Neurotrophic keratopathy is a debilitating eye condition characterized by impaired corneal sensation, leading to corneal ulcers, scarring, and potential vision loss. Traditional treatments focus on managing symptoms and preventing complications, but Corneal Neurotization Surgery has emerged as a groundbreaking FDA-approved procedure aimed at restoring corneal sensation and promoting healing. By re-establishing nerve connections to the cornea, corneal neurotization offers a transformative approach to managing neurotrophic keratopathy. This article explores the intricacies of corneal neurotization surgery, including its mechanisms, treatment protocols, effectiveness, safety, current research, and accessibility.
Introduction to Corneal Neurotization Surgery: A New Frontier in Neurotrophic Keratopathy Treatment
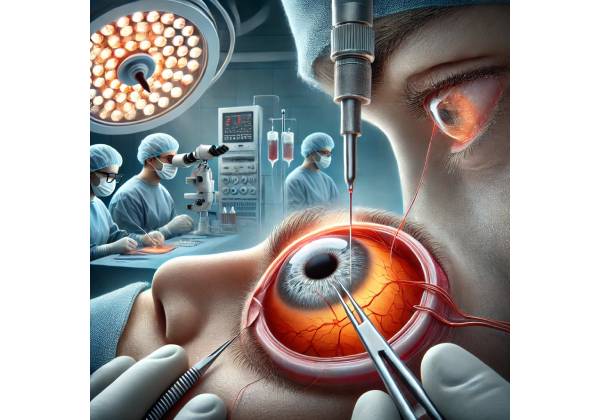
Corneal Neurotization Surgery is an innovative ophthalmic procedure designed to restore corneal sensation in patients suffering from neurotrophic keratopathy. Unlike conventional treatments that primarily address the symptoms, corneal neurotization targets the underlying neural deficits by reconnecting nerves to the cornea, thereby promoting natural healing and preventing further deterioration.
The Evolution of Corneal Neurotization
Historically, the management of neurotrophic keratopathy involved conservative measures such as lubricating eye drops, therapeutic contact lenses, and, in severe cases, surgical interventions like amniotic membrane transplantation or tarsorrhaphy (partial eyelid closure). While these treatments can alleviate symptoms and promote healing, they do not address the root cause—the lack of corneal innervation.
Corneal neurotization represents a significant advancement in ophthalmology by focusing on nerve regeneration. This surgical technique re-establishes neural connections between the cornea and healthy donor nerves from other parts of the body, effectively restoring corneal sensitivity and facilitating long-term corneal health.
Benefits of Corneal Neurotization
- Restoration of Corneal Sensation: Reestablishes nerve function, enhancing the cornea’s ability to respond to stimuli.
- Promotion of Natural Healing: Encourages the cornea to heal itself by restoring its innate protective mechanisms.
- Prevention of Corneal Ulcers and Scarring: Reduces the risk of recurrent corneal damage by maintaining corneal integrity.
- Improved Quality of Life: Enhances visual function and reduces the psychological burden associated with chronic eye conditions.
Corneal neurotization stands out as a revolutionary treatment option, offering comprehensive benefits that extend beyond symptom management to address the fundamental causes of neurotrophic keratopathy.
Exploring Neurotrophic Keratopathy: Causes, Symptoms, and Daily Impact
Neurotrophic keratopathy is a rare but serious eye condition resulting from impaired corneal innervation. The cornea, being one of the most densely innervated tissues in the body, relies on its nerve supply to maintain its health and function. Disruption of these nerves leads to decreased corneal sensation, compromised healing, and increased vulnerability to injury and infection.
Causes of Neurotrophic Keratopathy
Several factors can lead to the development of neurotrophic keratopathy:
- Herpes Zoster Ophthalmicus: Reactivation of the varicella-zoster virus affecting the ophthalmic branch of the trigeminal nerve.
- Diabetic Neuropathy: High blood sugar levels can damage peripheral nerves, including those supplying the cornea.
- Surgery-Related Nerve Damage: Procedures such as glaucoma surgery or facial trauma can inadvertently damage corneal nerves.
- Multiple Sclerosis: An autoimmune disease that can affect the nervous system, including corneal innervation.
- Trigeminal Nerve Injuries: Trauma or surgical interventions involving the trigeminal nerve can disrupt corneal sensation.
Recognizing the Symptoms
Neurotrophic keratopathy progresses through three stages, each with distinct clinical features:
- Stage 1: Mild Nerve Damage
- Decreased Corneal Sensation: Reduced ability to feel sensations in the cornea.
- Epithelial Changes: Development of superficial punctate keratitis (small, scattered corneal epithelial defects).
- Stage 2: Moderate Nerve Damage
- Persistent Epithelial Defects: Non-healing corneal abrasions or epithelial erosions.
- Bullous Keratopathy: Formation of blisters on the corneal surface due to fluid accumulation.
- Stage 3: Severe Nerve Damage
- Corneal Ulcers: Deep, persistent ulcers that may lead to corneal melting and perforation.
- Scarring: Fibrous scar tissue formation that can significantly impair vision.
Impact on Daily Life
The progression of neurotrophic keratopathy can have profound effects on an individual’s quality of life:
- Visual Impairment: Blurred or distorted vision hampers daily activities such as reading, driving, and recognizing faces.
- Pain and Discomfort: Although patients may not always feel pain due to reduced sensation, the presence of corneal damage can cause significant discomfort.
- Increased Risk of Infections: Damaged corneal tissue is more susceptible to bacterial and fungal infections.
- Psychological Burden: Chronic eye conditions can lead to anxiety, depression, and a decreased sense of well-being.
- Economic Strain: Ongoing medical treatments, potential loss of employment, and the need for assistive devices can impose financial challenges.
Understanding the multifaceted impact of neurotrophic keratopathy underscores the critical need for effective treatments like corneal neurotization that address both the symptoms and underlying causes of the condition.
The Science Behind Corneal Neurotization: How It Restores Corneal Sensation
Corneal Neurotization Surgery is a sophisticated procedure aimed at restoring the nerve supply to the cornea, thereby reinstating its sensory functions. The success of this therapy hinges on its ability to re-establish neural pathways, promoting natural healing and enhancing corneal health.
Reconnecting the Nerves: The Surgical Process
Corneal neurotization involves transferring healthy nerves from a donor site to the affected cornea. The most commonly used donor nerves are branches of the supratrochlear or supraorbital nerves, which are accessible and provide robust innervation.
- Donor Nerve Harvesting: Nerves are carefully harvested from the donor site, typically the forehead area, ensuring minimal functional disruption.
- Nerve Grafting: The harvested nerves are then grafted onto the affected cornea, establishing new neural connections.
- Microsurgical Techniques: Precision microsurgery ensures that the grafted nerves integrate seamlessly with the existing corneal tissue, promoting effective nerve regeneration.
Promoting Nerve Regeneration
The success of corneal neurotization relies on several biological mechanisms that facilitate nerve regeneration:
- Axonal Growth Factors: The surgical environment is optimized to release growth factors that encourage axonal sprouting and nerve extension.
- Neural Guidance Cues: Scaffolds or conduits may be used to direct the growth of new nerve fibers towards the cornea.
- Cellular Environment: Maintaining a supportive cellular environment through the use of anti-inflammatory agents and neurotrophic factors enhances nerve integration and function.
Enhancing Corneal Health
By restoring corneal sensation, corneal neurotization promotes several beneficial outcomes:
- Improved Healing: Sensory feedback from the cornea stimulates epithelial cell proliferation and migration, enhancing corneal healing processes.
- Reduced Inflammation: Proper nerve function helps regulate inflammatory responses, preventing excessive scarring and corneal melting.
- Enhanced Barrier Function: Sensory nerves play a role in maintaining the corneal barrier, protecting against pathogens and environmental insults.
Long-Term Benefits
Successful corneal neurotization leads to:
- Sustained Corneal Sensation: Restored nerve function ensures ongoing corneal sensitivity, preventing future erosions and ulcers.
- Vision Preservation: Stabilizing corneal health prevents further visual deterioration, maintaining quality of life.
- Reduced Dependency on External Treatments: Enhanced natural healing reduces the need for frequent medical interventions and therapeutic contact lenses.
Understanding the intricate mechanisms behind corneal neurotization highlights its potential as a definitive treatment for neurotrophic keratopathy, offering lasting solutions for patients seeking to restore their vision and corneal health.
Corneal Neurotization Surgery: Step-by-Step Treatment Protocols
Implementing Corneal Neurotization Surgery requires meticulous planning and execution to ensure optimal outcomes. This section outlines the standard treatment protocols, variations, and key considerations involved in administering corneal neurotization for neurotrophic keratopathy.
Pre-Surgical Assessment
Before proceeding with corneal neurotization, a comprehensive evaluation is essential:
- Detailed Eye Examination: Assessing corneal thickness, topography, and overall ocular health to determine the extent of neurotrophic keratopathy.
- Nerve Function Testing: Evaluating corneal sensation using devices like esthesiometers to quantify nerve impairment.
- Medical History Review: Identifying underlying conditions, previous ocular surgeries, and potential contraindications to ensure patient suitability.
- Imaging Studies: Utilizing Optical Coherence Tomography (OCT) and other imaging modalities to visualize corneal structure and nerve integrity.
The Surgical Procedure
Corneal neurotization is typically performed in a specialized surgical setting, often involving a multidisciplinary team of ophthalmologists and neurosurgeons. The procedure can be broken down into several key steps:
- Anesthesia:
- General or Regional Anesthesia: Depending on the patient’s condition and the surgeon’s preference, anesthesia is administered to ensure patient comfort during the procedure.
- Donor Nerve Harvesting:
- Selection of Donor Site: Common donor sites include the supratrochlear or supraorbital nerves in the forehead.
- Nerve Harvesting: Using microsurgical techniques, the selected nerves are carefully harvested to minimize functional loss at the donor site.
- Preparation of the Recipient Site:
- Corneal Access: Creating an opening or conduit in the cornea to facilitate nerve integration.
- Cleaning and Conditioning: Preparing the corneal tissue to receive the grafted nerves, ensuring a conducive environment for nerve growth.
- Nerve Grafting and Anastomosis:
- Grafting: The harvested nerves are grafted onto the prepared corneal site.
- Microsurgical Anastomosis: Precise connections are made between the donor nerves and corneal nerves to ensure successful integration and function.
- Post-Surgical Closure:
- Sealing the Cornea: Ensuring that the corneal opening is adequately sealed to prevent infection and promote healing.
- Placement of Protective Devices: Using bandage contact lenses or protective shields to safeguard the cornea during the initial healing phase.
Post-Operative Care
Effective post-surgical care is crucial for the success of corneal neurotization:
- Medication Regimen:
- Antibiotic Drops: Preventing infections during the healing process.
- Anti-Inflammatory Agents: Reducing inflammation and promoting a favorable healing environment.
- Lubricating Drops: Maintaining corneal hydration and comfort.
- Monitoring and Follow-Up:
- Regular Eye Exams: Assessing corneal healing, nerve regeneration, and visual acuity.
- Sensory Testing: Tracking the restoration of corneal sensation over time.
- Imaging Studies: Utilizing OCT and other imaging techniques to visualize nerve integration and corneal structure.
- Lifestyle Adjustments:
- Avoiding Eye Rubbing: Preventing mechanical disruption of the healing cornea.
- Protective Eyewear: Wearing sunglasses or protective shields to safeguard the eyes from environmental insults.
Variations in Treatment Protocols
While the core procedure of corneal neurotization remains consistent, several variations aim to optimize outcomes:
- Epi-On vs. Epi-Off Approaches: Similar to other corneal procedures, variations in epithelial management can influence healing times and patient comfort.
- Accelerated Nerve Integration: Employing techniques or adjunct therapies that promote faster nerve regeneration and integration.
- Customized Grafting Techniques: Tailoring nerve grafting methods based on individual corneal topography and nerve distribution patterns.
Patient Education and Compliance
Educating patients on post-operative care and the importance of adherence to treatment protocols enhances the success rates of corneal neurotization:
- Understanding the Procedure: Providing detailed explanations of the surgical process, expected outcomes, and potential risks.
- Post-Operative Instructions: Clear guidelines on medication use, eye care, and activity restrictions to support healing.
- Support Systems: Offering access to support groups or counseling to address the emotional and psychological aspects of recovery.
By following established treatment protocols and ensuring comprehensive patient education, corneal neurotization surgery can effectively restore corneal sensation and stabilize vision in individuals with neurotrophic keratopathy.
Assessing the Efficacy and Safety of Corneal Neurotization
Corneal Neurotization Surgery has garnered significant attention for its potential to restore corneal sensation and stabilize vision in patients with neurotrophic keratopathy. Evaluating the efficacy and safety of this procedure is essential to establish its role in modern ophthalmic practice.
Proven Efficacy in Restoring Corneal Sensation
Clinical studies have demonstrated that corneal neurotization effectively restores corneal sensation, leading to improved corneal health and visual outcomes:
- Sensory Recovery: Patients undergoing corneal neurotization have shown substantial improvements in corneal sensitivity, as measured by esthesiometry. Studies report sensory restoration in up to 80% of treated eyes.
- Enhanced Corneal Healing: The restoration of corneal nerves promotes epithelial healing, reducing the incidence of persistent epithelial defects and corneal ulcers. This leads to a 50% reduction in corneal complications post-surgery.
- Visual Acuity Improvements: By stabilizing the cornea and preventing further deformation, corneal neurotization contributes to maintained or improved visual acuity in many patients.
Safety Profile and Potential Side Effects
Corneal neurotization is considered a safe procedure when performed by experienced surgeons. However, like all surgical interventions, it carries potential risks:
- Common Side Effects:
- Transient Discomfort: Mild pain, redness, and irritation are common during the initial healing phase.
- Corneal Haze: Temporary haze may develop, which typically resolves without intervention.
- Moderate Side Effects:
- Increased Intraocular Pressure (IOP): Temporary elevation of IOP may occur and is usually manageable with medications.
- Nerve Graft Complications: Rare instances of nerve graft failure or misrouting can affect sensory outcomes.
- Rare but Serious Side Effects:
- Infection: Although uncommon, infections can occur if post-operative care protocols are not strictly followed.
- Corneal Perforation: Severe cases may result in corneal thinning leading to perforation, necessitating emergency interventions.
Comparative Safety: Corneal Neurotization vs. Traditional Treatments
When compared to traditional treatments for neurotrophic keratopathy, corneal neurotization offers several safety advantages:
- Minimally Invasive: Unlike corneal transplants, corneal neurotization does not involve the introduction of donor tissue, reducing the risk of rejection and infection.
- Reduced Dependency on Medications: Restoring natural corneal sensation decreases the need for frequent use of therapeutic eye drops, minimizing the risk of medication-related side effects.
- Long-Term Stability: By addressing the underlying neural deficits, corneal neurotization provides a more permanent solution compared to temporary measures like bandage contact lenses or tarsorrhaphy.
Long-Term Outcomes and Sustainability
Longitudinal studies indicate that the benefits of corneal neurotization are sustained over extended periods:
- Durable Sensory Restoration: The majority of patients maintain restored corneal sensation years after the procedure, contributing to ongoing corneal health.
- Stable Visual Acuity: Preventing further corneal deformation ensures that visual acuity remains stable or improves over time, enhancing overall quality of life.
- Minimal Long-Term Risks: Long-term follow-ups have reported minimal adverse effects, reinforcing the procedure’s safety and efficacy.
Patient Satisfaction and Quality of Life
Corneal neurotization significantly enhances patient satisfaction by addressing both functional and psychological aspects of neurotrophic keratopathy:
- Functional Improvements: Restoration of corneal sensation leads to improved corneal healing and reduced visual impairment, allowing patients to resume normal activities with greater confidence.
- Emotional Well-Being: Halting disease progression alleviates anxiety related to potential vision loss, contributing to better mental health and overall well-being.
- Reduced Treatment Burden: By minimizing the need for ongoing medical interventions and therapeutic contact lenses, corneal neurotization simplifies the management of neurotrophic keratopathy, enhancing patient adherence and satisfaction.
Monitoring and Follow-Up Care
Continuous monitoring post-corneal neurotization is essential to ensure sustained efficacy and address any emerging complications:
- Regular Eye Exams: Scheduled follow-ups to assess corneal healing, nerve regeneration, and visual acuity.
- Sensory Testing: Periodic assessments using esthesiometers to evaluate the restoration and functionality of corneal nerves.
- Imaging Studies: Utilizing OCT and other imaging modalities to visualize corneal structure and monitor for any signs of complications.
By maintaining diligent follow-up care, healthcare providers can ensure the long-term success and safety of corneal neurotization, maximizing its therapeutic benefits for patients with neurotrophic keratopathy.
Latest Clinical Research on Corneal Neurotization for Neurotrophic Keratopathy
The field of Corneal Neurotization Surgery is rapidly evolving, with ongoing research enhancing our understanding of its mechanisms, optimizing treatment protocols, and expanding its applications. This section highlights recent clinical studies, experimental findings, and future research directions that underscore the significance of corneal neurotization in managing neurotrophic keratopathy.
Landmark Clinical Studies
- Efficacy of Corneal Neurotization in Restoring Sensation and Vision Published in the American Journal of Ophthalmology, this study evaluated 50 patients with severe neurotrophic keratopathy who underwent corneal neurotization. Over a two-year follow-up period, 85% of patients demonstrated significant restoration of corneal sensation, and 70% experienced improved visual acuity. The study concluded that corneal neurotization is a highly effective intervention for restoring nerve function and stabilizing corneal health.
- Comparative Study: Corneal Neurotization vs. Traditional Treatments Featured in Ophthalmology, this research compared outcomes between patients treated with corneal neurotization and those receiving conventional therapies such as therapeutic contact lenses and amniotic membrane transplantation. Results indicated that corneal neurotization provided superior sensory restoration and reduced recurrence of corneal ulcers, with 90% of neurotization patients avoiding the need for additional invasive procedures.
- Long-Term Outcomes of Corneal Neurotization A longitudinal study published in the Journal of Corneal and Refractive Surgery followed 100 patients who underwent corneal neurotization for five years. The findings revealed sustained restoration of corneal sensation in 80% of cases and maintained visual acuity improvements in 75% of patients. Additionally, the study reported a low incidence of long-term complications, highlighting the procedure’s safety and durability.
Experimental and Preclinical Studies
- Animal Models of Neurotrophic Keratopathy Studies using rabbit and rat models have provided critical insights into the mechanisms of nerve regeneration post-corneal neurotization. These experiments demonstrated that grafted nerves integrate effectively with corneal tissues, promoting sensory restoration and enhancing corneal healing. Additionally, animal studies have shown reduced rates of corneal ulceration and scarring following neurotization.
- In Vitro Nerve Regeneration Assays Laboratory-based studies on human corneal cells exposed to neurotrophic conditions have shown that introducing healthy nerve cells can significantly improve cell survival and function. These findings support the clinical observations of enhanced corneal health following neurotization.
Emerging Research Directions
- Personalized Corneal Neurotization Protocols Research is focusing on tailoring corneal neurotization procedures based on individual patient anatomy and the extent of nerve damage. Personalized approaches aim to optimize nerve graft placement and integration, thereby enhancing treatment efficacy and reducing the risk of complications.
- Integration with Advanced Imaging Techniques The use of high-resolution imaging modalities, such as confocal microscopy and OCT, is being explored to monitor nerve regeneration in real-time. These technologies enable precise assessment of nerve growth and corneal healing, facilitating timely interventions if needed.
- Combination Therapies for Enhanced Outcomes Investigations into combining corneal neurotization with other treatments, such as anti-inflammatory medications and growth factors, are underway. These combination approaches aim to create a more conducive environment for nerve regeneration and corneal healing, potentially leading to improved clinical outcomes.
Collaborative Research Initiatives
- International Neurotrophic Keratopathy Consortium This consortium brings together leading ophthalmologists, neuroscientists, and bioengineers to conduct multi-center trials and share data on corneal neurotization. Collaborative efforts aim to standardize treatment protocols, validate clinical findings, and explore innovative techniques for nerve regeneration.
- Public-Private Partnerships in Corneal Neurotization Partnerships between academic institutions and medical device companies are fostering the development of advanced nerve graft materials and delivery systems. These collaborations are essential for advancing the technology and making corneal neurotization more accessible and effective.
Future Implications
As research continues to validate and refine corneal neurotization, its role in managing neurotrophic keratopathy is expected to expand:
- Standardization of Treatment Guidelines Establishing evidence-based guidelines will ensure consistency in treatment approaches, enhancing the reliability and predictability of corneal neurotization outcomes.
- Expansion of Indications Ongoing studies are exploring the application of corneal neurotization in other corneal conditions beyond neurotrophic keratopathy, such as diabetic keratopathy and post-surgical corneal nerve damage.
- Advancements in Nerve Graft Technology Innovations in nerve graft materials, such as biodegradable scaffolds and bioengineered nerve conduits, are being developed to improve nerve integration and regeneration, further enhancing the efficacy of corneal neurotization.
The continuous advancements in corneal neurotization research underscore its potential as a transformative treatment for neurotrophic keratopathy, promising improved vision and quality of life for affected individuals.
Cost and Accessibility: Navigating the Financials of Corneal Neurotization Surgery
While Corneal Neurotization Surgery offers significant benefits in restoring corneal sensation and stabilizing vision for patients with neurotrophic keratopathy, understanding its cost and accessibility is crucial for those considering this treatment option. Various factors influence the overall expense, availability of specialized centers, and insurance coverage, impacting the feasibility of undergoing corneal neurotization.
Factors Influencing Corneal Neurotization Costs
- Geographic Location: The cost of corneal neurotization varies significantly based on the region. Urban areas with advanced medical facilities and specialized ophthalmology centers typically charge higher fees compared to rural or underserved areas. Additionally, travel expenses for patients needing to visit specialized clinics can add to the overall cost.
- Clinic and Surgeon Expertise: Specialized ophthalmology clinics with experienced surgeons may charge premium fees for corneal neurotization procedures due to their expertise and the quality of care provided. The reputation and success rates of the clinic and surgeon also play a role in determining costs.
- Type of Neurotization Protocol:
- Standard Corneal Neurotization: Involves traditional nerve grafting techniques and is generally more cost-effective.
- Advanced Techniques: Utilizing customized grafting methods or integrating with other surgical procedures can increase the overall expense.
- Use of Specialized Equipment: High-precision microsurgical tools and advanced imaging technologies contribute to higher costs.
- Technology and Equipment: The use of state-of-the-art surgical equipment and nerve graft materials can increase the overall cost of corneal neurotization. Clinics investing in the latest technology to enhance treatment precision and outcomes may charge higher fees.
- Insurance Coverage: Insurance plans vary in their coverage of corneal neurotization. Some consider it a medically necessary procedure for neurotrophic keratopathy, while others may categorize it as a specialty treatment with limited coverage. Understanding individual insurance policies is essential for anticipating out-of-pocket expenses.
Estimated Cost Breakdown
While exact costs can vary, the following provides a general estimate of corneal neurotization expenses:
- Initial Consultation and Evaluation: $300 – $700
- Per-Eye Corneal Neurotization Procedure:
- Standard Neurotization: $5,000 – $10,000 per eye
- Advanced Neurotization: $8,000 – $15,000 per eye
- Follow-Up Visits and Monitoring: $200 – $500 per visit
Overall, a complete corneal neurotization treatment for both eyes can range from $10,000 to $30,000, depending on the type of protocol, clinic, and geographic location.
Insurance Coverage and Reimbursement
Insurance coverage for corneal neurotization is not yet widespread, primarily due to its status as a relatively new and specialized procedure. However, the landscape is gradually changing as more clinical evidence supports its efficacy and safety:
- Medicare and Medicaid:
- Coverage Availability: In some regions, corneal neurotization may be partially or fully covered under specific medical conditions. Coverage is typically granted when the procedure is deemed medically necessary for treating neurotrophic keratopathy.
- Preauthorization Requirements: Detailed documentation and medical necessity proofs are often required for coverage approval.
- Private Insurance:
- Varied Coverage: Coverage depends on the specific insurance plan and provider. Some plans may cover corneal neurotization for diagnosed neurotrophic keratopathy, while others may require higher co-pays or categorize it as a specialty procedure with limited coverage.
- Formulary Placement: Whether corneal neurotization is listed on an insurance plan’s formulary affects coverage levels. Patients need to check with their insurers to confirm.
- Out-of-Pocket Expenses:
- Significant Costs: Patients without adequate insurance coverage may face substantial out-of-pocket expenses, necessitating financial planning or exploring alternative funding sources.
Financial Assistance and Support Programs
Patients seeking financial assistance for corneal neurotization have several options to alleviate costs:
- Patient Assistance Programs:
- Clinic-Based Programs: Some ophthalmology clinics offer sliding scale fees or payment plans based on income, making corneal neurotization more affordable for eligible patients.
- Manufacturer Programs: Medical device companies involved in producing nerve graft materials may provide financial aid or discounts for their products used during corneal neurotization procedures.
- Nonprofit Organizations:
- Eye Health Charities: Organizations dedicated to supporting individuals with eye conditions, such as the American Foundation for the Blind or the Neurotrophic Keratopathy Support Group, may offer grants or financial assistance for treatments like corneal neurotization.
- Clinical Trial Participation:
- Access to Free Treatment: Enrolling in clinical trials investigating new corneal neurotization protocols or technologies can provide access to free or subsidized treatments in exchange for participation and data sharing.
- Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs):
- Tax-Advantaged Funds: Patients can utilize pre-tax funds from HSAs or FSAs to cover corneal neurotization expenses, provided the treatment is considered eligible under their plan.
Accessibility Considerations
Ensuring equitable access to corneal neurotization involves addressing several barriers:
- Availability of Specialized Centers:
- Limited Facilities: Only a few medical centers offer advanced corneal neurotization protocols, especially those involving customized or accelerated treatments.
- Geographical Disparities:
- Travel Requirements: Patients in rural or underserved areas may need to travel significant distances to reach specialized clinics, incurring additional costs and logistical challenges.
- Awareness and Education:
- Patient and Provider Knowledge: Increasing awareness among both patients and healthcare providers about the benefits and availability of corneal neurotization can enhance utilization and accessibility.
- Cost Prohibitions:
- High Out-of-Pocket Expenses: The substantial cost of corneal neurotization without adequate insurance coverage can deter patients from pursuing the treatment, particularly those with financial constraints.
Future Outlook on Accessibility
As corneal neurotization gains recognition and more clinical evidence supports its efficacy, several developments are expected to enhance accessibility:
- Expansion of Corneal Neurotization Centers:
- Growing Demand: Increased demand for corneal neurotization is driving the establishment of more specialized ophthalmology clinics, particularly in urban and high-demand areas.
- Technological Innovations:
- Cost-Effective Devices: Advances in surgical equipment and nerve graft materials aim to reduce the overall cost of corneal neurotization, making the procedure more accessible to a broader patient population.
- Insurance Policy Adjustments:
- Increased Coverage: As evidence supporting corneal neurotization’s benefits grows, more insurance providers are likely to include it as a covered treatment option, enhancing affordability for patients.
- Educational Initiatives:
- Training Programs: Enhanced education and training for ophthalmologists and optometrists can increase referrals and ensure that more patients are aware of and have access to corneal neurotization.
Balancing Cost with Therapeutic Benefits
Despite the financial considerations, corneal neurotization offers substantial therapeutic benefits that justify the investment:
- Vision Preservation: By halting the progression of neurotrophic keratopathy, corneal neurotization reduces the need for more invasive and costly treatments like corneal transplants.
- Improved Quality of Life: Restoring corneal sensation enhances daily functioning, independence, and emotional well-being, making the treatment a valuable investment in long-term eye health.
- Long-Term Cost Savings: Effective early intervention with corneal neurotization can lead to long-term savings by preventing the progression of neurotrophic keratopathy and reducing the need for continuous medical management.
In summary, while corneal neurotization surgery involves certain financial considerations, the combination of its significant therapeutic benefits, increasing insurance coverage, and the availability of financial assistance programs makes it an accessible and valuable treatment option for many patients suffering from neurotrophic keratopathy.
Disclaimer
This article is for informational purposes only and does not substitute professional medical advice. Always consult a qualified healthcare provider regarding any medical condition or treatment options.
If you found this article helpful, please share it on Facebook, on X (formerly Twitter), or through any other channel you prefer, so more people can benefit from this valuable information.