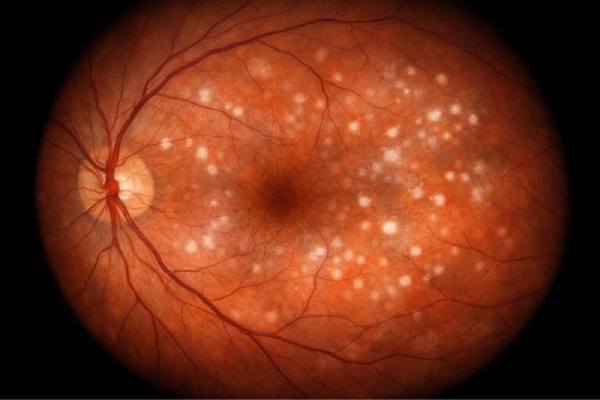
White dot syndromes (WDS) are a collection of rare, idiopathic inflammatory conditions that primarily affect the retina, retinal pigment epithelium (RPE), and choroid. Multiple white or yellow-white lesions, or “dots,” within the retina and choroid, which are often visible during fundoscopic examination, distinguish these syndromes. White dot syndromes are thought to be caused by immune-mediated inflammation, which could be triggered by viral infections, genetic predisposition, or autoimmune disorders. However, the precise cause is unknown.
The term “white dot syndromes” refers to a number of distinct clinical entities, each with its own unique characteristics, demographic preferences, and disease progression. The most common white dot syndromes are acute posterior multifocal placoid pigment epitheliopathy (APMPPE), multifocal choroiditis and panuveitis (MCP), birdshot chorioretinopathy (BCR), multiple evanescent white dot syndrome (MEWDS), punctate inner choroidopathy (PIC), and serpiginous choroiditis (SC). Each of these conditions has distinct clinical and imaging findings, but they all share the presence of white lesions in the retina or choroid.
Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPE)
APMPPE is an inflammatory condition that primarily affects young adults, typically aged 20 to 40. It is distinguished by the sudden onset of blurred vision, which is frequently accompanied by scotomas (areas of partial or complete vision loss) and photopsia (flashes of light). The condition is typically bilateral, but it can be asymmetric, which means that one eye may be more severely affected than the other.
- Clinical Presentation: Patients with APMPPE usually have multiple, creamy white placoid lesions at the level of the RPE, primarily in the posterior pole of their retina. These lesions may combine to form larger areas of involvement. The lesions may resolve spontaneously over time, leaving areas of pigmentation or atrophy in the RPE.
- Course and Prognosis: The visual prognosis for APMPPE is generally good, with many patients experiencing gradual vision improvement over weeks or months. However, some people may experience chronic or recurring inflammation, which can result in significant visual impairment.
Multifocal Choroiditis and Panuveitis(MCP)
MCP is an inflammatory condition that affects both the choroid and the retina, and is frequently associated with severe vitritis. It primarily affects young to middle-aged women and is typically bilateral.
- Clinical Presentation: Multiple, small, yellow-white lesions in the choroid and RPE are the hallmark of MCP. These lesions can progress over time, resulting in chorioretinal scars and pigmentary changes. Patients may present with blurred vision, floaters, or photopsia. MCP is frequently associated with panuveitis, which causes inflammation in all layers of the uvea, including the iris, ciliary body, and choroid.
- Course and Prognosis: MCP can be chronic and relapsing, with periods of rest followed by episodes of active inflammation. Chronic inflammation can lead to serious complications, such as choroidal neovascularization (CNV), which can cause permanent vision loss.
Birdshot Chorioretinopathy(BCR)
Birdshot chorioretinopathy, also known as birdshot retinochoroidopathy, is a chronic, bilateral, inflammatory disease that primarily affects people of European ancestry, typically aged 40 to 60. The name “birdshot” refers to the distinctive appearance of fundus lesions, which resemble birdshot pellets scattered across the retina.
- Clinical Presentation: BCR is characterized by multiple, small, cream-colored lesions scattered across the retina’s posterior pole and midperiphery. These lesions are located near the choroid and RPE. Patients with BCR frequently exhibit bilateral blurred vision, night blindness, and loss of peripheral vision. The HLA-A29 allele is strongly associated with the condition, and genetic testing for this marker is frequently part of the diagnostic process.
- Course and Prognosis: BCR is a chronic, progressive condition that, if not treated properly, can cause significant visual impairment. Inflammation can lead to retinal atrophy, cystoid macular edema (CME), and optic nerve damage, all of which contribute to vision loss over time.
Multiple Evanescent White Dot Syndrome (MEWDS)
MEWDS is an acute, self-limiting condition that primarily affects young, healthy women. The sudden onset of blurred vision in one eye, often accompanied by photopsia and an enlarged blind spot, distinguishes it.
- Clinical Presentation: MEWDS is defined by the presence of multiple, small, white or gray-white dots in the outer retina and RPE, primarily in the posterior pole. These dots are often subtle and can be difficult to detect during a clinical examination. In some cases, there may be mild vitritis or swelling of the optic disc.
- Course and Prognosis: MEWDS usually resolves spontaneously within a few weeks to months, with most patients regaining full vision. The lesions gradually fade, and the visual outcome is generally favorable. However, some people may have mild residual symptoms, such as a persistent blind spot or a minor photopsia.
Punctate Inner Choroidopathy (PIC)
PIC is an inflammatory condition that affects mostly young myopic women. Small, yellow-white lesions at the level of the inner choroid and RPE, typically located in the posterior pole, distinguish it.
- Clinical Presentation: Patients with PIC usually have sudden blurred vision, scotomas, and photopsia. PIC lesions are small, round, and well-defined, and they can combine over time to form larger areas of involvement. PIC is typically unilateral, but it can become bilateral in certain circumstances.
- Course and Prognosis: PIC can have a chronic, relapsing course, with periods of inflammation followed by periods of rest. The condition is associated with an increased risk of developing CNV, which can cause significant visual impairment if not treated promptly.
Serpiginous Choroiditis(SC)
Serpiginous choroiditis is a chronic, progressive inflammatory disorder that primarily affects the choroid and RPE. It is distinguished by the presence of serpentine or geographic lesions that extend from the optic disc or other areas of the retina.
- Clinical Presentation: Patients with SC typically have blurred vision, scotomas, and photopsia that develop gradually. Lesions of SC are frequently described as “serpentine” or “geographic” in appearance, with a preference for the peripapillary region. These lesions can spread over time, resulting in large areas of chorioretinal atrophy.
- Course and Prognosis: SC is a chronic, relapsing condition that can cause severe visual impairment over time. Because of the disease’s progressive nature and the risk of developing CNV, it is one of the most visually debilitating white dot syndromes.
Common Features of White Dot Syndromes
While each type of white dot syndrome has its own distinct features, these conditions share a few common characteristics:
- Idiopathic Nature: The exact cause of white dot syndromes is unknown, but they are thought to be the result of immune-mediated inflammation. Potential triggers include viral infections, genetic predisposition, and autoimmune disorders.
- Bilateral Involvement: Most white dot syndromes affect both eyes, though the severity of involvement may differ between the two.
- Relapsing-Remitting Course: Many white dot syndromes have a chronic, relapsing course that alternates between periods of active inflammation and periods of quiescence. This pattern can cause cumulative damage to the retina and choroid, resulting in progressive visual impairment.
- Association with Choroidal Neovascularization (CNV): Several white dot syndromes, including MCP, PIC, and SC, are linked to the development of CNV, a condition in which abnormal blood vessels grow beneath the retina, resulting in severe vision loss.
- Variable Prognosis: The visual prognosis for white dot syndromes varies greatly depending on the underlying condition, the severity of inflammation, and the presence of complications. While some conditions, such as MEWDS, have a good prognosis with spontaneous resolution, others, such as SC and BCR, can cause significant and permanent visual impairment if not treated properly.
Diagnostic methods
A detailed patient history, clinical examination, and advanced imaging techniques are required to diagnose white dot syndromes. Given the complexities and variability of these conditions, accurate diagnosis is critical for guiding appropriate management and treatment options.
Patient History and Clinical Examination
The diagnostic process starts with a thorough patient history, which focuses on the onset, duration, and nature of symptoms. Patients with white dot syndromes frequently report sudden onset blurred vision, scotomas, photopsia, and, in some cases, a previous viral illness. The clinician will ask about any recent infections, autoimmune diseases, or other systemic symptoms that may be associated with the condition.
- Visual Acuity Testing: Visual acuity is used to assess the severity of visual impairment. The degree of vision loss varies according to the type and severity of white dot syndrome.
- Slit-Lamp Examination: A slit-lamp examination enables the clinician to examine the anterior segment of the eye, including the cornea, lens, and anterior chamber, for signs of inflammation or other abnormalities.
- Fundoscopic Examination: The fundoscopic examination is a critical component of diagnosing white dot syndromes. The ophthalmologist uses an ophthalmoscope to examine the retina, retinal pigment epithelium (RPE), and choroid for the presence of characteristic white or yellow-white lesions. These lesions can differ in size, shape, and distribution depending on the type of white dot syndrome. The fundoscopic examination aids in the identification of key features such as placoid lesions in APMPPE, cream-colored spots in birdshot chorioretinopathy, and serpentine patterns in serpiginous choroiditis.
Advanced Imaging Techniques
Advanced imaging techniques are required to confirm the diagnosis of white dot syndromes and determine the degree of retinal and choroidal involvement. These imaging modalities provide detailed information that may not be visible during a routine clinical examination.
Fluorescein Angiography (FA)
Fluorescein angiography is a popular imaging technique that involves injecting a fluorescent dye into the bloodstream and taking a series of images as it travels through the retinal and choroidal blood vessels. FA is especially useful in detecting areas of retinal and choroidal inflammation, as well as choroidal neovascularization (CNV).
- Early and Late Phases: In the early stages of FA, the dye focuses on the retinal and choroidal circulation, allowing the clinician to assess the blood-retinal barrier. In the later stages, hyperfluorescence may indicate active inflammation or leakage, whereas hypofluorescence may indicate chorioretinal atrophy or scarring.
- Pattern Recognition: Different white dot syndromes have distinct patterns on FA. For example, APMPPE lesions typically exhibit early fluorescence blockage followed by late staining, whereas birdshot chorioretinopathy may be characterized by multiple hyperfluorescent spots corresponding to choroidal lesions.
Indocyanine Green Angiography (ICGA)
Indocyanine green angiography is another imaging technique that is especially useful for observing choroidal circulation. ICGA employs a different dye that fluoresces in the near infrared spectrum, allowing for greater penetration into the choroid.
- Choroidal Involvement: ICGA is particularly useful in conditions with significant choroidal involvement, such as birdshot chorioretinopathy, serpiginous choroiditis, and multifocal choroiditis. This technique can detect occult lesions that are not visible on FA or fundoscopic examination, providing a more complete picture of disease activity.
- Detailed Imaging: ICGA can also aid in the detection of CNV, a common complication in several white dot syndromes. Early detection of CNV is critical for avoiding severe vision loss.
Optical Coherence Tomography (OCT
Optical coherence tomography is a non-invasive imaging technique that produces detailed cross-sectional images of the retina and choroid. OCT is extremely useful in diagnosing and monitoring white dot syndromes because it allows for detailed visualization of retinal layers and the detection of subtle changes.
- Retinal Thickness and Edema: OCT can detect changes in retinal thickness, cystoid macular edema (CME), and disruption of the outer retinal layers, all of which can appear in white dot syndromes. Quantifying these changes over time is critical for assessing treatment response and disease progression.
- Outer Retinal Abnormalities: In conditions such as MEWDS, OCT may show disruption of the ellipsoid zone (formerly known as the inner segment/outer segment junction) in the outer retina. These abnormalities frequently correspond with the location of the white dots observed during clinical examination.
Fundus Autofluorescence (FAF)
Fundus autofluorescence imaging detects the natural fluorescence emitted by lipofuscin, a byproduct of photoreceptor metabolism, in the RPE. FAF can help identify areas of RPE damage or dysfunction, which are common in white dot syndromes.
- Pattern Recognition: Each white dot syndrome produces a unique pattern of autofluorescence. For example, in serpiginous choroiditis, FAF may show a “wave-like” pattern of hypoautofluorescence corresponding to areas of RPE atrophy, whereas in birdshot chorioretinopathy, multiple hypoautofluorescent spots corresponding to choroidal lesions may be visible.
- Monitoring Disease Activity: FAF can be used to track disease progression and response to treatment by recording changes in autofluorescence patterns over time. This is especially important for chronic or recurrent conditions such as birdshot chorioretinopathy and serpiginous choroiditis.
Additional Diagnostic Tests
In some cases, additional diagnostic tests may be required to rule out other conditions that cause similar symptoms or to confirm the diagnosis of a specific white dot syndrome.
- Electroretinography (ERG) measures the retina’s electrical response to light stimuli. This test can help assess the retina’s overall function, especially in conditions such as birdshot chorioretinopathy, which can cause generalized retinal dysfunction.
- Laboratory Testing: Blood tests may be required to rule out infectious or autoimmune causes of retinal inflammation. In the differential diagnosis of white dot syndromes, testing for syphilis, tuberculosis, or other systemic infections may be required.
- Genetic Testing: In conditions such as birdshot chorioretinopathy, which has a strong association with the HLA-A29 allele, genetic testing can help confirm the diagnosis. However, genetic testing is not always performed in cases of white dot syndrome.
White Dot Syndrome Management
The management of white dot syndromes (WDS) is complex and necessitates a tailored approach based on the type of syndrome, severity of symptoms, and presence of complications such as choroidal neovascularization. WDS encompasses a variety of conditions, including acute posterior multifocal placoid pigment epitheliopathy (APMPPE), multifocal choroiditis and panuveitis (MCP), birdshot chorioretinopathy (BCR), multiple evanescent white dot syndrome (MEWDS), punctate inner choroidopathy (PIC), and serpiginous choroiditis (SC), so management strategies must be individualized for each patient.
Corticosteroid Treatment
Corticosteroids are a common treatment for many white dot syndromes, particularly those involving significant inflammation. These medications can be given systemically, locally, or topically, depending on the severity and location of the inflammation.
- Oral Corticosteroids: Systemic corticosteroids, such as prednisone, are frequently used to reduce inflammation in MCP, SC, and BCR. The dosage is typically started at a high level and gradually reduced based on the patient’s response and side effects. Oral corticosteroids are effective at reducing active inflammation and preventing disease progression.
- Intravitreal Corticosteroids: When inflammation is localized or systemic side effects are a concern, intravitreal corticosteroids (such as triamcinolone acetonide) may be used. This method delivers a high concentration of the drug directly to the site of inflammation, resulting in targeted therapy with fewer systemic effects.
- Topical Corticosteroids: For patients with mild anterior uveitis or vitritis caused by WDS, topical corticosteroids in the form of eye drops may be adequate to control inflammation. However, this method is less effective for posterior segment involvement.
Immunosuppressive Therapy
Immunosuppressive agents may be used when corticosteroids alone are insufficient or when long-term steroid use increases the risk of serious side effects. These medications reduce inflammation by suppressing the immune system’s activity.
- Methotrexate, Azathioprine, and Mycophenolate Mofetil: These immunosuppressive agents are commonly used to treat chronic and relapsing forms of WDS, including birdshot chorioretinopathy and serpiginous choroiditis. They can be used as steroid-sparing agents, reducing the need for long-term corticosteroid use and lowering the risk of side effects.
- Biologic Agents: For patients with refractory WDS who do not respond to standard immunosuppressive therapy, biologic agents such as infliximab or adalimumab may be considered. These drugs target specific immune system components, such as TNF-α, to effectively control inflammation. Biologics are especially effective in treating severe cases of MCP and SC.
Treatment of Choroidal Neovascularization (CNV)
CNV is a serious complication of multiple white dot syndromes, including PIC, MCP, and SC. CNV can cause significant and rapid vision loss if not treated promptly. The most common treatment for CNV is anti-vascular endothelial growth factor (anti-VEGF) therapy.
- Anti-VEGF Injections: The standard treatment for CNV associated with WDS is intravitreal injections of anti-VEGF agents like ranibizumab (Lucentis), bevacizumab (Avastin), or aflibercept (Eylea). These medications work by preventing the formation of abnormal blood vessels beneath the retina, which stabilizes or improves vision. Regular monitoring and injections may be required to keep CNV under control.
- Laser Photocoagulation: In some cases, particularly when CNV is distant from the fovea (the central area of the retina responsible for sharp vision), laser photocoagulation may be used to seal off the abnormal blood vessels. However, because anti-VEGF therapy is so effective, this approach is becoming less popular.
Monitoring and Follow-up
Regular monitoring and follow-up are critical components of managing white dot syndrome. Many of these conditions are chronic and relapsing, necessitating ongoing evaluation to detect new or recurring inflammation, assess treatment response, and avoid complications.
- Regular Eye Examinations: Patients with WDS should have their eyes examined on a regular basis, including visual acuity testing, fundus examinations, and imaging studies like OCT and FA. These assessments help to monitor disease activity and guide treatment plan adjustments.
- Patient Education: It is critical to educate patients about recurrence symptoms such as sudden changes in vision, increased floaters, and new scotomas. Early detection and treatment of flare-ups can help to protect the retina and choroid from permanent damage.
Lifestyle and Supportive Measures
In addition to medical treatment, specific lifestyle and supportive measures can help manage white dot syndromes:
- Sun Protection: Patients with WDS, especially those with conditions like SC or aniridia, may benefit from wearing UV-protected sunglasses to reduce light sensitivity and protect their eyes from further damage.
- Low Vision Aids: Magnifiers, special lighting, or adaptive devices can help individuals with significant visual impairment maintain independence and improve their quality of life.
- Support Groups: Connecting with support groups or online communities for people with rare eye conditions can provide emotional support as well as practical advice on how to deal with the daily challenges that come with WDS.
Trusted Resources and Support
Books
- “Ocular Inflammatory Disease: Diagnosis and Treatment” by Ralph D. Levinson
- This comprehensive text provides detailed information on the diagnosis and management of ocular inflammatory diseases, including white dot syndromes. It is an excellent resource for both clinicians and patients seeking to understand these complex conditions.
- “Retinal and Choroidal Manifestations of Selected Systemic Diseases” by J. Fernando Arevalo
- This book offers an in-depth look at the retinal and choroidal manifestations of various systemic diseases, including white dot syndromes. It is a valuable reference for understanding the systemic connections and implications of these ocular conditions.
Organizations
- American Academy of Ophthalmology (AAO)
- The AAO provides extensive resources on eye diseases, including white dot syndromes. Their website offers patient education materials, clinical guidelines, and the latest research updates, making it a trusted source of information for both patients and healthcare professionals.
- National Organization for Rare Disorders (NORD)
- NORD is a leading organization dedicated to providing support and resources for individuals with rare diseases, including white dot syndromes. Their platform offers information on diagnosis, treatment options, and access to patient support services, helping individuals navigate the challenges of living with a rare eye condition.
condition.






