What is vitreoretinal lymphoma?
Vitreoretinal lymphoma (VRL) is a rare and aggressive cancer that affects the eye, particularly the vitreous and retina. It is a subtype of PCNSL, a non-Hodgkin lymphoma. Malignant lymphoid cells infiltrate the vitreous body and retina of the eye, causing a variety of ocular symptoms. Because of its rarity and non-specific symptoms, vitreoretinal lymphoma is frequently difficult to diagnose, and its aggressive behavior necessitates prompt recognition and treatment.
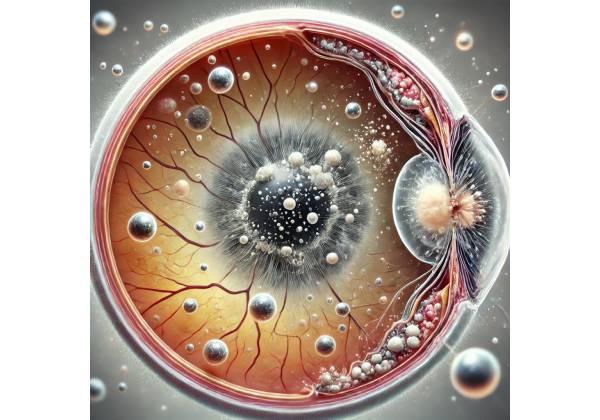
Understanding Anatomy: Vitreous and Retina
To fully comprehend the implications of vitreoretinal lymphoma, it is necessary to first understand the structures it affects: the vitreous and the retina.
The vitreous body:
The vitreous body is a clear, gel-like substance that fills the space between the lens and the retina, helping to keep the eye in shape and serving as a medium for light to pass through to the retina. The vitreous is normally transparent, allowing for clear vision; however, in conditions such as VRL, it can become clouded by the infiltration of malignant cells.
The retina:
The retina is a thin, light-sensitive layer of tissue that lines the back of the eye. It plays an important role in vision by converting light into electrical signals that are then transmitted to the brain via the optic nerve. The macula, located in the center of the retina, is in charge of providing the high-acuity vision required for tasks like reading and face recognition. Any condition affecting the retina can have a significant impact on vision, and VRL can cause serious visual impairment.
Pathogenesis of Vitreoretinal Lymphoma
Vitreoretinal lymphoma develops from malignant lymphocytes, a type of white blood cell involved in the immune response. VRL lymphocytes are typically of the B-cell lineage, though T-cell variants do exist but are even rarer. The exact cause of VRL is unknown, but it is thought to be the result of genetic mutations that cause uncontrolled growth and proliferation of these lymphocytes.
VRL can be classified into two major types based on its origin:
**1. Primary vitreoretinal lymphoma:
This type of VRL develops primarily in the eye and may or may not be associated with central nervous system involvement at the time of presentation. However, up to 80% of patients with primary VRL will develop CNS involvement, demonstrating the disease’s aggressive nature.
2. Secondary Vitreoretinal Lymphoma:
Secondary VRL develops when lymphoma from another part of the body, such as the central nervous system or lymph nodes, spreads to the eye. This type of VRL is frequently part of a larger systemic disease and is associated with a poor prognosis.
Malignant lymphocytes infiltrate the vitreous humor and retinal layers, causing inflammation, retinal detachment, and other structural changes to the eye. The presence of these cells in the vitreous can cause a characteristic “vitritis,” or vitreous inflammation, which is frequently mistaken for uveitis, a more common inflammatory condition. This misdiagnosis can delay the proper diagnosis of VRL, allowing the disease to progress.
Symptoms of Vitreoretinal Lymphoma
The symptoms of vitreoretinal lymphoma can be unpredictable and nonspecific, making early detection difficult. Patients frequently present with symptoms similar to other more common ocular conditions, such as uveitis or retinal detachment. Common symptoms of VRL are:
1. Blurred vision:
A gradual, painless loss of vision, often described as blurred or hazy, is one of the most common symptoms of VRL. This occurs when malignant cells infiltrate the vitreous and retina, disrupting their normal function. Blurred vision can affect one or both eyes, and it usually progresses.
2. Floaters:
Patients with VRL frequently report the presence of floaters, which are small, shadowy shapes that appear to drift across their visual fields. Cliques of malignant cells within the vitreous cause these floaters, which cast shadows on the retina. The number and density of floaters may increase as the disease progresses.
3. Photopsia (Flashes of Light):
Some VRL patients experience photopsia, which are flashes of light in the visual field. These flashes are usually caused by retinal irritation or traction as a result of malignant cells or associated retinal detachment.
4. Visual field defects:
As the disease progresses, VRL can cause visual field defects, in which parts of the visual field become obscured or lost. These defects can be central or peripheral, and they are frequently caused by lymphoma involvement in the retina or optic nerve.
5. Red Eyes and Pain:
Although less common, some VRL patients may experience eye redness (conjunctival injection) and ocular pain. These symptoms are typically associated with more advanced disease or secondary complications, such as elevated intraocular pressure.
Risk Factors of Vitreoretinal Lymphoma
Several factors can increase the risk of developing vitreoretinal lymphoma, but the exact cause is frequently unknown. The risk factors include:
1. Age:
VRL primarily affects older adults, with most cases occurring in people over the age of 60. The incidence of VRL rises with age, most likely due to the higher risk of lymphomas in this population.
2. Immunosuppression:
Individuals with weakened immune systems, such as those with HIV/AIDS, organ transplant recipients, or patients undergoing immunosuppressive therapy, are more likely to develop VRL. Immunosuppression can cause the uncontrolled growth of malignant lymphocytes, increasing the risk of lymphoma development.
3. Genetic predisposition:
While the exact genetic factors underlying VRL are unknown, there may be a hereditary component in some cases. People with a family history of lymphoproliferative disorders or other cancers may be more likely to develop VRL.
4. Previous history of lymphoma:
Patients with a history of systemic lymphoma, particularly central nervous system lymphoma, are at higher risk for secondary VRL. The disease could spread to the eye as part of a larger systemic involvement.
Complications Of Vitreoretinal Lymphoma
Vitreoretinal lymphoma is a serious condition that can lead to severe complications, especially if left untreated or diagnosed late. Some of the major complications associated with VRL are:
1. Central Nervous System Involvement:
One of the most serious concerns in VRL is the possibility of central nervous system involvement. Up to 80% of patients with primary VRL will develop CNS lymphoma, which has a poorer prognosis and requires more complex management.
2. Retinal detachment:
Malignant cell infiltration into the retina can cause retinal detachment, which occurs when the retina separates from the supporting tissue. Retinal detachment can result in severe vision loss and may necessitate surgical intervention.
3. Vision loss:
As VRL progresses, malignant cells accumulate in the vitreous and retina, causing significant and sometimes irreversible vision loss. A variety of factors can contribute to vision loss, including retinal detachment, optic nerve involvement, and the direct effects of the lymphoma on retinal function.
4. Misdiagnosis and Delay Treatment:
Because of the nonspecific nature of its symptoms, VRL is frequently misdiagnosed as uveitis or other inflammatory eye conditions. This misdiagnosis can result in ineffective treatment and a delay in starting the proper therapy, allowing the disease to progress unchecked.
5. Systematic spread:
Secondary VRL is a type of systemic lymphoma that can spread to other organs and tissues, resulting in widespread complications and a poor prognosis.
Given the aggressive nature of vitreoretinal lymphoma and the possibility of serious complications, early detection and accurate diagnosis are essential. Understanding the symptoms and risk factors associated with VRL can assist healthcare providers in identifying the condition more quickly, allowing for timely and effective treatment.
Diagnostic methods
Vitreoretinal lymphoma is difficult to diagnose due to its rarity and nonspecific symptoms. Several diagnostic methods are available to help identify and distinguish this condition from other ocular diseases.
1. Clinical Examination
The first step in diagnosing VRL is a thorough clinical examination by an ophthalmologist or retina specialist. This exam typically includes:
- Visual Acuity Testing: To determine the sharpness of vision and any reduction in visual acuity, which is common in VRL due to malignant cell infiltration into the vitreous and retina.
- Slit-Lamp Biomicroscopy: This technique enables the clinician to thoroughly examine the anterior and posterior segments of the eye. The examiner can use a slit lamp to look for cells, clumps, or other abnormalities in the vitreous that indicate VRL. The retina can also be checked for signs of inflammation, hemorrhages, and retinal detachment.
2. Optical Coherence Tomography (OCT
Optical Coherence Tomography (OCT) is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and vitreous. OCT is especially effective at detecting structural changes in the retina and vitreous caused by VRL. It can detect vitreous opacities, retinal thickening, subretinal fluid, and other abnormalities that indicate the presence of malignant cells.
OCT is frequently used to track the progression of VRL and evaluate treatment outcomes. It can also assist in distinguishing VRL from other conditions such as uveitis or other retinal diseases by providing detailed images of the retinal layers and any associated abnormalities.
3. Vitreous and retinal biopsy
A vitreous or retinal biopsy is frequently necessary to make a definitive diagnosis of vitreoretinal lymphoma. During this procedure, a small amount of vitreous humor or retinal tissue is collected and sent to a laboratory for testing. This biopsy is usually performed with a fine needle aspiration or during a vitrectomy procedure. The collected sample is then examined under a microscope to identify malignant lymphocytes and evaluate their properties.
Immunohistochemistry and flow cytometry are common techniques for analyzing biopsy samples. These methods enable the identification of specific cell surface markers that are unique to lymphoma cells, which aids in the confirmation of the VRL diagnosis. Molecular testing, such as polymerase chain reaction (PCR), can also be used to identify genetic mutations or rearrangements associated with lymphoma.
4. Fluorescein angiography
Fluorescein angiography is another useful method for detecting vitreoretinal lymphoma. This procedure entails injecting a fluorescent dye into a vein, usually in the arm, which then circulates through the blood vessels in the retina. As the dye passes through the retinal vasculature, the clinician takes a series of photographs to monitor blood flow and identify any abnormalities.
Fluorescein angiography in VRL can detect areas of retinal vascular leakage, which appear as hyperfluorescent spots on the angiogram. It can also detect retinal edema, hemorrhages, and other lymphoma-related retinal complications. While fluorescein angiography is not specific to VRL, it can provide useful evidence when combined with other diagnostic methods.
5. Cytology and flow cytometry
Cytology is the examination of cells under a microscope to determine their type and detect any abnormalities. Cytology is used in VRL to examine samples obtained via a vitreous tap or biopsy. Malignant cells in VRL usually appear as large, atypical lymphocytes with irregular nuclei and prominent nucleoli.
Flow cytometry is a more advanced technique for analyzing cell surface markers on lymphocytes. This method identifies specific markers associated with B-cell or T-cell lymphomas, which helps to distinguish VRL from other ocular conditions. Flow cytometry can also reveal information about the clonality of the lymphocyte population, which indicates malignancy.
6. Image of the Central Nervous System
Given the strong link between primary vitreoretinal lymphoma and central nervous system (CNS) involvement, brain imaging studies are frequently performed as part of the diagnostic process. Magnetic resonance imaging (MRI) is the preferred method for detecting lymphoma in the central nervous system. An MRI can detect lesions in the brain or spinal cord that may indicate CNS involvement, which is critical for disease staging and determining the best treatment plan.
In some cases, a lumbar puncture may be necessary to obtain cerebrospinal fluid (CSF) for analysis. The presence of malignant cells in the CSF confirms CNS involvement and guides disease management.
7. Ancillary tests
Additional tests may be required to confirm the diagnosis of vitreoretinal lymphoma or rule out other conditions. These may include:
- Blood Tests: To assess overall health, immune function, and identify markers associated with systemic lymphoma.
- Electrophysiological Testing: This includes electroretinography (ERG) to assess retinal function, which may be impaired in advanced VRL.
- Ocular Ultrasound: To evaluate the vitreous and retina in cases where direct visualization is difficult due to media opacities.
Best Practices in Vitreoretinal Lymphoma Treatment
Given the strong association with central nervous system (CNS) involvement, treating vitreoretinal lymphoma (VRL) is a complex process that necessitates a multidisciplinary approach involving ophthalmologists, oncologists, and possibly neurologists. VRL management strategies are tailored to each individual patient, taking into account factors such as ocular involvement, CNS or systemic disease, and overall health. The treatment goals include controlling the lymphoma, preserving vision, and preventing disease progression.
1. Systemic Chemotherapy
Systemic chemotherapy is an essential component of VRL management, especially in cases involving the central nervous system or spreading throughout the body. The most commonly used chemotherapeutic agents are high-dose methotrexate, cytarabine, and rituximab, a monoclonal antibody that targets CD20, a protein found in B-cell lymphomas. These drugs are administered intravenously and can cross the blood-brain barrier, making them effective against both ocular and CNS lymphoma.
High-dose methotrexate is especially effective in treating primary CNS lymphoma and VRL because it can cross the blood-brain barrier and reach therapeutic concentrations in the brain and eyes. This treatment is typically administered in cycles, with careful monitoring for potential side effects such as myelosuppression, nephrotoxicity, and mucositis. Rituximab is frequently added to chemotherapy regimens for its targeted action on B-cell lymphomas, which improves overall treatment efficacy.
2. Intravitreal Chemotherapy
Intravitreal chemotherapy is the direct injection of chemotherapeutic agents into the vitreous cavity of an eye. This localized treatment delivers high concentrations of the drug directly to the lymphoma site, reducing systemic exposure and associated side effects. The most common agents used for intravitreal chemotherapy in VRL are methotrexate and rituximab.
Intravitreal methotrexate is usually given in a series of injections over several weeks, with careful monitoring of the patient’s response and any side effects, such as inflammation or increased intraocular pressure. Intravitreal rituximab is also effective, especially when the lymphoma is resistant to other therapies. This method is particularly useful in the treatment of VRL that is limited to the eye or in cases where systemic therapy is unacceptable.
3. Radiation Therapy
Radiation therapy is another treatment option for VRL, especially when there is no CNS involvement or when chemotherapy is not an option. External beam radiation therapy (EBRT) can be administered to either the affected eye or both eyes, depending on the severity of the disease. Radiation therapy works by damaging cancer cells’ DNA, which inhibits their ability to grow and divide.
Radiation doses and schedules are carefully designed to minimize damage to surrounding healthy tissue, particularly the retina and optic nerve, while maximizing the therapeutic effect on the lymphoma. However, radiation therapy is associated with a risk of side effects such as cataract formation, radiation retinopathy, and optic neuropathy, all of which can result in vision loss. As a result, it is typically reserved for cases in which other treatment options are ineffective or as an adjunct to systemic therapy.
4. Combined Modality Therapy
Given VRL’s aggressive nature, combined modality therapy—a combination of systemic chemotherapy, intravitreal chemotherapy, and radiation therapy—is frequently used to maximize treatment efficacy. This approach aims to control the lymphoma both locally in the eye and systemically, lowering the risk of CNS involvement and relapse.
A patient, for example, may receive intravitreal methotrexate injections to manage the ocular component of VRL, followed by systemic chemotherapy to address any potential CNS involvement. Radiation therapy may be used to strengthen the response and lower the risk of recurrence. The specific combination and sequence of treatments are determined by the patient’s disease characteristics and overall health.
5. Monitoring and Follow-up
Continuous monitoring and follow-up are essential parts of VRL management. Regular eye examinations, including slit-lamp biomicroscopy and Optical Coherence Tomography (OCT), are required to assess treatment response and detect signs of recurrence. Imaging tests, such as MRI, are also used to monitor CNS involvement or progression.
In addition to clinical monitoring, patients with VRL require supportive care to manage potential chemotherapy or radiation side effects such as neutropenia, mucositis, and ocular complications. Close collaboration among ophthalmologists, oncologists, and other specialists is required to provide comprehensive care.
6. Emerging Therapies and Research
New VRL treatments are being developed with the goal of improving outcomes and reducing treatment-related toxicity. Immunotherapy, which uses the body’s immune system to fight cancer, is a field of active research. Immune checkpoint inhibitors, CAR T-cell therapy, and novel monoclonal antibodies all show promise in the treatment of VRL, especially in cases resistant to conventional therapies.
Clinical trials are critical for determining the safety and efficacy of emerging therapies, and patients with VRL may be eligible to participate. These studies help to develop new treatment options and provide access to cutting-edge therapies that can improve patient outcomes.
Trusted Resources and Support
Books
- “Ocular and Adnexal Lymphoma” by Arun D. Singh, MD
This comprehensive resource provides detailed information on various ocular lymphomas, including vitreoretinal lymphoma, offering valuable insights into diagnosis, management, and treatment strategies. - “Ocular Oncology: Clinical Diagnosis and Treatment” by Swathi Kaliki, MD
This book covers a wide range of ocular oncology topics, including vitreoretinal lymphoma, with a focus on clinical diagnosis and therapeutic approaches, making it a useful reference for both clinicians and patients.
Organizations
- American Academy of Ophthalmology (AAO)
The AAO provides extensive resources on ocular conditions, including vitreoretinal lymphoma. Their website offers patient education materials, the latest research updates, and access to expert opinions on managing this rare condition. - Lymphoma Research Foundation (LRF)
The LRF is dedicated to funding lymphoma research and providing support to patients and caregivers. Their resources include detailed information on different types of lymphoma, including VRL, and access to clinical trials and patient support networks.










