1. Exploring Micropulse Laser Treatment: A Transformative Therapy for DME
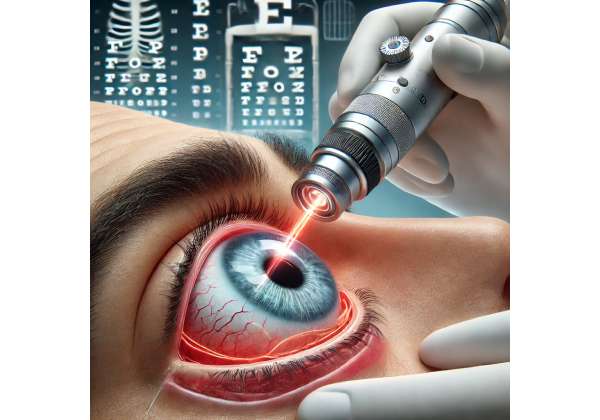
Micropulse laser treatment has gained recognition as a modern, minimally invasive approach for individuals grappling with diabetic macular edema (DME). By delivering pulses of low-energy laser energy at brief intervals, this therapy aims to preserve healthy retinal tissue while tackling the root causes of fluid accumulation. Unlike traditional continuous-wave laser techniques, the micropulse method strives to mitigate potential collateral damage, offering a protective strategy for delicate retinal structures and, by extension, a patient’s central vision.
For many years, conventional laser photocoagulation was the gold standard for treating DME. While effective, it typically deploys stronger thermal energy, which can unintentionally damage surrounding tissues and potentially create scotomas. Macular laser therapy, particularly in its continuous-wave form, has helped stabilize vision for countless individuals; however, breakthroughs in technology have led to the refinement of laser techniques that carry fewer side effects. Micropulse treatment represents the culmination of these advances, blending efficacy with gentler heat generation in the retina.
An Evolution in DME Care
Diabetic macular edema, a major complication of diabetic retinopathy, profoundly impacts quality of life by deteriorating central vision. Diabetes compromises blood vessels in the eye, making them porous and prone to leaking fluid and proteins into the macula. Persistent leakage disrupts the normal macular architecture, causing swelling and visual distortion. Continuous-wave laser therapy was historically effective in controlling some of this leakage, yet it often resulted in retinal scarring that, in turn, could compromise visual acuity or night vision.
Micropulse technology modifies traditional laser energy delivery by fragmenting the emission into thousands of short, repetitive bursts, each followed by a cooling period. This technique is designed to limit the thermal buildup that causes tissue destruction. Thus, while standard laser photocoagulation aims for tissue ablation or destruction of abnormal microvasculature, micropulse therapy focuses on restoring retinal homeostasis and encouraging the eye’s innate repair mechanisms. As a result, many patients benefit from stabilized or improved vision without the trade-off of significant retinal scarring.
Why Choose a Minimally Invasive Approach?
The main appeal of micropulse laser therapy lies in its ability to target problem areas precisely while preserving as much healthy retinal tissue as possible. Individuals with advanced DME or those prone to extensive vascular changes stand to gain the following benefits:
- Reduced Thermal Damage
Because the laser energy is delivered in ultra-brief, low-energy bursts, there is significantly less risk of permanent scarring, thereby preserving the functional capacity of the retina. - Less Patient Discomfort
Patients typically experience less pain during treatment. Although mild discomfort can occur, micropulse therapy is considered less intense compared to older laser modalities. - Synergy with Other Treatments
Many patients combine micropulse sessions with anti-VEGF injections or corticosteroid implants for broader disease management. The gentle nature of micropulse laser allows safe integration with other ophthalmic strategies. - Potential for Repeat Sessions
Traditional laser treatments often have a limit on how frequently they can be repeated without causing severe damage. With micropulse, doctors can safely schedule multiple sessions if necessary, ensuring ongoing control of fluid leakage.
Patient Eligibility and Selection
Micropulse laser therapy is often considered for patients who show persistent macular edema despite receiving anti-VEGF injections. Those with non-central-involving DME or mild to moderate edema may also be suitable candidates, although every individual’s case must be carefully assessed. An ophthalmologist typically evaluates retinal thickness via optical coherence tomography (OCT), checks the severity of retinopathy, and considers the patient’s overall systemic health. Factors like uncontrolled diabetes or active infections might delay the use of laser therapies until the underlying issues are managed.
Because the micropulse approach aims to maintain the integrity of the foveal region (responsible for central vision), it is especially beneficial for those who rely on acute visual detail, such as individuals who read or drive frequently. In mild or moderate DME, micropulse laser therapy can be used as a first-line intervention or as an adjunct to other treatments, based on the physician’s judgment and discussion with the patient.
Long-Term Outlook
Given that diabetes is a chronic condition, maintaining stable vision often requires ongoing vigilance and therapy adjustments. Micropulse laser treatment grants a relatively gentle option within the broader DME arsenal. While not a cure in isolation, it complements systemic measures like glucose control, blood pressure regulation, and lipid management to foster better ocular health. Patients who remain proactive in managing their diabetes can discover that micropulse therapy helps slow or halt disease progression, reducing the complications of repeated surgeries or more invasive treatments.
The sections to follow will delve deeper into the nature of diabetic macular edema itself, the specific science behind micropulse energy delivery, how treatment protocols are established, and the latest findings that underscore its effectiveness and safety. By weaving medical rigor with accessible explanations, the aim is to highlight why micropulse laser therapy holds promise in modern DME management.
2. Understanding Diabetic Macular Edema: The Underlying Challenge
Diabetic macular edema (DME) is a direct result of ongoing microvascular damage from diabetes, a systemic disease characterized by high blood glucose levels. As blood vessels in the retina weaken, fluid and plasma components leak into the retinal tissue, primarily impacting the macula—the central part of the retina essential for detailed vision. While diabetic retinopathy generally starts as mild (non-proliferative) changes, it can advance to proliferative stages involving abnormal blood vessel growth. DME can appear at any stage, putting millions at risk of vision loss.
How Diabetes Triggers Retinal Damage
Chronic hyperglycemia causes a cascade of biochemical changes, particularly in the delicate blood vessels of the retina. Notable mechanisms include:
- Oxidative Stress
Elevated blood sugar levels expedite the production of free radicals, leading to oxidative damage of endothelial cells. - Inflammatory Pathways
Diabetes upregulates pro-inflammatory cytokines like interleukin-1, interleukin-6, and TNF-α. This persistent state of inflammation damages retinal capillaries. - Breakdown of the Blood-Retinal Barrier
The retinal vasculature’s integrity depends on tight endothelial junctions. In diabetic retinopathy, these junctions become weakened or disrupted, enabling fluid to seep into the retinal layers. - VEGF Overexpression
Vascular endothelial growth factor (VEGF) is produced in response to hypoxia and other ischemic conditions. Overproduction of VEGF increases vascular permeability and fosters the development of abnormal new blood vessels, amplifying the risk of DME.
Types of Diabetic Macular Edema
DME can be categorized based on the anatomical location of swelling:
- Focal DME
Occurs due to localized microaneurysms that leak fluid, usually confined to a small area within the macula. - Diffuse DME
Involves diffuse leakage from an extensive area of the capillary network and may more seriously affect the entire macula. - Ischemic Maculopathy
Associated with significant capillary dropout or closure, leading to poor retinal perfusion and severe visual impairment.
Determining the subtype of DME, as well as the overall severity, aids ophthalmologists in formulating precise treatment plans. Imaging modalities like fundus fluorescein angiography (FFA) and OCT are invaluable in assessing how advanced the edema is and whether fluid accumulates in the central macula or only in peripheral areas.
Risk Factors Beyond Blood Sugar
While diabetes duration and glycemic control are central determinants of DME risk, other factors also contribute:
- Hypertension: Elevated blood pressure aggravates microvascular damage, intensifying the leakiness of compromised vessels.
- Dyslipidemia: Abnormal cholesterol levels can exacerbate vascular inflammation and lead to plaque formation in small vessels.
- Kidney Disease: Poorly functioning kidneys reduce the clearance of waste products, promoting a pro-inflammatory environment in the bloodstream.
- Smoking: Tobacco use compounds oxidative stress and vascular dysfunction, hastening the onset of microvascular complications in the retina.
Common Symptoms of Macular Edema
DME often manifests with subtle changes that can easily go unnoticed in the early stages. These include:
- Blurry or Distorted Central Vision
Straight lines might appear curved or wavy, and reading small print becomes challenging. - Difficulty with Color Perception
Colors may seem washed out or less vibrant. - Dark or Empty Areas in Vision
Some patients experience gaps or shadows in their central field of view, hampering their daily activities. - Fluctuations in Visual Sharpness
Vision can vary based on blood sugar levels or fluid retention.
Early detection is crucial. Many guidelines advocate routine screening for diabetic retinopathy, especially for patients who have had diabetes for five years or more or who show additional risk factors. Regular dilated eye exams and non-invasive imaging tests remain the best way to catch DME before it severely impacts vision.
Standard Approaches to DME Management
Before the micropulse laser technique became widely available, clinicians relied on continuous-wave laser photocoagulation and, more recently, pharmacotherapy. The latter includes anti-VEGF agents (like ranibizumab or aflibercept) or intravitreal corticosteroids (e.g., triamcinolone, dexamethasone implants) to reduce vascular permeability and control inflammation. While these treatments can be highly effective, they often necessitate repeated injections to maintain benefit, raising patient burden and expenses.
Laser photocoagulation historically sought to seal leaking vessels and slow disease progression. However, continuous-wave laser therapy can result in visible scars, accidental damage to sensitive retinal areas, and occasional night vision difficulties. By contrast, micropulse laser emerges as a more precise, tissue-sparing modality that can either supplement or replace more aggressive treatments. Recognizing that DME is part of a systemic issue—often intertwined with a patient’s overall diabetic care—underscores the importance of a multifaceted approach involving endocrinologists, nutritionists, and primary care providers for best outcomes.
In the following sections, we will dissect how micropulse laser technology works at a cellular level and how it differs from older laser treatments. By appreciating the nuances of micropulse energy, patients and healthcare professionals alike can make informed decisions about incorporating this technique into a comprehensive DME management plan.
3. The Science Behind Micropulse Laser: How It Targets Diabetic Macular Edema
At the heart of micropulse laser therapy’s success lies a nuanced understanding of thermal dynamics. Traditional continuous-wave laser photocoagulation delivers a single, sustained laser beam to the retina, rapidly heating and coagulating tissue to seal off leaking blood vessels. While effective at controlling leakage, this method can damage adjacent cells, leading to scarring and possible visual field deficits. Micropulse technology alters that paradigm by segmenting the laser beam into rapid, low-power pulses—fundamentally changing how heat is generated and dissipated.
Pulsed Energy Delivery: The Fundamentals
Instead of one continuous shot, micropulse lasers break the beam into a train of ultrashort bursts, or “micropulses,” each often measured in microseconds (µs). Between pulses, there is a cooling interval that dissipates heat, preventing a damaging thermal buildup in the retinal pigment epithelium (RPE) and photoreceptors. This approach aims to induce beneficial biological effects—such as improved metabolism and reduced fluid leakage—without initiating irreversible tissue necrosis.
The “duty cycle” is a crucial concept in micropulse therapy. It represents the ratio of “laser on” time to the total duration of one pulse cycle. A lower duty cycle (e.g., 5%) means the laser is active for a shorter fraction of each cycle, further reducing heat accumulation. Conversely, a higher duty cycle introduces more thermal energy per pulse, potentially intensifying treatment but also raising the risk of unwanted burns. By fine-tuning the duty cycle, physicians can personalize treatment to the edema’s severity and the patient’s tolerance.
Biological Effects of Subthreshold Laser Application
Although micropulse laser does not produce a visible burn like conventional photocoagulation, research indicates it sparks multiple positive changes at the cellular and molecular levels:
- RPE Stimulation
The RPE cells play a vital role in maintaining the health of photoreceptors, specifically in waste removal and nutrient transport. Subthreshold laser energy can boost RPE metabolism, enhancing its capacity to manage fluids and reduce edema. - Regulation of Cytokines and Growth Factors
Mild heat stress from micropulse therapy may modulate factors like VEGF and pigment epithelium-derived factor (PEDF). Balancing these molecules can curb neovascularization and reduce vascular permeability. - Microvascular Stabilization
By toning down local inflammation and fluid leakage, micropulse energy stabilizes the microvasculature within the retina, thus mitigating the progression of edema. - Minimal Photoreceptor Damage
Since micropulse therapy hinges on a sublethal thermal dose, the photoreceptors and surrounding neuronal structures remain largely intact. This underscores micropulse’s advantage in preserving central vision.
Comparisons to Other Laser Modalities
Laser therapies for diabetic retinopathy span a spectrum from intense focal treatments to grid patterns and panretinal photocoagulation for proliferative disease. Some clinicians also employ frequency-doubled Nd:YAG lasers. While each type has its merits, micropulse stands out for its tissue-sparing, subthreshold approach, which leads to fewer side effects and greater potential for repeated treatments over time.
By generating no or minimal scotoma, micropulse laser therapy allows patients to maintain color vision and night vision, areas sometimes impaired by traditional laser scarring. The absence of visible burn marks during or after treatment can be confusing for those used to seeing immediate effects from conventional photocoagulation, but it underscores the gentler nature of this method.
Device Configuration and Parameters
Different laser platforms offer micropulse technology, frequently associated with diode or solid-state lasers in wavelengths such as 810 nm or 577 nm. The selection of wavelength can affect how deeply the laser energy penetrates and how specifically it targets pigmented retinal layers. Regardless of the exact wavelength, surgeons generally calibrate power settings, pulse durations, and duty cycles using standardized protocols or guidelines from manufacturers and professional bodies.
Notably, micropulse therapy can be delivered through contact or non-contact laser lenses, improving precision. By mapping the target areas of edema using OCT images, the physician can plan a treatment zone that addresses leaks effectively while avoiding delicate foveal structures.
Limitations and Considerations
While micropulse laser therapy carries distinct advantages, some limitations exist:
- Treatment Customization: The subthreshold nature means outcomes can vary, and fine-tuning power settings is critical. Overly conservative settings may under-treat edema, while aggressive parameters might lead to unintended burns.
- Response Variability: Some patients respond quickly with reduced fluid buildup, whereas others see incremental improvements. A strict protocol for follow-up and re-treatment (if needed) is essential.
- Learning Curve: Practitioners must become adept at balancing duty cycle, pulse duration, and spot size. Although not overly complex, micropulse therapy demands a degree of expertise unique to subthreshold treatments.
Overall, micropulse laser technology is a technically advanced solution rooted in basic thermodynamics and cell biology. By delivering small, repeated doses of energy that trigger tissue repair rather than destruction, this approach offers a valuable alternative or supplement to systemic and intravitreal DME treatments. In the next section, we will delve into how clinicians structure micropulse therapy sessions, from preoperative planning to postoperative care, illuminating the entire process step-by-step.
4. Step-by-Step Approach to Micropulse Laser Therapy: Protocols and Best Practices
Delivering micropulse laser therapy for diabetic macular edema involves a structured workflow that ensures safety, effectiveness, and patient comfort. While each clinic may adopt slight variations, the following comprehensive approach summarizes how healthcare teams typically prepare for, perform, and follow up on micropulse laser procedures.
Preoperative Evaluations and Preparations
- Diagnostic Imaging
Optical coherence tomography (OCT) remains a cornerstone for delineating the extent and location of macular edema. Fluorescein angiography can highlight leaking microaneurysms or ischemic regions, refining the treatment map. - Visual Acuity Assessment
Physicians measure best-corrected visual acuity (BCVA) to establish a baseline. This information is critical for tracking postoperative improvements or stable outcomes. - Medical History Review
Knowing a patient’s diabetic status, HbA1c levels, blood pressure, kidney function, and cholesterol levels helps reveal the broader metabolic factors at play. If these comorbidities are poorly managed, the risk of recurrence or suboptimal laser response increases. - Informed Consent and Discussion
Patients must understand the intent of micropulse therapy—namely to manage edema rather than to cure diabetes—and be aware that multiple sessions could be necessary. The discussion also covers potential risks, such as unintended burns if parameters are set too high (though rare with proper training).
Treatment Planning and Parameter Selection
An individualized plan targets the zones of fluid leakage identified on imaging. The physician chooses:
- Laser Wavelength: Commonly around 577 nm (yellow laser) or 810 nm (infrared), selected based on depth of penetration and the area of retina requiring therapy.
- Spot Size: Usually in the 100–200 µm range for macular treatments.
- Duty Cycle and Power: Duty cycles between 5% and 15% are typical; lower cycles reduce thermal load, while higher cycles intensify the thermal effect. Initial power is often titrated by applying test spots outside the foveal center and observing for subtle changes.
During the Procedure
- Topical Anesthesia
Micropulse laser treatment generally requires only topical anesthetic eye drops to numb the surface. - Patient Positioning
Patients rest their chin on the laser device’s platform, similar to a routine eye exam. A specialized contact lens may be placed on the eye to magnify the view of the retina and stabilize movement. - Laser Application
The ophthalmologist precisely directs the micropulse spots to areas with thickened retina or active leaks. The minimal thermal buildup means no visible color change or lesion typically appears during application, a stark contrast to continuous-wave lasers.
Immediate Post-Treatment Care
Many patients can return to regular activities immediately, though some ophthalmologists recommend briefly resting to confirm no adverse reactions such as increased IOP or acute corneal edema. Mild dryness, irritation, or transient visual fluctuations may occur but usually resolve within hours to a few days.
Follow-Up Schedule and Re-treatment
- Short-Term Visit
A check-up within one to two weeks may be scheduled to rule out complications like choroidal neovascularization or macular scarring. - Subsequent Imaging
OCT is repeated anywhere from one to three months after the procedure to gauge changes in central retinal thickness. If persistent fluid remains, the doctor may consider an additional micropulse session or complementary therapy like anti-VEGF injections. - Monitoring Long-Term Stability
Individuals with diabetes require regular follow-ups to ensure that improvements in macular thickness and visual acuity are maintained. Good systemic management of blood sugar and blood pressure is equally essential to reduce recurrence rates.
Synergistic Combinations and Adjunct Therapies
A hallmark of modern DME management is the use of combined treatments. Many patients already receive intravitreal injections of anti-VEGF drugs (e.g., bevacizumab, ranibizumab, or aflibercept). Incorporating micropulse therapy can help address small foci of leakage that injections may not fully control, or it can help reduce the frequency of these injections:
- Anti-VEGF + Micropulse: This combination can lead to both macular thickness reduction and improved long-term vessel stabilization.
- Steroids + Micropulse: Intravitreal steroids assist in controlling inflammation, while micropulse laser maintains the structural integrity of the macula. Patients prone to steroid-induced IOP elevation, however, require closer monitoring.
Potential Complications and How They Are Managed
Although micropulse laser therapy is significantly safer compared to conventional photocoagulation, a few rare complications include:
- Overtreatment or Misplacement
If laser parameters are set too aggressively or if spots overlap the foveal center, unintended macular burns can occur, leading to permanent scotomas. This is why a careful parameter titration is crucial. - Transient Inflammation
The mild heating effect can trigger short-term inflammatory changes, generally managed with topical steroids or non-steroidal anti-inflammatory drugs (NSAIDs). - Inadequate Response
Not all patients respond equally. If edema remains largely unchanged after repeated micropulse sessions, the ophthalmologist may escalate to other interventions, such as vitrectomy or sustained-release steroid implants.
By adhering to standardized protocols—starting from thorough preoperative imaging to carefully calibrated parameter selection—micropulse laser treatment can be delivered safely and effectively. In the next section, we’ll evaluate the mounting body of evidence that supports micropulse’s favorable safety profile and consistent efficacy in the management of diabetic macular edema.
5. Clinical Outcomes and Safety: Why Micropulse Laser Is Gaining Ground
Micropulse laser therapy has undergone extensive scrutiny to determine its capacity to stabilize or improve vision in diabetic macular edema (DME). Ophthalmologists worldwide are embracing this treatment modality for its relatively gentle approach, reduced risk profile, and promising track record in clinical practice. While no single intervention can claim absolute superiority for every patient, a growing body of evidence underlines micropulse’s effectiveness.
Key Efficacy Metrics
- Retinal Thickening Reduction
Studies consistently report a statistically significant decrease in central macular thickness (CMT) on OCT scans following micropulse laser therapy. Although the degree of reduction varies, many patients exhibit stabilizing or slowly improving thickness over months. - Maintenance or Improvement of Visual Acuity
A principal goal in DME management is preventing further loss of vision. Micropulse laser frequently meets or surpasses this objective, with many participants in research trials retaining or even gaining lines on the Snellen chart. In some comparisons, micropulse outcomes parallel those achieved by continuous-wave lasers but with fewer complications. - Reduced Recurrence of Edema
Because micropulse aims to restore the RPE’s normal fluid transport mechanisms, some patients experience longer remission periods between relapses, obviating the need for frequent repeat injections or additional treatments.
Safety Advantages
- Minimal Retinal Damage
Subthreshold micropulse therapy does not produce full-thickness retinal burns as standard lasers do. This structural preservation translates into lower risks of scotoma or color vision impairment. - Repeatability
The ability to re-treat problematic areas—without cumulative tissue damage—proves especially valuable in chronic, relapsing conditions like DME. Clinicians can adapt the treatment plan over time without escalating risk to essential macular tissue. - Favorable Risk Profile
The typical concerns that accompany macular laser, such as scarring near the fovea, are significantly diminished. Additionally, patients often report minimal discomfort and can typically return to daily activities shortly after the procedure.
Comparisons with Continuous-Wave Lasers and Anti-VEGF Therapy
While pharmacological approaches—particularly anti-VEGF injections—are often first-line therapies for center-involving DME, micropulse laser therapy provides an adjunct or alternative for certain patient profiles:
- Fewer Injections
Some data suggest that adding micropulse laser can decrease the frequency of intravitreal injections, as the subthreshold energy helps maintain fluid control longer. - Preservation of Retinal Sensitivity
Although traditional laser therapy has shown success in preventing severe vision loss, it may degrade local retinal sensitivity. Micropulse, conversely, appears to maintain or even improve local function, an advantage for tasks like reading and recognizing detailed objects. - Combination Benefit
Patients with persistent fluid despite ongoing anti-VEGF therapy may benefit from micropulse laser to address residual leaking microaneurysms or localized swelling.
Real-World Clinical Experiences
Beyond clinical trial data, retrospective case studies and registries corroborate the safety and efficacy of micropulse therapy. Some high-volume ophthalmic centers report notable success rates in halting progression of DME in patients who previously experienced limited response to lasers or injections. Observing robust anatomical improvements, these practices often incorporate micropulse as a standard offering within their broader DME protocol.
Patient-Reported Outcomes and Satisfaction
Patient satisfaction is a core component of modern ophthalmic care. Many micropulse recipients voice appreciation for the reduced discomfort compared to older photocoagulation treatments. They also value the possibility of avoiding the side effects linked with repeated intravitreal injections, such as risk of infection or vitreous hemorrhage.
Limitations to Note
Even though micropulse laser therapy is effective for a majority, a subset of patients might see modest or no benefit. Those with highly advanced DME or significant macular ischemia may require more aggressive approaches like vitrectomy, extended-release steroid implants, or repeated anti-VEGF injections. Furthermore, micropulse’s success can hinge on timely intervention—very late-stage disease, in which structural damage to the macula is already profound, may not respond as well.
All told, micropulse laser therapy emerges as a robust, gentler treatment path that has proven itself in both controlled and real-world settings. Next, we’ll turn to the most recent studies that dig deeper into micropulse’s long-term outcomes, comparative performance, and evolving role in the standard of care for diabetic macular edema.
6. Cutting-Edge Findings: Latest Research on Micropulse for DME
The momentum behind micropulse laser technology continues to build, thanks to rigorous research efforts aimed at clarifying its role in modern diabetic macular edema (DME) management. New clinical trials and observational data contribute valuable perspectives on the therapy’s success rates, safety profiles, and optimal usage patterns, helping both seasoned specialists and newly diagnosed patients make well-informed decisions.
Notable Clinical Trials and Data
- Randomized Controlled Trials (RCTs)
One prominent RCT compared micropulse 577-nm laser treatment with conventional focal/grid laser in patients with center-involving DME. Data revealed that both groups experienced significant reductions in central macular thickness, but the micropulse cohort reported fewer laser-induced lesions and higher rates of retinal sensitivity preservation at the one-year mark. - Micropulse Plus Anti-VEGF
Several studies explore the synergy of micropulse therapy combined with intravitreal anti-VEGF agents like bevacizumab or aflibercept. Results frequently indicate that dual treatment can hasten fluid resolution and allow for fewer injections. Over a 12–24 month follow-up, combined therapy often yields stable or improved best-corrected visual acuity (BCVA) and a decline in macular thickness. - Long-Term Efficacy
Observational studies extending up to three years affirm that micropulse laser can sustainably control DME in a significant fraction of patients, especially those who incorporate lifestyle modifications and manage systemic factors such as glucose levels and hypertension.
Key Statistical Highlights
- Visual Acuity Gains
In one multicenter analysis, approximately 40% of micropulse recipients achieved a gain of at least five letters on the ETDRS visual chart, underscoring the therapy’s potential to enhance central vision. - Anatomical Improvements
Across multiple trials, reductions in mean central subfield thickness ranged from 50 µm to over 120 µm in responsive patients, a clinically meaningful improvement. - Safety Signals
Serious adverse events—like permanent scotomata or significant subretinal hemorrhage—were exceedingly rare, with an incidence under 1%. Most complications noted were mild, temporary, and managed conservatively.
Emerging Insights into Mechanisms
New investigative work delves deeper into how micropulse triggers beneficial changes without causing scarring. Some hypotheses propose that short bursts of controlled heat stimulate the secretion of protective cytokines and growth factors, including pigment epithelium-derived factor (PEDF), which counters the harmful effects of VEGF. Concurrently, mild thermal “conditioning” may upregulate heat shock proteins, further defending retinal cells against stress and degenerative processes.
Comparisons with Novel Laser Technologies
Micropulse is not the only subthreshold approach available. Technologies such as Navigated Laser Photocoagulation (NLP) use advanced imaging to guide laser application accurately. However, many comparative analyses still favor micropulse for its lower heat output and flexible treatment parameters. Evidence suggests that micropulse offers a narrower margin of retinal damage—a noteworthy advantage, particularly for regions near the foveal center.
Evolving Guidelines in Ophthalmic Societies
Professional bodies, including the American Academy of Ophthalmology (AAO) and the European Society of Retina Specialists (EURETINA), have begun incorporating micropulse therapies into their recommendations. While anti-VEGF injections and vitreoretinal surgeries remain crucial for severe or proliferative stages, micropulse therapy is increasingly accepted as a front-line or adjunct solution for mild to moderate DME with minimal ischemia. Formal guidelines encourage personalized approaches, urging clinicians to consider each patient’s unique ocular findings, systemic health, and lifestyle factors.
Future Directions in Research
Ongoing studies seek to fine-tune treatment algorithms:
- Optimized Duty Cycles: Researchers are testing duty cycles as low as 2.5% in attempts to mitigate even the slightest risk of thermal damage, while still providing tangible benefits.
- Predictive Biomarkers: Identifying characteristics—such as baseline retinal thickness or functional imaging markers—may help pinpoint which patients are most likely to respond favorably.
- Extended Follow-Up: Trials lasting five or more years will clarify the durability of micropulse benefits and define ideal intervals for retreatment.
The wealth of data now available solidifies micropulse laser therapy’s place in the evolving landscape of DME treatments. Although not a panacea, it frequently offers high reward with comparatively low risk, particularly for individuals seeking to preserve macular function. In the subsequent section, we’ll examine the financial aspects surrounding micropulse therapy, shedding light on typical pricing structures, insurance coverage, and factors that may influence a patient’s decision.
7. Therapy Price: Costs, Coverage, and Accessibility
Micropulse laser therapy for diabetic macular edema involves specialized laser equipment, training, and clinic resources, all of which factor into the treatment’s overall cost. In many settings, micropulse treatments are priced similarly to other ophthalmic laser procedures, though fees can vary based on the clinic’s location, the complexity of the case, and whether additional diagnostics are performed. Some ophthalmologists bundle the cost of preoperative imaging and post-treatment follow-up visits into a single package, offering a more transparent financial structure.
Many insurance plans, including Medicare and private insurers, recognize micropulse as a medically necessary procedure when used to address DME. Out-of-pocket expenses therefore hinge on an individual’s specific policy, deductible, and co-payment requirements. For those whose coverage is limited, financing options or flexible payment arrangements may be available through certain eye centers. Patients are encouraged to discuss these matters in advance with their providers, ensuring they fully understand both the potential benefits of micropulse therapy and the associated costs or payment options. Some practices also collaborate with patient assistance programs to mitigate financial barriers, broadening access to this innovative treatment.
Disclaimer:
This article is intended for educational purposes and does not replace individualized medical advice. Always consult a qualified healthcare professional to determine the best treatment options for your specific condition.
We invite you to share this article with friends, family, or anyone who might benefit from learning about micropulse laser therapy for diabetic macular edema. Use our Facebook and X (formerly Twitter) share buttons or any other preferred platform—together, let’s help more people discover advanced, minimally invasive options for preserving their vision!