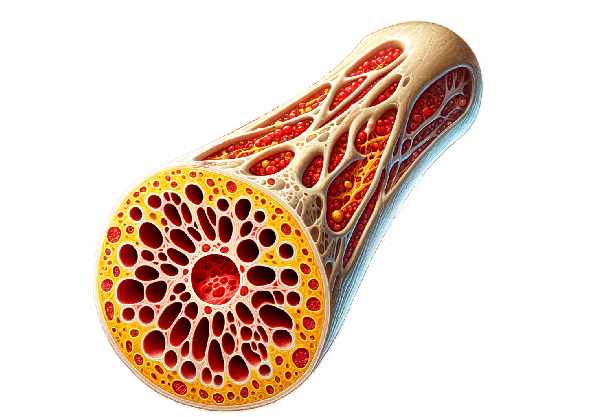
Bone marrow is a dynamic, vital tissue hidden deep within our bones, playing a crucial role in the production of blood cells and supporting immune function. It exists in two forms—red marrow, responsible for hematopoiesis, and yellow marrow, which primarily stores fat. This comprehensive guide explores the intricate anatomy of bone marrow, its key physiological functions, and common disorders that can affect it. We also review current diagnostic techniques, state-of-the-art treatment strategies, and practical nutritional and lifestyle tips to help you maintain optimal bone marrow health.
Table of Contents
- Detailed Bone Marrow Anatomy
- Functional Dynamics and Roles
- Bone Marrow Disorders & Conditions
- Diagnostic Strategies
- Therapeutic Interventions
- Nutritional and Supplementary Support
- Lifestyle and Preventive Measures
- Authoritative Resources
- Frequently Asked Questions
Detailed Bone Marrow Anatomy
Bone marrow is housed within the medullary cavities of bones and is classified into two distinct types—red marrow and yellow marrow—each with unique cellular compositions and functions.
Red Bone Marrow
Red marrow is primarily located in flat bones such as the sternum, pelvis, and ribs, as well as in the epiphyses of long bones in children. It is highly vascular and teems with hematopoietic stem cells (HSCs), which are responsible for generating all blood cell types. These include:
- Erythroid cells that develop into red blood cells (RBCs) for oxygen transport.
- Myeloid cells that mature into various white blood cells (WBCs) and platelets for immune defense and clotting.
- Lymphoid progenitors that contribute to the adaptive immune system by forming B and T lymphocytes.
The red marrow’s supportive stroma is composed of reticular fibers, fibroblasts, and macrophages, which secrete critical cytokines and growth factors to regulate blood cell differentiation and maturation.
Yellow Bone Marrow
Yellow marrow, which predominates in the medullary cavities of long bones in adults, consists mainly of adipocytes (fat cells). Although it appears less active in hematopoiesis, yellow marrow functions as:
- An energy reservoir: The stored fat can be mobilized to support metabolic demands.
- A hematopoietic reserve: Under conditions such as severe blood loss or anemia, yellow marrow can reconvert to red marrow to increase blood cell production.
Microscopic Structure
At the microscopic level, bone marrow is a complex microenvironment:
- Hematopoietic Cells:
These include multipotent stem cells and progenitor cells that give rise to all blood lineages. Their differentiation is tightly regulated by a host of cytokines and growth factors. - Stromal Cells:
Fibroblasts, endothelial cells, and mesenchymal stem cells create a supportive niche (or “niche”) that governs HSC quiescence, self-renewal, and differentiation. - Sinusoids:
Specialized, fenestrated capillaries called sinusoids facilitate the transfer of newly formed blood cells into the circulation. Their porous structure enables cells to exit the marrow with ease.
Vascularization and Innervation
The bone marrow is richly vascularized:
- Arterial Supply:
Nutrient arteries penetrate the cortical bone and branch into smaller arterioles within the marrow cavity, ensuring a robust supply of oxygen and nutrients. - Venous Drainage:
The venous network collects deoxygenated blood and metabolic waste, channeling them into larger veins and ultimately the central circulation. - Innervation:
Both sympathetic and sensory nerve fibers innervate the marrow, regulating blood flow and influencing hematopoietic processes.
Age-Related Changes
During early childhood, most of the marrow is red to support rapid growth and high hematopoietic activity. As individuals age, red marrow gradually converts to yellow marrow in the long bones, reflecting a natural shift towards increased fat storage while preserving hematopoietic activity in flat bones and the axial skeleton.
Understanding the detailed anatomy of bone marrow is fundamental to appreciating its vital role in sustaining life through blood cell production and immune system support.
Functional Dynamics and Roles
Bone marrow is not merely a static tissue; it is a dynamic organ responsible for several essential physiological functions that are critical for maintaining overall health.
Hematopoiesis
Hematopoiesis is the process of blood cell production that occurs primarily in red bone marrow:
- Erythropoiesis:
The formation of red blood cells is triggered by the hormone erythropoietin, primarily produced by the kidneys in response to low oxygen levels. - Leukopoiesis:
White blood cells, vital for immune defense, are produced from both myeloid and lymphoid progenitors. - Thrombopoiesis:
Platelets are formed by the fragmentation of megakaryocytes, large cells that reside in the marrow, and are essential for clotting and wound repair.
The bone marrow’s microenvironment, or niche, is crucial for regulating the balance between quiescence and active proliferation of hematopoietic stem cells.
Immune System Support
Beyond hematopoiesis, bone marrow plays a pivotal role in immune function:
- Lymphopoiesis:
It is the primary site for the development of B lymphocytes, which are essential for antibody production and adaptive immunity. - Myelopoiesis:
The generation of myeloid cells, including neutrophils and monocytes, supports innate immunity and the immediate response to infections. - Cytokine Production:
Stromal cells within the marrow secrete growth factors and cytokines that modulate the immune response, ensuring that the body can respond to infections effectively.
Nutrient and Mineral Storage
Bone marrow also functions as a storage site for essential nutrients:
- Fat Storage:
Yellow marrow serves as an energy reserve by storing lipids, which can be mobilized during periods of increased metabolic demand. - Mineral Metabolism:
The marrow plays a role in iron metabolism by storing iron within macrophages, which is later used in the synthesis of hemoglobin during erythropoiesis.
Response to Physiological Stress
Bone marrow is highly adaptive and can respond dynamically to physiological stress:
- Stress Hematopoiesis:
In response to conditions such as infection, bleeding, or hypoxia, the marrow can rapidly increase the production of specific blood cells to meet heightened demands. - Marrow Plasticity:
Under conditions of severe stress, yellow marrow can reconvert to red marrow to boost hematopoiesis, demonstrating the tissue’s remarkable adaptability.
Integration with Systemic Physiology
Bone marrow is intricately linked to other body systems:
- Endocrine Interactions:
Hormones such as erythropoietin, growth factors, and cytokines influence marrow activity, ensuring a coordinated response to the body’s needs. - Neural Regulation:
Innervation of the marrow by the sympathetic nervous system helps regulate blood flow and may influence hematopoietic processes, integrating marrow function with overall homeostasis.
Overall, the bone marrow is indispensable for the continuous production of blood cells, immune system support, and the storage of essential nutrients. Its ability to adapt to various physiological challenges is fundamental to maintaining health.
Bone Marrow Disorders & Conditions
Disorders of the bone marrow can have profound effects on blood cell production and overall health. Here, we review several common conditions that affect bone marrow function, detailing their pathophysiology, clinical manifestations, and potential complications.
Leukemia
Leukemia is a group of cancers characterized by the uncontrolled proliferation of abnormal blood cells in the bone marrow.
- Acute Leukemia:
- Acute Lymphoblastic Leukemia (ALL): Rapid growth of immature lymphoid cells, most common in children.
- Acute Myeloid Leukemia (AML): Rapid proliferation of myeloid blasts, affecting adults more frequently.
- Symptoms: Fatigue, frequent infections, easy bruising, and bleeding.
- Chronic Leukemia:
- Chronic Lymphocytic Leukemia (CLL): Slow-growing malignancy of mature lymphocytes.
- Chronic Myeloid Leukemia (CML): Characterized by the presence of the Philadelphia chromosome; may present with fatigue and splenomegaly.
Aplastic Anemia
Aplastic anemia is a condition in which the bone marrow fails to produce sufficient blood cells, leading to pancytopenia.
- Etiology:
It can be idiopathic, autoimmune, or due to exposure to toxins, medications, or viral infections. - Symptoms:
Fatigue, increased susceptibility to infections, and easy bruising or bleeding. - Clinical Impact:
This life-threatening condition requires prompt diagnosis and treatment, often including immunosuppressive therapy or bone marrow transplantation.
Myelodysplastic Syndromes (MDS)
MDS encompasses a group of disorders characterized by ineffective hematopoiesis and abnormal cell morphology.
- Pathophysiology:
Abnormal maturation of blood cells in the marrow leads to cytopenias and a high risk of progression to acute myeloid leukemia. - Symptoms:
Anemia, fatigue, and increased vulnerability to infections. - Management:
Treatment may include supportive care, growth factor therapy, or bone marrow transplantation in severe cases.
Multiple Myeloma
Multiple myeloma is a cancer of plasma cells that disrupts the normal bone marrow environment.
- Pathogenesis:
Abnormal plasma cells produce excessive monoclonal proteins, which interfere with normal blood cell production. - Clinical Presentation:
Bone pain, anemia, kidney dysfunction, and recurrent infections. - Treatment:
Options include chemotherapy, targeted therapy, immunomodulatory drugs, and stem cell transplantation.
Bone Marrow Infiltration
Various cancers, such as metastatic breast or prostate cancer, and lymphomas can infiltrate the bone marrow, interfering with its function.
- Manifestations:
Symptoms may include anemia, leukopenia, thrombocytopenia, and bone pain. - Diagnosis and Management:
Bone marrow biopsy is critical for diagnosis, and treatment typically involves systemic chemotherapy or targeted therapies.
Hematophagocytic Lymphohistiocytosis (HLH)
HLH is a severe, life-threatening syndrome characterized by excessive immune activation and subsequent phagocytosis of blood cells by activated macrophages.
- Etiology:
It can be familial or acquired, triggered by infections, malignancies, or autoimmune disorders. - Symptoms:
Persistent fever, hepatosplenomegaly, cytopenias, and coagulopathy. - Treatment:
Aggressive immunosuppressive therapy and supportive care are required to manage this hyperinflammatory state.
Bone Marrow Fibrosis
Bone marrow fibrosis involves the replacement of healthy marrow with fibrous tissue.
- Primary Myelofibrosis:
A chronic disorder that leads to progressive scarring of the marrow, resulting in anemia, splenomegaly, and extramedullary hematopoiesis. - Secondary Fibrosis:
Can occur as a consequence of other chronic conditions, including autoimmune diseases or previous chemotherapy. - Clinical Impact:
Fibrosis impairs normal blood cell production, necessitating supportive care and, in some cases, bone marrow transplantation.
Understanding these disorders is crucial for early diagnosis and intervention, which can significantly improve outcomes and quality of life.
Diagnostic Strategies for Bone Marrow Health
Diagnosing bone marrow disorders requires a comprehensive approach that integrates clinical evaluation, laboratory analysis, imaging studies, and specialized procedures. These methods provide a detailed picture of marrow function and help guide effective treatment.
Bone Marrow Biopsy and Aspiration
- Bone Marrow Biopsy:
A core of marrow tissue is extracted—commonly from the posterior iliac crest—to assess cellularity, morphology, and the presence of fibrosis or infiltrative processes. This procedure is essential for diagnosing conditions such as leukemia, lymphoma, and myelodysplastic syndromes. - Bone Marrow Aspiration:
This process involves drawing a liquid sample of marrow to analyze individual cell characteristics and determine the myeloid-to-erythroid ratio. It is often performed alongside a biopsy for a comprehensive evaluation.
Laboratory Analysis
- Complete Blood Count (CBC):
A CBC provides baseline data on the levels of red cells, white cells, and platelets, which can indicate marrow dysfunction. - Peripheral Blood Smear:
Examination of blood cell morphology can reveal dysplastic features or the presence of blast cells. - Cytogenetic and Molecular Testing:
Techniques like fluorescence in situ hybridization (FISH), PCR, and next-generation sequencing (NGS) are used to identify chromosomal abnormalities and gene mutations associated with marrow disorders. - Flow Cytometry:
This method is used for immunophenotyping, particularly in the evaluation of leukemias and lymphomas, by analyzing the expression of cell surface markers.
Imaging Techniques
- Magnetic Resonance Imaging (MRI):
MRI is particularly useful for detecting marrow infiltration, bone lesions, and changes in marrow composition, which are important in conditions like multiple myeloma. - Positron Emission Tomography (PET/CT):
PET/CT scans assess metabolic activity in the marrow, helping to identify areas of abnormal cellular proliferation, such as in lymphoma or metastatic cancer. - X-rays and CT Scans:
These imaging modalities are employed to evaluate skeletal abnormalities associated with marrow disorders, including lytic or sclerotic lesions.
Functional Tests
- Reticulocyte Count:
Evaluates the bone marrow’s ability to produce new red blood cells and is useful in diagnosing anemias. - Serum Erythropoietin Levels:
These levels can provide insights into the bone marrow’s response to anemia and help differentiate between various causes of low blood cell production.
Integration of Diagnostic Data
Combining clinical findings with laboratory, imaging, and functional test results allows clinicians to accurately diagnose bone marrow conditions and tailor treatment strategies accordingly.
Therapeutic Interventions for Bone Marrow Disorders
Treating bone marrow disorders requires a multifaceted approach, ranging from supportive care to aggressive therapies such as chemotherapy and bone marrow transplantation. Treatment is tailored to the specific disorder, its severity, and the overall health of the patient.
Pharmacological Therapies
- Chemotherapy:
Utilized primarily for treating hematologic malignancies like leukemia and lymphoma, chemotherapy targets rapidly dividing cells, reducing the burden of cancerous cells in the marrow. - Targeted Therapy:
Drugs such as tyrosine kinase inhibitors (e.g., imatinib) are used to target specific molecular abnormalities in certain leukemias, offering a more focused treatment with potentially fewer side effects. - Immunomodulatory Agents:
Medications like thalidomide and lenalidomide are used in multiple myeloma to enhance immune response and inhibit abnormal plasma cell growth. - Growth Factors:
Agents such as erythropoietin (EPO) and granulocyte colony-stimulating factor (G-CSF) stimulate marrow production of red cells and white cells, respectively, supporting recovery from anemia or neutropenia. - Corticosteroids:
Often used in combination with other therapies, corticosteroids help reduce inflammation and can induce apoptosis in certain leukemic cells.
Bone Marrow and Stem Cell Transplantation
- Allogeneic Transplantation:
This procedure involves transferring healthy hematopoietic stem cells from a compatible donor to the patient. It is a critical treatment option for conditions like acute leukemia, aplastic anemia, and high-risk myelodysplastic syndromes. - Autologous Transplantation:
In this procedure, a patient’s own stem cells are harvested before high-dose chemotherapy and later reinfused to restore marrow function, commonly used in multiple myeloma and certain lymphomas.
Innovative and Emerging Therapies
- Chimeric Antigen Receptor (CAR) T-Cell Therapy:
This cutting-edge therapy involves genetically modifying a patient’s T cells to target and destroy malignant cells, showing promise in refractory leukemias and lymphomas. - Gene Therapy:
Although still largely experimental, gene therapy holds potential for correcting genetic defects underlying marrow disorders such as sickle cell anemia and thalassemia. - Monoclonal Antibodies:
These antibodies target specific antigens on malignant cells, aiding in the treatment of conditions like multiple myeloma and certain leukemias.
Supportive Care
- Blood Transfusions:
Transfusions of red blood cells and platelets provide critical support for patients with severe cytopenias. - Infection Prophylaxis:
Antibiotics, antifungals, and antivirals are administered to prevent infections in immunocompromised patients. - Nutritional Support:
Proper nutrition, including vitamin and mineral supplementation, is essential to support overall health during treatment. - Pain and Symptom Management:
Effective pain management and supportive therapies improve quality of life during treatment for chronic marrow disorders.
A personalized treatment plan that integrates these interventions is essential for managing bone marrow disorders and restoring normal blood cell production.
Nutritional & Supplementary Support for Bone Marrow
Optimal bone marrow function depends not only on medical treatments but also on adequate nutrition and supplementation. A targeted approach to dietary support can enhance hematopoiesis, bolster the immune system, and protect marrow cells from oxidative stress.
Key Nutrients
- Iron:
Essential for hemoglobin synthesis, iron is crucial for red blood cell production. Iron deficiency can lead to anemia, undermining marrow function. - Vitamin B12 and Folate:
These vitamins are vital for DNA synthesis and proper blood cell formation. Deficiencies can cause megaloblastic anemia and impaired marrow function. - Vitamin D:
Plays a significant role in immune modulation and supports the bone marrow microenvironment, influencing hematopoiesis. - Omega-3 Fatty Acids:
Found in fish oil, these fatty acids reduce inflammation and support cellular health in the marrow.
Herbal and Natural Supplements
- Echinacea:
Known for its immune-enhancing properties, echinacea may boost white blood cell production and support overall marrow function. - Curcumin (Turmeric Extract):
Curcumin’s potent anti-inflammatory properties can help reduce marrow inflammation and support a healthy microenvironment. - Green Tea Extract:
Rich in antioxidants, green tea extract helps protect marrow cells from oxidative damage and supports cellular energy production. - Coenzyme Q10 (CoQ10):
An essential antioxidant that supports mitochondrial function, CoQ10 helps maintain the energy production necessary for blood cell synthesis.
Dietary Strategies
- Whole Foods Approach:
Emphasize a diet high in fresh fruits, vegetables, lean proteins, and whole grains to supply essential vitamins and minerals. - Consistent Hydration:
Adequate water intake promotes effective nutrient transport and cellular function. - Meal Regularity:
Eating at consistent intervals helps stabilize blood sugar and ensures a steady supply of nutrients to support continuous marrow activity.
Integrating these nutritional and supplementary measures can provide a robust foundation for maintaining bone marrow health and optimizing blood cell production.
Lifestyle and Preventive Measures for Bone Marrow Health
Maintaining healthy bone marrow is not solely about medical treatments—it also involves adopting a lifestyle that supports overall cellular health and immune function.
Healthy Eating Habits
- Balanced Diet:
Focus on nutrient-dense foods rich in iron, B vitamins, and antioxidants to support effective hematopoiesis. - Fiber-Rich Foods:
A high-fiber diet improves digestion and nutrient absorption, contributing to a healthy internal environment. - Proper Hydration:
Consistently drinking water supports blood volume and facilitates the transport of essential nutrients.
Regular Physical Activity
- Moderate Exercise:
Engaging in regular physical activity, such as walking, cycling, or swimming, promotes healthy circulation and overall cellular health. - Strength and Flexibility Training:
These exercises not only support cardiovascular health but also help maintain a strong skeletal system, which is critical for supporting bone marrow function.
Stress Management
- Mindfulness and Meditation:
Techniques like deep breathing, meditation, and yoga help reduce stress hormones that can negatively impact marrow function. - Adequate Sleep:
Aim for 7–9 hours of quality sleep per night to allow the body to repair and regenerate, ensuring optimal marrow performance.
Avoidance of Harmful Substances
- No Smoking:
Smoking impairs oxygen delivery and can adversely affect bone marrow function. - Limit Alcohol Consumption:
Excessive alcohol intake can suppress hematopoiesis and contribute to nutritional deficiencies. - Environmental Toxins:
Minimize exposure to harmful chemicals and pollutants that may damage bone marrow cells.
Regular Medical Monitoring
- Routine Check-Ups:
Regular blood tests and bone marrow assessments can detect early signs of dysfunction and allow for timely intervention. - Nutritional Evaluations:
Periodic assessment of vitamin and mineral levels can guide dietary adjustments and supplementation needs.
By integrating these lifestyle and preventive measures, you can support a healthy bone marrow environment, ensuring robust blood cell production and overall well-being.
Authoritative Resources for Bone Marrow Health
Staying informed about bone marrow health is key to managing and preventing disorders. The following resources offer valuable insights, research updates, and practical advice for both healthcare professionals and individuals.
Recommended Books
- “The Blood Sugar Solution” by Mark Hyman:
This book discusses holistic strategies for improving overall health, including insights relevant to bone marrow function. - “Nutrition and Physical Degeneration” by Weston A. Price:
A classic work exploring the impact of diet on overall health, offering context for maintaining bone marrow vitality. - “The Immune System Recovery Plan” by Susan Blum:
Provides strategies for supporting immune function, with practical tips that can benefit bone marrow health.
Academic Journals
- Blood:
A leading journal in hematology that publishes the latest research on blood cell production, bone marrow disorders, and innovative therapies. - Journal of Hematology & Oncology:
Offers insights into cutting-edge research and clinical trials related to bone marrow health and hematologic malignancies.
Mobile Applications
- MyFitnessPal:
Tracks nutritional intake and exercise, supporting a balanced lifestyle that benefits bone marrow function. - Headspace:
Provides guided meditation and mindfulness exercises to help reduce stress and support overall immune and marrow health. - Blood Pressure Monitor:
Assists in monitoring blood pressure, which indirectly affects overall health and can provide clues about systemic conditions impacting the marrow.
These resources empower you with the latest information and practical tools to manage and optimize bone marrow health.
Frequently Asked Questions
What is the primary function of bone marrow?
Bone marrow is responsible for hematopoiesis—the production of red blood cells, white blood cells, and platelets. It also serves as an energy reserve and plays a role in immune system support.
How does red bone marrow differ from yellow bone marrow?
Red bone marrow is active in blood cell production and is found in flat bones and the ends of long bones, while yellow bone marrow primarily stores fat and can convert to red marrow under conditions of increased hematopoietic demand.
What are common symptoms of bone marrow disorders?
Symptoms may include fatigue, frequent infections, easy bruising or bleeding, bone pain, and anemia. These signs warrant further evaluation through blood tests and bone marrow biopsy.
How is bone marrow health assessed?
Bone marrow health is assessed through biopsies, aspirations, complete blood counts (CBC), and specialized tests like flow cytometry and cytogenetic studies, which evaluate cellular composition and genetic markers.
What lifestyle changes can support bone marrow function?
A balanced diet rich in iron, B vitamins, and antioxidants, regular exercise, proper hydration, stress management, and avoiding harmful substances like tobacco can help maintain optimal bone marrow health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
We encourage you to share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about bone marrow health and empower others with valuable insights!