Diabetic retinopathy often compromises daily life by impairing vision. Transcorneal Electrical Stimulation (TCE) is a specialized electrotherapy that sends low-level electrical pulses through the cornea to activate retinal cells and promote functional improvements. This innovative approach has attracted growing attention as a promising addition to existing diabetic retinopathy management strategies. By targeting the eye’s complex neural network and offering a pathway to bolster retinal health, TCE may enhance vision quality and offer long-term benefits to affected individuals. Below, we explore how TCE works, its role in mitigating diabetic retinopathy, relevant treatment protocols, real-world clinical findings, considerations around costs, and much more.
Decoding the Complexities of Diabetic Retinopathy
Diabetic retinopathy is a major complication of diabetes and a leading cause of preventable blindness worldwide. According to the World Health Organization (WHO), roughly one-third of individuals with diabetes exhibit signs of retinopathy—a startling statistic that underscores the serious toll of this disease on global eye health. To grasp how TCE may benefit patients, it is crucial to understand how diabetic retinopathy develops and progresses.
How Diabetes Damages the Retina
Chronic high blood glucose levels can harm blood vessels in the retina, the light-sensitive tissue at the back of the eye. These damaged vessels may leak fluid or even close off, depriving the retinal tissues of oxygen. Over time, new, abnormal vessels can form in the retina (a process called neovascularization). While the body intends to create these vessels to compensate for reduced oxygen supply, these fragile vessels leak or rupture easily, further compromising vision.
Early stages of diabetic retinopathy, often called nonproliferative retinopathy, might present few or even no symptoms. Patients may be unaware of their gradually deteriorating retinal health until they experience blurry vision or difficulty seeing in low light. As the condition moves into advanced stages (proliferative retinopathy), the risk of severe visual loss rises significantly.
The Impact on Vision
Vision loss typically begins subtly. Patients may notice floaters or dark spots in their field of vision, and reading small print may become increasingly challenging. Over time, continued vessel damage can lead to macular edema, where fluid accumulates in the central portion of the retina, reducing visual clarity and color perception. In severe cases, scar tissue and hemorrhages cause permanent vision impairment.
Traditional Management Approaches
Standard treatments for diabetic retinopathy often include strict blood glucose control, blood pressure management, and lipid-lowering therapies. Medical professionals frequently recommend laser therapy (photocoagulation) to seal leaking vessels and inhibit the growth of unwanted new vessels. Intravitreal injections—medications injected directly into the vitreous humor of the eye—are used to manage macular edema and address harmful vascular growth. Vitrectomy surgery, which removes blood-filled or scarred vitreous gel, is reserved for advanced cases. These approaches can be effective but may come with significant expense, potential side effects, or surgical risks.
Why Explore New Modalities?
While current interventions can slow or halt some progression, many patients continue to face challenges with residual vision loss, fluctuating visual acuity, or ongoing complications like recurrent macular edema. As a result, the medical community is actively pursuing complementary therapies. This is precisely where Transcorneal Electrical Stimulation (TCE) steps in. By stimulating the retinal cells and enhancing blood flow, TCE may offer additive benefits to slow or even partially reverse visual deterioration. Patients looking to optimize their vision outcomes often seek such novel techniques to complement established treatments.
Searching for a Holistic Approach
Professionals emphasize a holistic strategy that includes regular eye exams, consistent management of blood sugar, and attention to cardiovascular health. When integrated into this broader plan, TCE could help stabilize or improve existing sight. By targeting the retina’s complex neural network, TCE attempts to re-energize damaged cells, encourage better visual processing, and reduce inflammation—key factors in slowing the progression of diabetic retinopathy.
When patients understand the multi-faceted nature of diabetic retinopathy, they are better positioned to see how TCE fits into comprehensive care. For many, the appeal lies in TCE’s potential to proactively address retina cell vitality, possibly bridging the gap between conventional management and the hope for more meaningful vision recovery.
Diving into Transcorneal Electrical Stimulation: Mechanisms and Therapeutic Scope
Transcorneal Electrical Stimulation (TCE) is grounded in the principle that controlled electrical impulses, applied to the front of the eye, can activate and support retinal cell function. While electrotherapy as a concept has been employed across multiple medical fields—physical therapy, pain management, and neurological rehabilitation—its adoption in ophthalmology is relatively recent.
How TCE Works
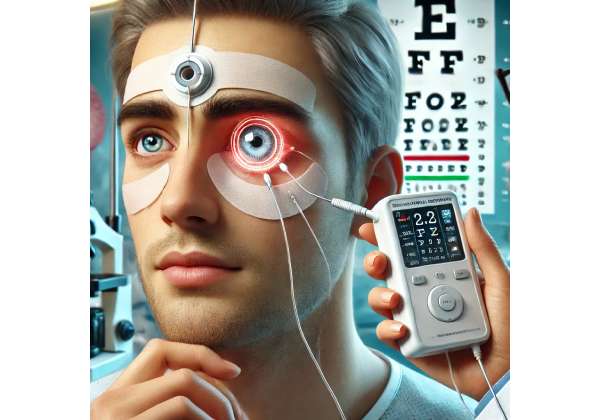
At the core of TCE is the delivery of low-intensity electrical signals through a specialized electrode placed on or near the cornea. Despite its intricate design, the procedure is relatively straightforward for both patient and practitioner. During each session, very gentle currents pass through the cornea and into the retina, stimulating neurons involved in visual signal processing. These impulses may help:
- Enhance Cellular Metabolism: By improving blood flow and oxygenation, TCE can help retinal cells “breathe” more effectively and rid themselves of metabolic waste.
- Activate Dormant Cells: Damaged or underperforming cells may begin functioning more robustly after receiving small electrical boosts, leading to improved communication along the visual pathway.
- Promote Neuroprotective Factors: Research suggests that electrical stimulation can elevate levels of neurotrophic factors—substances that support the survival, growth, and maintenance of neurons—in the retina, thus slowing or reversing cellular damage.
Key Physiological Processes
The retina is an extension of the central nervous system. It houses various cell types, including photoreceptors (rods and cones), bipolar cells, and ganglion cells. In diabetic retinopathy, the microvasculature’s damage affects all these cell layers. The micro-injuries accumulated over years or decades can weaken signal transmission, resulting in suboptimal visual responses.
By introducing low-level electrical currents, TCE may:
- Boost Retinal Blood Flow: Enhanced circulation nourishes cells, reducing oxidative stress.
- Stabilize Retinal Pigment Epithelium (RPE): The RPE is critical for photoreceptor health. Better oxygenation and nutrient supply may maintain RPE integrity, which is essential for absorbing stray light and recycling photopigments.
- Support Synaptic Connectivity: Efficient transmission of impulses among retinal cells translates into sharper vision and better adaptation to different light conditions.
Advantages Over Traditional Therapies
TCE’s primary advantage lies in its noninvasive or minimally invasive nature. When compared to procedures like intravitreal injections or laser surgeries, TCE has a relatively lower risk profile and can be administered more frequently without major disruptions to daily activities. Unlike medication-based interventions, TCE is less likely to induce systemic side effects, such as blood pressure fluctuations or increased intraocular pressure.
That said, TCE does not aim to replace existing therapies outright. Instead, it serves as an additional tool in the ophthalmic arsenal—helpful especially for patients who either have contraindications to certain drugs or who seek to maximize any residual function in their retina. By conferring a neuroprotective effect, TCE may work synergistically with pharmacological agents that reduce edema or halt neovascularization.
Indications for TCE in Diabetic Retinopathy
While TCE has gained attention for multiple vision disorders (e.g., retinitis pigmentosa, optic nerve atrophy), its application in diabetic retinopathy is particularly compelling for individuals who:
- Are in the Early-to-Mid Stages of Retinopathy: Intervention at these stages might preserve and even improve existing visual function, delaying disease progression.
- Have Mild to Moderate Vision Impairment: TCE could potentially yield noticeable improvements in visual acuity or contrast sensitivity.
- Have Other Comorbidities: For patients in whom surgical interventions pose higher risk (e.g., heart disease or advanced kidney disease), TCE can offer a relatively safer adjunct therapy.
Limitations and Considerations
Electrotherapy outcomes can vary widely depending on each patient’s severity of retinal damage, glycemic control, and overall treatment adherence. While TCE is well-tolerated, side effects—though rare—might include mild corneal irritation, eye redness, or discomfort during sessions. Moreover, TCE’s effectiveness in advanced proliferative retinopathy with extensive scarring is still under investigation, and not all patients experience substantial improvement.
Nevertheless, TCE offers a valuable dimension of therapy that extends beyond symptomatic management by addressing possible underlying cellular deficits. In combination with meticulous diabetic care and frequent follow-up exams, TCE can be a strategic tool in boosting retinal resilience.
Designing a TCE Approach: Understanding Protocols and Patient Selection
Adopting TCE requires precise treatment protocols. Patients might expect regular sessions, a customized intensity level, and thorough monitoring of their vision changes. The goal is to ensure optimal stimulation that activates the retina without causing discomfort or stress on the eye.
Initial Patient Evaluation
Before initiating TCE, a comprehensive ophthalmic examination is key. This often includes:
- Visual Acuity Testing: Establishes a baseline to track progress.
- Optical Coherence Tomography (OCT): Provides detailed images of the retina’s layers, assessing edema or abnormalities.
- Fluorescein Angiography: Evaluates blood vessel integrity.
- Fundus Examination: Examines the internal surface of the eye for hemorrhages, microaneurysms, or neovascularization.
- Patient Medical History: Encompasses diabetes duration, glycemic control, comorbidities, and other eye conditions, like glaucoma or cataracts.
Additionally, specialists will ensure that the cornea is healthy enough to handle the electrode placement. If corneal scarring or severe dry eye is present, doctors might modify or delay TCE until the cornea is stable.
Session Frequency and Duration
TCE sessions often last about 20–30 minutes, with the actual stimulation phase spanning a few minutes. To elicit meaningful improvements, multiple sessions are typically recommended. The frequency can vary from weekly or biweekly to monthly, depending on the individual’s disease stage and clinical response.
- Acute Phase Protocol: In early to mid-stage diabetic retinopathy, some providers may advise weekly TCE sessions for a set period (e.g., six to eight weeks) to quickly capitalize on the neuroprotective and microcirculatory boosts.
- Maintenance Phase Protocol: After initial gains are observed, the frequency might be tapered to monthly or quarterly sessions to sustain progress.
Treatment breaks are sometimes employed to allow the eye to adapt and recover, preventing overstimulation. During these breaks, ophthalmologists track changes in visual function to refine the protocol for future sessions.
Intensities and Electrode Placement
The electrical intensity is measured in microamperes or milliamperes. Too little current may be ineffective; too much may irritate the cornea or the retina. Modern TCE devices often have built-in safety features, regulating maximum current thresholds to avoid accidental overexposure.
- Corneal Contact Lens Electrode: A customized contact lens embedded with an electrode gently contacts the cornea. A separate electrode is placed on the skin or behind the ear to complete the circuit.
- Transpalpebral Electrodes: In some setups, electrodes are placed on the closed eyelid. However, direct corneal contact typically ensures more precise stimulation of retinal cells.
Integrating TCE with Other Treatments
TCE can be synchronized with conventional treatments such as anti-VEGF injections or laser therapy. Physicians often schedule TCE sessions a few days or weeks apart from these interventions to track any synergistic effects. For instance, a patient receiving monthly intravitreal injections for macular edema may undergo TCE sessions in between to provide additional neuroprotective benefits.
It is essential to maintain close communication with one’s medical team. Endocrinologists managing diabetes should be aware of the TCE protocol to coordinate overall care, ensuring tight control of blood glucose and addressing any potential drug-device interactions.
Patient Adherence and Lifestyle Adjustments
Like most interventions, TCE benefits are amplified by consistent follow-up and healthy lifestyle choices. Patients are encouraged to:
- Maintain Optimal Glycemic Control: High blood glucose can counteract the positive effects of TCE by continuing to damage retinal vessels.
- Monitor Blood Pressure and Lipids: Effective cardiovascular management supports improved circulation in the retina.
- Adopt a Nutritious Diet: Antioxidant-rich foods, including leafy greens and colorful fruits, can promote cellular health.
- Stay Compliant with Eye Appointments: Regular screenings catch relapses or complications early, helping refine TCE protocols in real time.
Given that TCE is not a one-time solution, patients must view it as part of an ongoing plan. Attendance at scheduled sessions and open communication about any vision changes or side effects enable medical teams to tailor interventions for the best possible outcome.
Unveiling the Latest Research: Clinical Evidence and Notable Studies
Substantial clinical interest in TCE has sparked a range of studies focused on its efficacy and safety for diabetic retinopathy. While the body of research is still evolving, preliminary findings are promising, suggesting that TCE can indeed complement existing treatments for enhanced vision preservation and even recovery.
Key Clinical Investigations
- Multi-Center Pilot Studies: Early phase trials have explored TCE in patients with nonproliferative diabetic retinopathy. Several reported moderate improvements in best-corrected visual acuity (BCVA) and contrast sensitivity.
- Randomized Controlled Trials: Researchers conducted trials to compare TCE plus standard care (laser therapy, anti-VEGF injections) against standard care alone. Participants who received TCE showed slower progression of retinopathy over a six- to twelve-month follow-up period.
- Long-Term Observational Studies: A few observational studies followed patients for more than a year to evaluate sustained benefits. While results varied, a significant portion of participants reported stable or improved vision, which was correlated with consistent TCE sessions and tight metabolic control.
Understanding the Mechanisms Through Research
Clinical data point to how TCE might influence specific molecular and vascular pathways:
- Promotion of Angiogenic Balance: TCE may modulate growth factors like VEGF (Vascular Endothelial Growth Factor), helping preserve functional vasculature without promoting the formation of leaky new vessels.
- Reduction in Inflammatory Markers: Elevated inflammation often contributes to diabetic retinopathy. Certain studies demonstrate that TCE can lower local cytokine levels, reducing cellular stress in the retina.
- Optic Nerve Support: Some research also indicates a supportive effect on the optic nerve head, which may be beneficial for overall visual function.
Highlight on Efficacy in Early to Moderate Stages
Study outcomes repeatedly highlight that patients in the earlier or moderate stages of retinopathy tend to reap the most benefits. This aligns with the idea that TCE likely works best when there is sufficient viable retinal tissue to stimulate. In severe proliferative or end-stage retinopathy, extensive scarring or hemorrhages may limit the therapy’s reach.
Quantifying Vision Improvement
Quantifying changes in vision can be challenging, as improvements may be subtle. Researchers measure:
- LogMAR Visual Acuity: A standard measure for tracking small increments of acuity changes. Even a 0.1 or 0.2 LogMAR improvement can enhance day-to-day visual tasks.
- Contrast Sensitivity Tests: Improved contrast sensitivity can help patients navigate low-light environments and distinguish objects more effectively.
- Visual Field Assessments: Certain TCE protocols may bolster peripheral vision, valuable for safe mobility.
Real-World Data
Aside from controlled research settings, increasing anecdotal and real-world evidence supports TCE’s role in sustaining functional vision. Ophthalmic clinics offering TCE have reported overall positive patient feedback, with some individuals noticing clearer vision in less than a month. However, personal experiences differ widely, reinforcing the need for individualized treatment plans.
Ongoing Investigations
Large-scale, multi-year clinical trials are underway to definitively establish the therapy’s long-term safety profile and cost-effectiveness. Topics under examination include:
- Optimal Session Frequency: Pinpointing exactly how many sessions per month yield the most sustained results without imposing unnecessary patient burden or cost.
- Combination Therapy Protocols: Exploring how TCE might synergize with emerging gene therapies or new classes of intravitreal medications.
- Prognostic Indicators: Identifying patient characteristics—such as retina thickness, glycemic control patterns, or inflammatory markers—that predict the best outcomes.
Researchers remain committed to fine-tuning TCE for maximum impact. The growing body of evidence points to TCE as a valuable asset in bridging the gap between stable disease control and potential vision improvements for those living with diabetic retinopathy.
Assessing Efficacy and Safety: Real-World Outcomes of TCE
For medical professionals and patients alike, efficacy and safety sit at the heart of any new treatment. TCE is no different. By examining clinical data, patient testimonials, and post-market surveillance, we can draw a balanced view of what to expect.
Measuring Treatment Success
Success in TCE is often multi-dimensional. It may involve halting the deterioration of visual acuity, enhancing contrast sensitivity, or simply improving a patient’s ability to complete daily tasks. Some common measures used in practice include:
- Functional Assessments: Eye care providers may administer reading charts or mobility tests under various lighting conditions to see if patients notice tangible improvements.
- Subjective Patient Reports: Some individuals report reduced glare or quicker adaptation to darkness, both of which significantly affect quality of life but are not always reflected in standard visual acuity tests.
- Ocular Imaging: OCT scans before and after TCE can show whether macular thickness has stabilized or decreased.
The Safety Profile
Overall, TCE is generally considered to have a favorable safety margin:
- Mild Irritation: A small percentage of individuals may experience temporary redness or foreign body sensation in the eye after each session. This usually resolves without interventions.
- Risk of Overstimulation: Excessively high current can theoretically damage the cornea or retina, but modern devices and properly trained clinicians mitigate this risk with strict protocols and built-in safety mechanisms.
- Compatibility: TCE typically does not interfere with other diabetic retinopathy treatments, making it a flexible add-on. Regular monitoring ensures that changes in the retina are tracked to avoid any adverse overlap with intravitreal injections or laser treatments.
Patient Selection Criteria and Contraindications
TCE’s best results often occur in patients who meet specific criteria:
- Retina Health: Sufficient healthy retinal cells that can respond to electrical stimulation.
- Stable Corneal Surface: The absence of severe corneal scarring or active infections that might complicate electrode placement.
- Healthy Ocular Pressure: Individuals with advanced glaucoma or severe ocular hypertension might warrant more caution.
Moreover, certain contraindications exist, although they are relatively rare. Patients with implanted cardiac pacemakers or severe arrhythmias might require cardiology evaluation before commencing TCE because of the use of electrical currents near the head and neck.
Balancing Risks and Benefits
Compared to the potential complications of more invasive procedures, TCE is considered relatively low risk. However, it remains essential for healthcare providers to monitor each patient’s response carefully. If improvements plateau or side effects arise, adjustments in session frequency or current intensity can be made. The absence of systemic side effects is a significant advantage, as diabetic patients often juggle multiple medical conditions and are wary of treatments that could exacerbate those issues.
Success Stories and Clinical Vignettes
Some patients who were gradually losing the ability to read small print or identify faces from a distance have reported marked improvements after multiple TCE sessions, supported by consistent glycemic control. Additionally, individuals with mild neovascular changes have found that TCE, paired with anti-VEGF injections, helped slow the formation of new vessels more effectively than injections alone. While not a cure, these case studies spotlight TCE’s tangible impact on day-to-day visual function and overall quality of life.
Importance of Continuous Evaluation
Because diabetic retinopathy is a chronic, progressive disease, regular evaluations are paramount. Individuals who start TCE often continue for months or even years, with an adaptable approach to tweak intensity levels and scheduling. Ophthalmologists may alternate therapy breaks with intensives depending on a patient’s condition. This dynamic method allows for more personalized care, ensuring that TCE remains beneficial over the long term.
In conclusion, the majority of clinical data and anecdotal evidence collectively portray TCE as a safe, well-tolerated therapy that can yield meaningful visual improvements or at least halt rapid deterioration in patients with diabetic retinopathy. Its noninvasive nature, minimal systemic impact, and potential for synergy with other standard treatments mark it as a notable option for individuals striving to preserve or enhance their vision.
Estimated Costs and Financial Options for TCE
Costs for TCE sessions can vary widely, reflecting factors such as clinic location, the experience of the medical provider, and whether advanced diagnostic imaging is included. Each TCE treatment can range from several hundred to over a thousand dollars, and a series of sessions is generally recommended. Many clinics provide flexible payment plans, and some insurance policies may offer partial coverage if TCE is deemed medically necessary. It is advisable to inquire about package deals or discounts when multiple sessions are pre-booked. Patients should carefully verify coverage details with their insurance carrier or consider healthcare financing programs to minimize out-of-pocket expenses.
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice, diagnosis, or treatment. Always consult qualified healthcare providers for personalized guidance regarding any medical concerns or treatment options.
We invite you to share this article to help others discover valuable insights on TCE and diabetic retinopathy. Feel free to use our Facebook and X (formerly Twitter) share buttons or any preferred method to spread the word!