion and decreased visual acuity.
3. Retinal detachment:
In rare cases, severe VPT can cause retinal detachment, in which the retina pulls away from the underlying tissue layers. Retinal detachment is a medical emergency that requires immediate surgical intervention to avoid permanent vision loss.
4. Progressive Visual Loss:
Over time, the vitreous’ continuous traction on the optic nerve head can cause progressive vision loss. This loss can occur gradually or suddenly, depending on the severity of the condition and the presence of complications.
Effects on Quality of Life
Vitreopapillary traction can significantly improve a person’s quality of life, especially as the disease progresses and symptoms worsen. Visual disturbances caused by VPT, such as visual distortion, blurred vision, and visual field defects, can make it difficult to perform daily tasks that require sharp central vision. Reading, driving, and using digital devices can become increasingly difficult, causing frustration and a loss of independence.
Moreover, the psychological impact of VPT should not be underestimate. The fear of losing vision, as well as the uncertainty about the condition’s progression, can cause anxiety and depression. Individuals with VPT may also feel isolated or self-conscious about their visual impairments, especially if they are unable to participate in social activities or hobbies that they previously enjoyed.
Given the risk of significant visual impairment, individuals with VPT should seek regular eye examinations and appropriate treatment to manage the condition and avoid complications.
Diagnostic Approaches for Vitreopapillary Traction
Vitreopapillary traction is diagnosed using a combination of clinical evaluation, imaging techniques, and a thorough assessment of the patient’s symptoms. The goal is to detect the presence of VPT, assess the amount of vitreous traction on the optic nerve head, and determine the best course of action. Several diagnostic methods are frequently used to assess VPT:
1. Clinical Examination
- Visual Acuity Testing: To determine visual acuity and identify any reductions. This test assesses the effect of vitreopapillary traction on the patient’s central vision, which is critical for activities that require detailed vision.
- Slit-Lamp Biomicroscopy: A slit-lamp examination enables the clinician to thoroughly examine the anterior and posterior segments of the eye. The clinician can use specialized lenses to closely inspect the vitreous body and the optic nerve head, looking for abnormal adhesions, traction, or signs of optic disc edema. This examination is critical for detecting structural changes indicative of VPT.
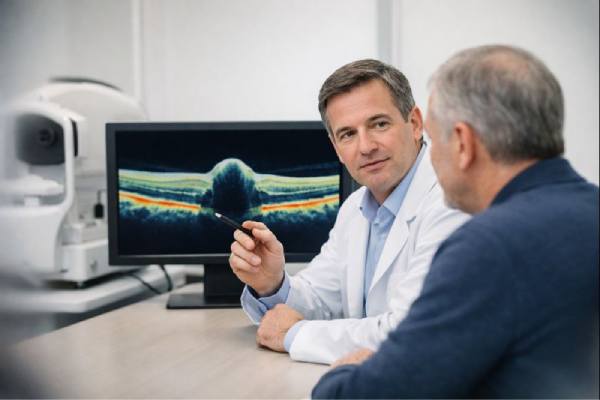
2. Optical Coherence Tomography (OCT
Optical Coherence Tomography (OCT) is the gold standard imaging method for diagnosing vitreopapillary traction. OCT is a non-invasive, high-resolution imaging technique that produces cross-sectional views of the retina and optic nerve head. It allows clinicians to see the vitreous interface and optic disc in great detail.
OCT can detect the extent of vitreous traction on the optic nerve head, as well as any changes in the surrounding retinal tissue, such as thickening, distortion, or macular edema. It is especially useful for tracking the progression of VPT over time and determining the efficacy of any treatment interventions.
3. B-scan ultrasonography
B-scan ultrasonography is an important diagnostic tool, particularly when OCT is insufficient due to medial opacities (such as cataracts) that obscure the view of the retina. This ultrasound technique produces a two-dimensional cross-sectional image of the eye’s internal structures, such as the vitreous and optic nerve head.
B-scan ultrasonography can detect vitreous adhesions, confirm the presence of vitreopapillary traction, and evaluate the overall health of the vitreous body and retina. It can also aid in the identification of VPT-related complications such as retinal detachment or vitreous hemorrhage.
4. Fundus Photography
Fundus photography is the process of capturing detailed images of the retina and optic nerve head with a specialized camera. While fundus photography is not as detailed as OCT, it is an effective tool for documenting the appearance of the optic disc and surrounding retina. It can detect optic disc edema, hemorrhages, and other abnormalities associated with vitreopapillary traction.
These images provide a visual record that can be used to monitor changes over time, especially in response to treatment or as the condition worsens. Fundus photography is frequently used in conjunction with other imaging modalities to provide a complete picture of the retinal and optic nerve health.
5. Fluorescein angiography
Fluorescein angiography is a diagnostic procedure that involves injecting a fluorescent dye into the bloodstream and taking a series of photographs as it circulates through the retinal blood vessels. This test is especially useful for determining blood flow to the retina and optic nerve head.
Fluorescein angiography can help identify areas of compromised blood flow, retinal ischemia, or leakage caused by vitreous tractional forces. While it is not the primary method for diagnosing VPT, it can reveal important information about associated vascular changes or complications.
6. Visual Field Testing
Visual field testing, also known as perimetry, evaluates the patient’s entire visual field, including peripheral vision. This test detects visual field defects caused by vitreopapillary traction, such as scotomas or areas of vision loss. By mapping the visual field, clinicians can gain a better understanding of how VPT affects the patient’s vision.
Visual field testing is especially useful for tracking the progression of VPT and determining whether the condition is affecting the optic nerve function in general.
Approaches to Vitreopapillary Traction Management
Managing vitreopapillary traction (VPT) requires a variety of approaches, depending on the severity of the condition, the presence of symptoms, and the likelihood of complications. The management strategy is individualised for each patient, taking into account the impact of VPT on their vision and quality of life. The following are the primary methods for managing VPT:
1. Observation and Monitoring
Patients with mild VPT, particularly those who are asymptomatic or have minimal symptoms, may benefit from a conservative approach of observation and regular monitoring. In some cases, the vitreous humor may gradually detach from the optic nerve head, relieving traction without the need for intervention.
This approach requires regular follow-up visits with an eye care provider. During these visits, the patient’s visual acuity is evaluated, and imaging tests such as Optical Coherence Tomography (OCT) are used to track the progression of VPT. Patients should also monitor their vision at home and report any changes in symptoms, such as increased visual distortion, blurred vision, or the appearance of new floaters.
If the condition remains stable and the symptoms do not worsen, the observation period may continue. However, if the condition worsens or the symptoms significantly impair the patient’s quality of life, more aggressive treatment options may be considered.
2. Pharmaceutical Treatment
VPT is primarily mechanical rather than inflammatory or vascular, so pharmacological treatment is generally limited in its management. However, in some cases where inflammation is present or associated with conditions such as uveitis, corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce inflammation and relieve symptoms.
For patients with diabetic retinopathy or other retinal conditions that worsen VPT, controlling the underlying disease with systemic medications or intravitreal injections (e.g., anti-VEGF therapy) can be an important part of the overall management strategy. These treatments aim to stabilize the retinal environment, which may reduce vitreous adhesion and traction.
3. Surgical Intervention
Patients with more advanced VPT frequently require surgical intervention, especially if they have significant visual distortion, decreased visual acuity, or complications such as macular edema or retinal detachment. Vitrectomies are the most common surgical procedure for VPT.
Vitrectomy:
Vitrectomy is the removal of vitreous gel from the eye, which eliminates traction on the optic nerve head. During the procedure, small incisions are made in the eye and the vitreous is carefully removed using specialized instruments. In cases where an epiretinal membrane (ERM) has formed, the surgeon may peel it away to reduce traction and restore the retina’s normal structure.
Vitrectomy is an extremely effective procedure for relieving vitreopapillary traction and improving visual outcomes. However, there are some risks, such as cataract formation, retinal detachment, infection, and intraocular bleeding. The patient and their eye care provider should have a thorough discussion about the potential benefits and risks of vitrectomy before making the decision.
Surgical Treatment of Complications:
If VPT has resulted in complications such as macular edema or retinal detachment, additional surgical procedures may be required. For example, if there is macular edema, the surgeon may perform additional procedures to drain the fluid and restore the macula’s normal contour. In the case of retinal detachment, more extensive surgical repair may be required, such as the use of a gas bubble or silicone oil to tamponade the retina and encourage reattachment.
4. Lifestyle Changes and Supportive Care
In addition to medical and surgical treatments, lifestyle modifications and supportive care can help manage VPT:
- Visual Aids: Patients with VPT may benefit from visual aids such as magnifiers, brighter lighting, and adaptive devices to assist with reading and other tasks that require sharp vision. These aids can improve daily functioning and mitigate the effects of visual distortion.
- Regular Eye Examinations: Regular follow-up with an eye care provider is essential for tracking the progression of VPT and adjusting the treatment plan as needed. Early detection of complications can result in timely intervention and better visual outcomes.
- Psychological Support: Counseling or support groups can be beneficial to patients who are experiencing anxiety or depression as a result of their fear of losing their vision.
Eye care professionals can effectively manage VPT by combining observation, pharmacological treatments, surgical options, and supportive care to help patients keep their vision and quality of life.
Trusted Resources and Support
Books
- “Retina” by Stephen J. Ryan, MD
This comprehensive textbook provides detailed information on various retinal conditions, including vitreopapillary traction, making it an essential resource for both clinicians and patients seeking to understand the condition better. - “The Vitreous: Structure, Function, and Pathology” by J. Sebag, MD
This book offers an in-depth exploration of the vitreous body’s role in ocular health and disease, including conditions like VPT, providing valuable insights into the underlying mechanisms and potential treatments.
Organizations
- American Academy of Ophthalmology (AAO)
The AAO offers a wide range of resources, including information on vitreopapillary traction, its diagnosis, and management. The website provides access to patient education materials and the latest research in ophthalmology. - The Retina Society
An organization dedicated to advancing knowledge and research in retinal diseases. Their website offers educational materials, support resources, and updates on the latest developments in the treatment of conditions like vitreopapillary traction.






