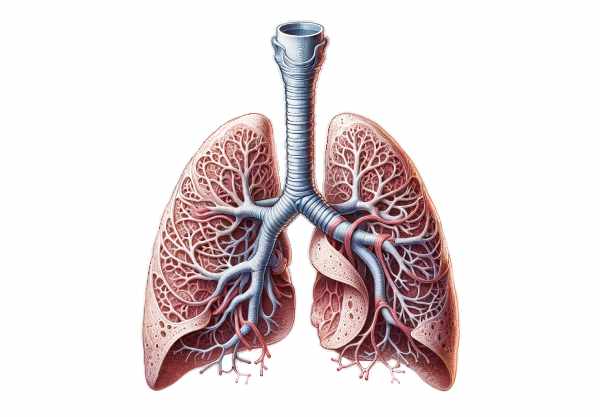
The bronchi play a crucial role in our respiratory system, acting as the primary passageways for air to travel from the trachea into the lungs. These tubular structures not only facilitate effective air distribution but also serve essential functions in filtering, humidifying, and regulating inhaled air. An in-depth understanding of bronchi anatomy, physiology, common disorders, diagnostic methods, treatment modalities, and healthy living practices is vital for maintaining optimal respiratory health. This guide aims to provide a comprehensive review of these aspects while offering practical tips and the latest insights into bronchial care.
Table of Contents
- Anatomical Blueprint and Structural Makeup
- Functional Dynamics and Airflow Mechanics
- Common Disorders Impacting Bronchial Health
- Diagnostic Techniques and Evaluative Methods
- Therapeutic Strategies and Management Options
- Nutritional Support and Supplementary Aids
- Lifestyle Practices for Sustained Bronchial Wellness
- Additional Resources and Reference Materials
- Frequently Asked Questions About Bronchi
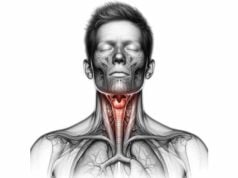
Anatomical Blueprint and Structural Makeup
Understanding the detailed anatomy of the bronchi is fundamental for appreciating their role in respiratory health. The bronchial tree begins at the trachea’s bifurcation and divides into two main branches, each following a distinct anatomical pathway. The right main bronchus is typically shorter, wider, and more vertically oriented than its left counterpart, which is longer and more horizontal. This anatomical variation significantly influences clinical presentations, such as the tendency for foreign bodies to more easily enter the right bronchus.
Main Airway Divisions
Within the primary bronchial architecture, the right bronchus quickly divides to accommodate the three lobes of the right lung, whereas the left splits into two lobar branches corresponding to the left lung’s lobes. These divisions are critical not only for efficient air conduction but also for targeted surgical and diagnostic procedures. Cartilaginous support, provided by C-shaped rings in the larger airways, ensures that the bronchi maintain their patency and resist collapse under various physiological pressures.
Secondary and Tertiary Branching
As the bronchi extend into the lung tissue, they further subdivide into lobar (secondary) and segmental (tertiary) branches. Each segmental bronchus serves a specific bronchopulmonary segment, ensuring a well-distributed airflow that is crucial for gas exchange. This elaborate branching increases the overall surface area, making the respiratory process more efficient. The segmental bronchi also provide surgeons with clear demarcation lines, which is essential during procedures that target specific lung segments.
Wall Architecture and Layers
The bronchial wall is a composite of several layers, each contributing to its overall function:
- Mucosal Layer:
The innermost layer, lined with pseudostratified ciliated columnar epithelium, is interspersed with goblet cells that secrete mucus. This mucus traps particulates and pathogens, while coordinated ciliary movement propels the mucus upward for removal. - Submucosa:
Situated beneath the mucosa, this layer houses seromucous glands that contribute additional moisture and protection to the airway lining. - Muscular Layer:
Surrounding the submucosa is a robust network of smooth muscle fibers that mediate bronchial constriction and dilation. This muscular activity is essential for regulating airflow and adapting to varying respiratory demands. - Cartilage:
In the larger bronchi, hyaline cartilage provides structural rigidity, preventing airway collapse. As the bronchi branch further into smaller passages, the cartilage diminishes, allowing increased flexibility and precise control over airway caliber. - Adventitia:
The outermost layer consists of connective tissue that anchors the bronchi to surrounding structures, ensuring stability within the thoracic cavity.
Vascular and Neural Integration
The bronchi receive a dedicated blood supply through the bronchial arteries, branches of the thoracic aorta, ensuring that the airway tissues remain well oxygenated and metabolically supported. Venous drainage occurs via the bronchial veins, which connect to larger systemic venous pathways. In parallel, autonomic innervation from both the sympathetic and parasympathetic nervous systems governs bronchial tone and secretory activity. This intricate network of nerves ensures rapid adjustments to changing respiratory demands, such as during exercise or in response to environmental irritants.
Lymphatic Channels and Immune Surveillance
Lymphatic vessels distributed within the bronchial walls play a critical role in immune surveillance. They facilitate the transport of immune cells to regional lymph nodes, such as the bronchopulmonary and tracheobronchial nodes. This process is vital for initiating immune responses to inhaled pathogens and helps maintain the delicate balance between defense mechanisms and tissue homeostasis.
In summary, the anatomical complexity of the bronchi—from their primary divisions to the intricate wall structures—underscores their importance in respiratory physiology. A detailed understanding of bronchial anatomy not only aids clinicians in diagnosing and managing respiratory diseases but also provides valuable insights for researchers aiming to develop innovative treatments for bronchial disorders.
Functional Dynamics and Airflow Mechanics
The bronchi are far more than simple air conduits; they play an active role in ensuring optimal respiratory function. Their dynamic physiology encompasses multiple processes that work in concert to support effective gas exchange and protect the respiratory tract from environmental hazards.
Efficient Air Conduction
At its core, the primary function of the bronchi is to transport air from the external environment deep into the lungs. The extensive branching network ensures that air is distributed evenly throughout the alveoli, maximizing the surface area available for oxygen and carbon dioxide exchange. As air travels through these channels, its movement is carefully modulated by the structure of the bronchial tree, ensuring that even the most peripheral lung regions receive sufficient airflow.
Airway Defense Mechanisms
The bronchi are equipped with a robust defense system designed to neutralize harmful particles and pathogens. The mucociliary escalator is central to this mechanism. Goblet cells produce a viscous mucus that adheres to dust, bacteria, and other irritants, while the cilia beat rhythmically to propel this mucus upward toward the pharynx. This continuous clearance process is essential for maintaining clean air passages and preventing infections, thereby contributing significantly to overall respiratory health.
Humidification and Thermal Regulation
As air moves through the bronchial passages, it is simultaneously warmed and humidified. The bronchial blood vessels supply heat, ensuring that the temperature of the inhaled air approaches body temperature by the time it reaches the alveoli. Moisture provided by the mucosal lining further prevents the desiccation of delicate lung tissues. This humidification process is vital not only for protecting the alveoli from injury but also for facilitating the optimal exchange of respiratory gases.
Regulation of Airflow
The smooth muscle fibers embedded within the bronchial walls play a pivotal role in modulating airway diameter. Under the influence of the autonomic nervous system, these muscles can contract or relax, thereby controlling the resistance to airflow. During instances of bronchoconstriction—triggered by allergens, irritants, or cold air—the airway narrows, reducing airflow. Conversely, during bronchodilation, the muscles relax, widening the airway and promoting easier passage of air. This regulatory mechanism is crucial for adapting to varying physiological states, such as during physical exertion or rest.
Immunological Contributions
Beyond their mechanical functions, the bronchi are active participants in the body’s immune response. Specialized immune cells reside within the bronchial mucosa, ready to respond to pathogenic invasions. These include macrophages, dendritic cells, and lymphocytes, which work collectively to identify and eliminate potential threats. Moreover, the presence of bronchial-associated lymphoid tissue (BALT) further enhances local immune defenses by producing antibodies tailored to neutralize specific antigens encountered in the airways.
Synergy with the Pulmonary System
Although the bronchi themselves do not directly participate in the gas exchange process, their proper functioning is critical to ensure that oxygen-rich air reaches the alveoli. A seamless integration with the vascular system facilitates the swift transfer of oxygen into the bloodstream while simultaneously removing carbon dioxide. Additionally, the interplay between the bronchi and other systems, such as the cardiovascular and nervous systems, ensures that respiratory function adapts dynamically to meet the body’s metabolic demands.
Adaptive Responses and Homeostasis
The bronchi demonstrate remarkable adaptability in response to environmental and physiological changes. In the face of irritants, the bronchial walls may thicken or increase mucus production as protective measures. Conversely, during periods of low exposure to harmful agents, the airways maintain a state of minimal resistance to maximize airflow efficiency. These adaptive responses are critical for maintaining homeostasis and preventing chronic respiratory conditions.
In essence, the functional dynamics of the bronchi encompass a blend of mechanical, immunological, and regulatory processes that collectively support respiratory efficiency. By ensuring that air is properly conditioned, evenly distributed, and rapidly cleared of contaminants, the bronchi play a central role in preserving lung health and overall well-being.
Common Disorders Impacting Bronchial Health
A variety of conditions can impair bronchial function and compromise respiratory health. Understanding these disorders—from their etiology and clinical manifestations to their management strategies—is critical for both healthcare professionals and patients alike. This section provides a detailed exploration of the most common bronchial conditions and their implications.
Inflammatory Bronchitis
Bronchitis, which can manifest as either an acute or chronic condition, is characterized by the inflammation of the bronchial tubes. Acute bronchitis is usually triggered by viral infections and presents with symptoms such as coughing, mucus production, and mild wheezing. Chronic bronchitis, a subset of chronic obstructive pulmonary disease (COPD), is marked by a prolonged, productive cough and persistent mucus hypersecretion. Common risk factors include smoking, prolonged exposure to environmental pollutants, and recurrent respiratory infections. Management typically involves symptomatic relief, avoidance of triggers, and in some cases, the use of bronchodilators and anti-inflammatory medications.
Asthmatic Manifestations
Asthma is a chronic respiratory disorder characterized by airway hyperresponsiveness, intermittent bronchoconstriction, and inflammation. Patients with asthma often experience episodic wheezing, chest tightness, shortness of breath, and coughing. These symptoms may be triggered by allergens, respiratory infections, exercise, or environmental irritants. The management of asthma centers on the avoidance of known triggers, the use of bronchodilators (both short- and long-acting), and inhaled corticosteroids to reduce inflammation. An individualized asthma action plan is essential for effective long-term management and reducing the frequency of exacerbations.
Bronchiectasis and Airway Dilation
Bronchiectasis involves the permanent dilation and destruction of the bronchial walls, often resulting from chronic infections or an underlying impairment in mucociliary clearance. This condition leads to a cycle of infection and inflammation, resulting in symptoms such as chronic cough, excessive sputum production, and recurrent respiratory infections. Management strategies include aggressive airway clearance techniques, prolonged courses of antibiotics to combat infections, and, in severe cases, surgical intervention to remove severely affected lung segments.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive respiratory disorder that encompasses both chronic bronchitis and emphysema. Patients with COPD typically present with a chronic cough, sputum production, and exertional dyspnea. The inflammatory processes underlying COPD lead to structural changes in the bronchi, including airway narrowing and mucus hypersecretion. Smoking is the primary risk factor, with environmental pollutants further contributing to disease progression. Treatment strategies involve smoking cessation, pharmacotherapy with bronchodilators and inhaled corticosteroids, pulmonary rehabilitation, and oxygen therapy in advanced cases.
Bronchial Tumors and Neoplastic Conditions
Bronchial carcinoid tumors, although relatively rare, are slow-growing neuroendocrine tumors that can develop within the bronchial tree. They may present with non-specific symptoms such as coughing, wheezing, or hemoptysis (coughing up blood). The diagnosis is often confirmed through imaging and biopsy, with surgical resection being the treatment of choice. The prognosis largely depends on the size, location, and presence of metastatic spread. Early detection and intervention are crucial to improve outcomes in patients with bronchial neoplasms.
Foreign Body Obstruction
Accidental inhalation of foreign objects can lead to partial or complete airway obstruction, triggering a range of symptoms from coughing and wheezing to severe respiratory distress. Children and elderly individuals are particularly vulnerable to foreign body aspiration. Prompt diagnosis, typically via imaging or bronchoscopy, is critical for timely removal and to prevent subsequent complications such as pneumonia or localized bronchiectasis.
Genetic Disorders Affecting Bronchi
Cystic fibrosis is a genetic disorder that significantly impacts bronchial function. The disease is characterized by the production of abnormally thick and sticky mucus, which obstructs the airways and predisposes patients to chronic infections. Individuals with cystic fibrosis often suffer from persistent coughing, recurrent lung infections, and progressive respiratory decline. Management involves aggressive airway clearance, the use of mucolytic agents, antimicrobial therapy, and, in some cases, lung transplantation to manage end-stage disease.
Overall, a clear understanding of these disorders and their underlying mechanisms is essential for early diagnosis and effective management. With advancements in medical research and therapeutic interventions, many of these conditions can now be managed more effectively, leading to improved quality of life and better respiratory outcomes.
Diagnostic Techniques and Evaluative Methods
Accurate diagnosis of bronchial disorders is crucial for effective treatment and long-term management. A multifaceted approach that combines clinical assessments, imaging studies, functional tests, and advanced diagnostic procedures is often required to achieve a precise diagnosis.
Clinical Assessment and History Taking
The initial evaluation of bronchial conditions begins with a comprehensive patient history and physical examination. Clinicians gather detailed information on symptom onset, duration, and severity. Important clinical features such as chronic cough, sputum production, wheezing, and dyspnea are carefully noted. Risk factors, including a history of smoking or exposure to pollutants, are also recorded. Auscultation with a stethoscope allows physicians to detect abnormal lung sounds, such as wheezes or crackles, which may suggest airway obstruction or inflammation.
Pulmonary Function Testing
Pulmonary function tests (PFTs) are indispensable in assessing bronchial health. Spirometry is the cornerstone of PFTs and measures key metrics like Forced Expiratory Volume in One Second (FEV₁) and Forced Vital Capacity (FVC). These tests help quantify the degree of airway obstruction and assess response to bronchodilator therapy. Additionally, bronchial provocation tests may be performed to evaluate airway hyperresponsiveness, particularly in suspected cases of asthma.
Imaging Modalities
Imaging studies provide visual insights into the structural integrity of the bronchi:
- Chest X-rays:
A fundamental imaging technique that can reveal gross structural abnormalities, areas of consolidation, and signs of chronic lung disease. - Computed Tomography (CT) Scans:
High-resolution CT scans offer detailed cross-sectional images of the bronchial tree and lung parenchyma. They are particularly useful for identifying bronchiectasis, neoplasms, and subtle inflammatory changes. - Magnetic Resonance Imaging (MRI):
Although less common for bronchial evaluation, MRI offers excellent soft-tissue contrast without radiation exposure, making it an alternative in specific clinical scenarios such as the evaluation of bronchial tumors.
Bronchoscopic Examination
Bronchoscopy is a minimally invasive procedure that allows direct visualization of the airways. Through the use of either flexible or rigid bronchoscopes, clinicians can inspect the bronchial mucosa for signs of inflammation, obstruction, or neoplastic changes. The procedure also facilitates tissue biopsy, which is critical for histopathological diagnosis. In addition, bronchoalveolar lavage (BAL) performed during bronchoscopy can collect cellular and microbiological samples, aiding in the diagnosis of infections and inflammatory disorders.
Laboratory Investigations
Laboratory tests further support the diagnostic process. Sputum analysis enables the identification of infectious agents, inflammatory cells, and, in some cases, malignant cells. Blood tests may be conducted to evaluate inflammatory markers, immune response parameters, and specific antibodies. These tests, in conjunction with imaging and functional studies, help form a comprehensive picture of bronchial health.
Advanced Diagnostic Techniques
In complex or ambiguous cases, advanced techniques such as Positron Emission Tomography (PET) scans and Endobronchial Ultrasound (EBUS) have become invaluable. PET scans, often combined with CT (PET-CT), assess metabolic activity within bronchial tissues, facilitating the detection and staging of neoplastic processes. EBUS, which integrates ultrasound with bronchoscopy, allows for the evaluation of mediastinal and hilar lymph nodes, providing critical information in cases of suspected lung cancer or granulomatous diseases.
The integration of these diagnostic methods not only enables early detection of bronchial disorders but also informs treatment decisions and long-term management plans. As technological advancements continue to evolve, diagnostic accuracy improves, leading to more tailored and effective therapeutic strategies for bronchial conditions.
Therapeutic Strategies and Management Options
Managing bronchial disorders requires a comprehensive and personalized approach. Treatment modalities range from pharmacological interventions to advanced surgical procedures and innovative therapies. The choice of treatment depends on the specific condition, its severity, and the overall health of the patient.
Pharmacological Interventions
Bronchodilators are the first line of defense in treating conditions like asthma and COPD.
- Short-acting beta-agonists (SABAs), such as albuterol, offer rapid relief by relaxing the smooth muscle and easing bronchoconstriction.
- Long-acting beta-agonists (LABAs) provide extended relief and are often used in combination with inhaled corticosteroids for long-term management.
Corticosteroids play a central role in reducing airway inflammation.
- Inhaled corticosteroids (ICS) are the mainstay for controlling chronic inflammation in asthma, while systemic corticosteroids may be reserved for severe exacerbations.
- Anticholinergics reduce bronchial constriction and decrease mucus production, proving particularly beneficial in COPD management.
Leukotriene modifiers and biologic agents offer targeted therapy for patients with specific inflammatory profiles, helping to reduce exacerbation frequency and improve overall lung function.
Non-Pharmacological and Supportive Therapies
Beyond medications, non-pharmacological approaches are essential for optimizing bronchial health. Pulmonary rehabilitation programs combine exercise, education, and behavioral strategies to enhance lung function and overall well-being. Oxygen therapy is vital for patients with advanced respiratory compromise, improving oxygen saturation and reducing dyspnea during daily activities.
Surgical and Interventional Procedures
For cases unresponsive to conventional treatments, surgical intervention may be warranted. Bronchial thermoplasty, a minimally invasive procedure, reduces airway smooth muscle mass using controlled thermal energy, thereby diminishing bronchoconstriction. Endobronchial valve placement offers relief for patients with emphysema by redirecting airflow away from diseased lung areas. In instances of localized disease or bronchiectasis, surgical resection may be necessary to remove the affected tissue, while lung transplantation remains an option for end-stage disease.
Cutting-Edge and Innovative Approaches
The field of respiratory medicine is rapidly advancing with emerging therapies:
- Gene therapy is under investigation as a means to correct the genetic defects underlying conditions like cystic fibrosis.
- Regenerative medicine, including stem cell therapy, shows promise in repairing and regenerating damaged bronchial tissues.
- Telemedicine and digital health platforms are increasingly being used to monitor chronic respiratory conditions, enabling real-time interventions and enhancing patient engagement through remote management strategies.
By integrating a variety of treatment options—ranging from traditional pharmacotherapy to the latest in innovative research—healthcare providers can tailor interventions to meet the individual needs of patients, ultimately improving bronchial function and quality of life.
Nutritional Support and Supplementary Aids
Nutrition plays a critical role in supporting respiratory health. The right balance of vitamins, minerals, and supplements can help reduce inflammation, boost immune function, and enhance the overall health of the bronchi.
Essential Vitamins and Nutrients
Vitamin D is known to support immune function and may help reduce airway inflammation. Adequate levels of vitamin D can contribute to better respiratory health and reduce the frequency of infections.
Vitamin C is a potent antioxidant that can mitigate oxidative stress in bronchial tissues, potentially reducing the severity and duration of respiratory infections.
Omega-3 Fatty Acids, commonly found in fish oil, possess anti-inflammatory properties that can be particularly beneficial for patients with chronic bronchial inflammation.
Herbal and Natural Supplements
Certain herbal supplements have long been used to support bronchial health. Echinacea is believed to enhance the body’s immune response, although research results remain mixed. Licorice root is traditionally used for its soothing effects on inflamed airways and its role as an expectorant, facilitating the clearance of mucus from the respiratory tract.
Enzymatic and Antioxidant Agents
N-acetylcysteine (NAC) serves as a mucolytic agent by breaking down mucus, thus enhancing expectoration. Its antioxidant properties further protect the bronchi from oxidative damage. Coenzyme Q10 (CoQ10), essential for cellular energy production, also acts as an antioxidant, supporting overall respiratory function and reducing oxidative stress.
Hormonal Influences
Melatonin, beyond its role in regulating sleep cycles, exhibits antioxidant properties that can help protect bronchial tissues. Its use may be particularly beneficial in managing inflammation in certain respiratory conditions, contributing to better bronchial health.
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains, combined with targeted nutritional supplements, can provide the necessary support for maintaining healthy bronchi. These nutritional strategies not only contribute to improved respiratory function but also enhance the body’s resilience against environmental and pathogenic challenges.
Lifestyle Practices for Sustained Bronchial Wellness
Long-term bronchial health is not solely dependent on medical interventions; everyday lifestyle choices have a profound impact on respiratory well-being. Adopting practical habits can significantly reduce the risk of bronchial disorders and promote optimal lung function.
Smoking Cessation and Environmental Awareness
Smoking remains the single most significant risk factor for bronchial diseases. Quitting smoking is paramount for preventing chronic bronchitis, COPD, and other respiratory conditions. Additionally, reducing exposure to environmental pollutants—such as industrial emissions, vehicle exhaust, and indoor allergens—can help minimize bronchial irritation and inflammation.
Hydration and Airway Moisturization
Staying well-hydrated is essential for maintaining the optimal viscosity of mucus, which in turn facilitates the effective clearance of irritants and pathogens. Drinking adequate water daily ensures that the mucosal lining remains moist, reducing the risk of irritation and helping to sustain airway function.
Regular Physical Activity
Engaging in regular exercise strengthens respiratory muscles and enhances overall lung capacity. Activities such as walking, jogging, and aerobic workouts not only improve cardiovascular health but also promote better ventilation and gas exchange. Exercise can help reduce the frequency of respiratory symptoms and improve the overall quality of life.
Nutritious Diet and Immune Support
A well-balanced diet rich in antioxidants, vitamins, and minerals supports immune function and helps reduce inflammation. Incorporating fresh fruits, vegetables, whole grains, and lean proteins into daily meals provides the essential nutrients that support bronchial health. Omega-3 fatty acids, in particular, play a significant role in curbing inflammation and maintaining clear airways.
Home Environment and Allergen Management
Maintaining a clean home environment, using air purifiers, and regularly cleaning air ducts and filters can minimize exposure to dust, mold, and allergens. The use of humidifiers during dry weather can help maintain moisture in the air, preventing the bronchial lining from becoming dry and irritated.
Preventive Health Practices
Regular vaccinations against influenza and pneumonia, as well as routine health check-ups, are crucial for preventing infections that could compromise bronchial health. Managing allergies through appropriate medications and avoiding known triggers further supports respiratory function.
Incorporating these lifestyle practices into daily routines not only enhances bronchial health but also contributes to overall wellness. The combination of healthy habits, nutritional support, and preventive measures creates a robust foundation for sustained respiratory function and improved quality of life.
Additional Resources and Reference Materials
Staying informed and accessing quality resources is essential for both patients and healthcare professionals. A variety of reputable books, academic journals, and digital tools are available to deepen one’s understanding of bronchial health and support ongoing education.
Recommended Books
Several authoritative texts provide in-depth insights into respiratory anatomy, physiology, and pathology:
- “The Respiratory System at a Glance” offers an accessible yet detailed overview of lung structure and function.
- “Respiratory Physiology: The Essentials” delves into the mechanics of breathing and the role of the bronchi in gas exchange.
- “Principles of Pulmonary Medicine” covers a comprehensive range of topics, including diagnostic techniques and treatment strategies for bronchial disorders.
Scholarly Journals
For those seeking cutting-edge research and clinical updates, academic journals are indispensable:
- The American Journal of Respiratory and Critical Care Medicine publishes peer-reviewed studies on respiratory diseases and novel therapeutic approaches.
- Chest is another respected journal that provides in-depth reviews and clinical insights into bronchial conditions and treatments.
Digital and Mobile Applications
Modern technology offers numerous tools to monitor and manage bronchial health:
- MyAsthma helps patients track symptoms, medication usage, and triggers, thereby supporting personalized asthma management.
- Breathing Zone provides guided breathing exercises that enhance lung capacity and reduce stress.
- Lung Health Check offers easy access to lung function tests and health tips, enabling users to monitor their respiratory well-being on the go.
These resources not only serve as educational tools but also empower individuals to take proactive steps in managing their respiratory health. Whether you are a patient seeking information or a healthcare provider aiming to stay updated, these books, journals, and digital apps can serve as invaluable assets in the journey toward optimal bronchial function.
Frequently Asked Questions About Bronchi
What role do the bronchi play in respiration?
The bronchi are essential air passageways that conduct air from the trachea to the lungs, facilitating proper gas exchange. They also filter, humidify, and warm inhaled air, ensuring that oxygen reaches the alveoli in optimal condition.
How does the structure of the bronchi support their function?
The bronchi’s structure—comprising multiple layers like mucosa, smooth muscle, and cartilage—maintains airway patency and flexibility. This design allows for efficient air distribution, protection against pathogens, and adaptation to varying respiratory demands.
What are common conditions that affect the bronchi?
Common bronchial disorders include bronchitis, asthma, bronchiectasis, COPD, and less common conditions such as bronchial carcinoid tumors. These conditions may cause inflammation, airway obstruction, and impaired respiratory function.
How are bronchial disorders diagnosed?
Diagnosis involves a combination of clinical evaluation, pulmonary function tests, imaging studies (X-ray, CT scan, MRI), bronchoscopy, and laboratory tests. Advanced techniques like PET scans and EBUS can further refine the diagnosis in complex cases.
What lifestyle changes can help maintain bronchial health?
Key practices include smoking cessation, regular exercise, maintaining hydration, a balanced diet, proper allergen management, and routine vaccinations. These measures help reduce inflammation, improve airflow, and protect against infections.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered as a substitute for professional medical advice. Always consult with a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about bronchial health and wellness.