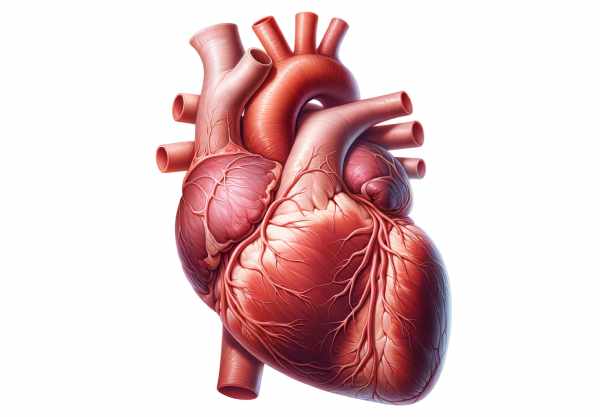
The heart is the central powerhouse of the circulatory system, tirelessly pumping blood to deliver oxygen and nutrients throughout the body while removing waste products. This vital organ works ceaselessly to maintain homeostasis and supports every cell, tissue, and organ. Its complex structure—including four chambers, specialized valves, and a finely tuned electrical conduction system—ensures efficient blood flow and robust performance under various physiological conditions. In this comprehensive guide, we delve into the intricate anatomy, dynamic physiology, common disorders, advanced diagnostic techniques, treatment modalities, and lifestyle strategies to help you maintain a healthy heart and overall well-being.
Table of Contents
- Structural Anatomy & Composition
- Cardiac Physiology & Functional Dynamics
- Common Heart Conditions & Disorders
- Diagnostic Techniques & Evaluation Methods
- Treatment Strategies & Interventions
- Nutritional Strategies & Supplements
- Lifestyle Recommendations for Heart Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
Structural Anatomy & Composition
The heart is a robust, muscular organ located within the thoracic cavity, predominantly to the left of the midline. It is enclosed in a protective double-walled sac known as the pericardium, which minimizes friction as the heart beats. The heart’s structure is meticulously organized to ensure optimal performance in blood circulation.
Cardiac Chambers
The heart comprises four chambers, each playing a distinct role in the circulatory process:
- Right Atrium:
This upper chamber receives deoxygenated blood from the body through the superior and inferior vena cavae. Acting as a holding reservoir, the right atrium prepares the blood for passage into the right ventricle. - Right Ventricle:
The right ventricle receives blood from the right atrium and pumps it into the pulmonary circulation via the pulmonary artery. Its walls are thinner than those of the left ventricle since it operates under lower pressure. - Left Atrium:
Oxygenated blood from the lungs returns to the heart through the pulmonary veins into the left atrium. This chamber acts as a collecting station before transferring blood to the left ventricle. - Left Ventricle:
The powerhouse of the heart, the left ventricle, pumps oxygen-rich blood to the entire body through the aorta. Its thick muscular walls generate the high pressures necessary for systemic circulation.
Cardiac Valves
Valves within the heart ensure that blood flows in one direction, preventing backflow during the cardiac cycle. The four primary valves are:
- Tricuspid Valve:
Positioned between the right atrium and right ventricle, it prevents backflow of blood into the atrium during ventricular contraction. - Pulmonary Valve:
Located at the exit of the right ventricle, it stops blood from re-entering the ventricle after being pumped into the pulmonary artery. - Mitral Valve:
Also known as the bicuspid valve, it sits between the left atrium and left ventricle, ensuring one-way flow as blood is transferred for systemic circulation. - Aortic Valve:
At the exit of the left ventricle, this valve prevents blood from flowing back into the ventricle after it is pumped into the aorta.
Layers of the Heart Wall
The heart wall is composed of three main layers that contribute to its structure and function:
- Epicardium:
The outermost layer, which is also part of the pericardium, acts as a protective barrier and provides a smooth surface for the heart’s movement. - Myocardium:
The thick, muscular middle layer is responsible for the contractile force of the heart. It consists of cardiac muscle fibers arranged in a spiral pattern to optimize the pumping action. - Endocardium:
The innermost layer lines the heart’s chambers and valves, providing a smooth, frictionless surface for blood flow and playing a role in the regulation of heart function.
Coronary Circulation
The heart’s own blood supply is delivered through the coronary arteries. The left coronary artery, which bifurcates into the left anterior descending (LAD) and the circumflex arteries, supplies the left side of the heart, while the right coronary artery (RCA) caters to the right side and parts of the conduction system. Proper coronary circulation is essential for delivering oxygen and nutrients to the myocardium.
Electrical Conduction System
The heart’s electrical system orchestrates the rhythmic contractions of the cardiac muscle. Key components include:
- Sinoatrial (SA) Node:
Often referred to as the natural pacemaker, it initiates electrical impulses that set the heart’s rhythm. - Atrioventricular (AV) Node:
This node delays the electrical signal, ensuring that the atria have sufficient time to contract and fill the ventricles before they contract. - Bundle of His and Purkinje Fibers:
These pathways distribute the electrical impulse throughout the ventricles, resulting in coordinated contraction and efficient blood ejection.
This intricate anatomical structure ensures that the heart functions as a highly efficient pump, capable of meeting the body’s constant demands for oxygenated blood.
Cardiac Physiology & Functional Dynamics
The heart’s physiology is fundamental to its role as the engine of the circulatory system. It functions through a finely coordinated sequence of electrical and mechanical events that ensure continuous, effective blood circulation.
The Cardiac Cycle
The cardiac cycle encompasses the series of events that occur during one heartbeat, including contraction and relaxation phases.
- Systole:
During systole, the heart muscle contracts. This phase is divided into: - Atrial Systole: The atria contract, pushing blood into the ventricles.
- Ventricular Systole: The ventricles contract, forcing blood into the pulmonary artery and aorta. The closure of the atrioventricular valves prevents backflow into the atria.
- Diastole:
In diastole, the heart relaxes, allowing the chambers to fill with blood. The reopening of the atrioventricular valves facilitates the flow of blood from the atria to the ventricles. Diastole is crucial for ensuring that the heart is adequately filled before the next contraction.
Heart Rate and Cardiac Output
The autonomic nervous system finely tunes the heart rate and cardiac output to match the body’s varying demands:
- Heart Rate:
The SA node sets the baseline heart rate. The sympathetic nervous system increases the rate during stress or physical activity, while the parasympathetic system slows it during rest. - Stroke Volume and Cardiac Output:
Stroke volume, the amount of blood pumped per beat, multiplied by the heart rate, yields cardiac output. Factors influencing stroke volume include preload, afterload, and myocardial contractility.
Regulation of Blood Pressure
Blood pressure is maintained through the interplay of heart function, vascular resistance, and kidney regulation:
- Systolic and Diastolic Pressure:
Systolic pressure, measured during ventricular contraction, and diastolic pressure, during ventricular relaxation, are key indicators of cardiovascular health. - Baroreceptor Reflex:
Baroreceptors in the aorta and carotid arteries sense changes in blood pressure and send signals to the brain to adjust heart rate and vascular tone accordingly.
Electrical Conduction and Coordination
The heart’s electrical conduction system ensures that all parts of the heart contract in a coordinated manner:
- Impulse Initiation and Propagation:
Electrical impulses originate in the SA node and travel through the AV node, the Bundle of His, and Purkinje fibers to prompt synchronized contractions across the ventricles. - Conduction Abnormalities:
Disruptions in this system can lead to arrhythmias, which may affect cardiac output and overall cardiovascular health.
Oxygen and Nutrient Delivery
The heart’s relentless pumping action ensures that oxygenated blood reaches all tissues and that metabolic waste is efficiently removed. The circulation of blood is vital for:
- Gas Exchange:
Oxygen is delivered to tissues while carbon dioxide is removed. - Nutrient Distribution:
Nutrients absorbed in the digestive system are distributed to cells throughout the body.
In essence, the heart’s physiology is a masterful orchestration of electrical impulses, muscular contractions, and regulatory mechanisms that work together to sustain life by continuously circulating blood and maintaining homeostasis.
Common Heart Conditions & Disorders
Despite its critical role in sustaining life, the heart is susceptible to various disorders that can compromise its function. Early diagnosis and management are essential to prevent severe complications and improve outcomes.
Coronary Artery Disease (CAD)
- Pathophysiology:
Coronary artery disease occurs when the coronary arteries become narrowed or blocked due to atherosclerosis. This reduces blood flow to the heart muscle, leading to ischemia and potentially causing angina or myocardial infarction. - Risk Factors:
Factors include smoking, high cholesterol, hypertension, diabetes, obesity, sedentary lifestyle, and a family history of heart disease. - Symptoms:
Common symptoms include chest pain or discomfort, shortness of breath, fatigue, and sometimes nausea. - Management:
Treatments range from lifestyle modifications and medications (such as statins, beta-blockers, and nitrates) to interventional procedures like angioplasty and coronary artery bypass grafting (CABG).
Heart Failure
- Definition:
Heart failure occurs when the heart is unable to pump blood effectively, leading to inadequate tissue perfusion and fluid buildup in the lungs and other tissues. - Types:
It can be classified as systolic (reduced ejection fraction) or diastolic (preserved ejection fraction) heart failure. - Symptoms:
Symptoms include breathlessness, fatigue, swelling in the legs and ankles, and a rapid or irregular heartbeat. - Management:
Treatment involves lifestyle changes, medications (such as ACE inhibitors, diuretics, and beta-blockers), and in severe cases, device therapy or heart transplantation.
Arrhythmias
- Overview:
Arrhythmias are disorders of the heart’s rhythm. They can cause the heart to beat too fast, too slow, or irregularly, affecting the efficiency of blood flow. - Common Types:
Atrial fibrillation, ventricular tachycardia, and bradycardia are among the most common. - Symptoms:
Patients may experience palpitations, dizziness, chest discomfort, and, in severe cases, syncope (fainting). - Treatment:
Management includes medications (such as antiarrhythmics), lifestyle modifications, and procedures like catheter ablation or the implantation of pacemakers and defibrillators.
Hypertension
- Definition:
Hypertension, or high blood pressure, is a common condition that, if left untreated, can lead to heart disease, stroke, and kidney damage. - Risk Factors:
Genetic predisposition, obesity, high salt intake, stress, and sedentary lifestyle all contribute. - Symptoms:
Often asymptomatic, hypertension is typically detected during routine screening. - Management:
Lifestyle modifications, along with medications like ACE inhibitors, beta-blockers, and diuretics, help maintain blood pressure within a healthy range.
Valvular Heart Disease
- Overview:
Valvular heart disease involves dysfunction of one or more of the heart’s valves, leading to impaired blood flow. This can result from congenital abnormalities, degenerative changes, infections (endocarditis), or rheumatic fever. - Symptoms:
Symptoms include fatigue, shortness of breath, chest pain, and palpitations. - Treatment:
Management depends on the severity and may include medications, valve repair, or replacement via surgical or transcatheter methods.
Cardiomyopathy
- Definition:
Cardiomyopathy is a disease of the heart muscle that can lead to heart failure. It may be due to genetic factors, chronic high blood pressure, or damage from toxins or infections. - Types:
Dilated, hypertrophic, and restrictive cardiomyopathy are the primary forms. - Symptoms:
These include breathlessness, swelling, and arrhythmias. - Management:
Treatment includes medications, lifestyle modifications, and, in severe cases, implantable devices or heart transplantation.
Understanding these conditions is essential for early diagnosis and intervention, which can prevent severe complications and enhance overall heart function.
Diagnostic Techniques & Evaluation Methods
Accurate diagnosis of heart conditions is crucial for effective treatment and management. A variety of diagnostic tools and imaging techniques help clinicians assess the heart’s structure, function, and overall health.
Electrocardiogram (ECG/EKG)
- Overview:
An electrocardiogram measures the electrical activity of the heart using electrodes placed on the skin. It provides a graphical representation of heart rhythms, helping to detect arrhythmias, myocardial infarctions, and other electrical abnormalities. - Procedure:
Electrodes are attached to specific locations on the chest, arms, and legs, and the electrical impulses generated by the heart are recorded over a few minutes.
Echocardiography
- Transthoracic Echocardiography (TTE):
A non-invasive ultrasound test that provides real-time images of the heart’s chambers, valves, and overall function. TTE is instrumental in diagnosing structural heart disease, valve disorders, and heart failure. - Transesophageal Echocardiography (TEE):
In TEE, an ultrasound probe is inserted into the esophagus to obtain clearer images of the heart, particularly when TTE results are inconclusive. This method is valuable for assessing the left atrium, atrial appendage, and aorta.
Stress Testing
- Exercise Stress Test:
This test evaluates the heart’s performance under physical stress. The patient walks or runs on a treadmill while heart rate, blood pressure, and ECG are monitored to detect exercise-induced ischemia. - Pharmacologic Stress Test:
For patients unable to exercise, medications stimulate the heart to mimic exercise conditions, allowing clinicians to assess blood flow and detect coronary artery disease.
Cardiac Catheterization and Angiography
- Procedure:
A catheter is inserted into a blood vessel and advanced to the heart. Contrast dye is injected, and X-ray images (angiograms) are taken to visualize the coronary arteries, identifying blockages or narrowing. - Applications:
This procedure is critical for diagnosing coronary artery disease and for planning interventional procedures such as angioplasty or stent placement.
Cardiac Magnetic Resonance Imaging (MRI)
- Technique:
Cardiac MRI uses magnetic fields and radio waves to produce detailed images of the heart’s anatomy and function. It is particularly useful for assessing myocardial viability, congenital heart disease, and cardiomyopathies. - Advantages:
MRI offers excellent soft tissue contrast without exposing the patient to ionizing radiation.
Computed Tomography (CT) Angiography
- Overview:
CT angiography combines CT scanning with contrast dye to visualize the coronary arteries. It is useful for detecting coronary artery disease and assessing cardiac structures in detail. - Procedure:
Rapid CT imaging is performed after the injection of contrast material, producing high-resolution images of the heart and vessels.
Blood Tests and Biomarkers
- Troponin:
Troponin levels are measured to detect heart muscle damage, particularly in cases of myocardial infarction. - Lipid Profile:
Evaluates cholesterol and triglyceride levels, which are important for assessing cardiovascular risk. - B-type Natriuretic Peptide (BNP):
Elevated BNP levels indicate heart failure and help gauge the severity of the condition.
By utilizing these diagnostic techniques, healthcare professionals can comprehensively evaluate heart health, accurately identify underlying conditions, and develop effective treatment strategies tailored to the individual patient.
Treatment Strategies & Therapeutic Interventions
Treating heart conditions often requires a multifaceted approach that encompasses lifestyle changes, pharmacologic therapies, interventional procedures, and surgical options. Tailoring the treatment to the specific cardiac condition is essential for optimal outcomes.
Lifestyle Modifications
- Dietary Changes:
A heart-healthy diet is critical. Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting saturated fats, trans fats, cholesterol, and sodium. Dietary adjustments can reduce the risk of coronary artery disease and hypertension. - Regular Exercise:
Engaging in aerobic activities such as walking, cycling, or swimming for at least 150 minutes per week can improve cardiovascular fitness, lower blood pressure, and support weight management. - Smoking Cessation:
Quitting smoking is one of the most impactful lifestyle changes to improve heart health by reducing the risk of atherosclerosis, heart attacks, and stroke. - Stress Management:
Techniques such as mindfulness, yoga, and meditation help reduce stress, which can have a beneficial effect on heart rate, blood pressure, and overall cardiovascular health. - Weight Management:
Maintaining a healthy weight reduces the strain on the heart and lowers the risk of developing heart disease.
Pharmacologic Therapies
- Antihypertensives:
Medications like ACE inhibitors, beta-blockers, calcium channel blockers, and diuretics help control high blood pressure, a major risk factor for heart disease. - Antiplatelet and Anticoagulant Agents:
Drugs such as aspirin, clopidogrel, and warfarin reduce the risk of clot formation, which is essential for preventing heart attacks and strokes. - Cholesterol-Lowering Medications:
Statins and other lipid-lowering agents help manage cholesterol levels, thereby reducing the risk of coronary artery disease. - Heart Failure Medications:
For heart failure, medications like ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists help manage symptoms and improve cardiac function.
Interventional Procedures
- Percutaneous Coronary Intervention (PCI):
PCI, commonly known as angioplasty, involves the use of a balloon catheter and stents to open blocked coronary arteries, improving blood flow and reducing the risk of heart attacks. - Catheter Ablation:
This procedure targets abnormal electrical pathways in the heart to treat arrhythmias. It involves inserting a catheter to deliver energy to the problematic tissue, restoring a normal heart rhythm.
Surgical Interventions
- Coronary Artery Bypass Grafting (CABG):
CABG surgery creates new pathways for blood to bypass blocked coronary arteries, ensuring adequate blood supply to the heart muscle. - Valve Repair or Replacement:
Surgical intervention may be necessary to repair or replace defective heart valves, restoring proper blood flow and reducing symptoms such as shortness of breath and fatigue. - Heart Transplant:
In cases of end-stage heart failure, a heart transplant may be the only viable option. Transplantation involves replacing the diseased heart with a healthy donor heart.
Emerging and Innovative Therapies
- Gene Therapy:
Research is ongoing into gene therapies that could potentially correct genetic abnormalities responsible for certain heart diseases, offering new avenues for treatment. - Stem Cell Therapy:
Experimental stem cell treatments aim to regenerate damaged heart tissue, potentially improving function in patients with heart failure. - Implantable Devices:
Devices such as pacemakers, implantable cardioverter-defibrillators (ICDs), and left ventricular assist devices (LVADs) provide mechanical support for patients with severe heart conditions. - Remote Monitoring and Telemedicine:
Technological advances enable continuous monitoring of cardiac function through wearable devices and telemedicine, allowing for timely interventions and improved management of chronic conditions.
By integrating lifestyle modifications, pharmacologic therapies, interventional procedures, and emerging innovations, a comprehensive treatment plan can be tailored to meet the unique needs of each patient, ensuring effective management and improved heart health.
Nutritional Strategies & Supplements for Heart Health
Nutrition plays a fundamental role in maintaining a healthy heart. A balanced diet enriched with essential vitamins, minerals, and antioxidants can help regulate cholesterol, reduce inflammation, and improve overall cardiovascular function.
Key Nutrients for Cardiac Wellness
- Omega-3 Fatty Acids:
Found in fish oil, flaxseeds, and walnuts, omega-3 fatty acids help reduce triglycerides, lower blood pressure, and decrease inflammation. They support healthy blood vessel function and reduce the risk of arrhythmias. - Coenzyme Q10 (CoQ10):
CoQ10 is a vital antioxidant that aids in energy production within heart cells. Supplementing with CoQ10 may improve heart function, particularly in patients with heart failure or those taking statins. - Magnesium:
Magnesium is crucial for maintaining normal heart rhythm and muscle function. It helps lower blood pressure and prevent arrhythmias. Sources include leafy greens, nuts, seeds, and whole grains. - Vitamin D:
Adequate levels of vitamin D are linked to improved cardiovascular health. It helps regulate blood pressure, supports immune function, and may reduce the risk of heart disease. Sun exposure and fortified foods are primary sources. - Vitamin K2:
Vitamin K2 plays a role in calcium metabolism, directing calcium to the bones and away from the arteries, which may help prevent arterial calcification and improve heart health. - Fiber:
A high-fiber diet helps manage cholesterol levels and supports overall heart health. Whole grains, fruits, vegetables, and legumes are excellent sources of dietary fiber.
Herbal and Natural Supplements
- Garlic Extract:
Garlic has been shown to reduce blood pressure and cholesterol levels, as well as improve overall cardiovascular function. Its active compounds provide antioxidant and anti-inflammatory benefits. - Resveratrol:
Found in red grapes and berries, resveratrol is a polyphenol with antioxidant properties that may improve endothelial function and reduce inflammation.
Antioxidant Support
- Vitamin E:
An important antioxidant, vitamin E helps protect heart cells from oxidative damage. It works synergistically with other antioxidants to maintain cardiovascular health. - Alpha-Lipoic Acid:
This antioxidant supports energy production in cells and helps reduce oxidative stress, which can protect the heart from damage and improve overall function.
A heart-healthy diet supplemented with these key nutrients can significantly improve cardiovascular function, reduce the risk of heart disease, and support overall well-being.
Lifestyle Recommendations for a Healthy Heart
A heart-healthy lifestyle is essential for preventing cardiovascular disease and maintaining overall health. Adopting positive habits can reduce risk factors and improve the heart’s efficiency, ensuring that it meets the body’s demands effectively.
Dietary Practices
- Heart-Healthy Diet:
Consume a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated fats, trans fats, and excessive sodium to reduce the risk of coronary artery disease. - Moderate Alcohol Intake:
If you drink alcohol, do so in moderation, as excessive alcohol consumption can lead to high blood pressure and other heart-related issues.
Physical Activity
- Regular Exercise:
Aim for at least 150 minutes of moderate aerobic activity per week, along with strength training exercises. Regular exercise helps control weight, lowers blood pressure, improves circulation, and strengthens the heart muscle. - Incorporate Flexibility and Balance Exercises:
Activities such as yoga or tai chi not only reduce stress but also improve overall physical stability, which benefits heart health.
Stress Management
- Practice Mindfulness:
Techniques such as meditation, deep breathing, and mindfulness can reduce stress, which in turn lowers heart rate and blood pressure. - Maintain a Healthy Work-Life Balance:
Reducing stress through proper time management, hobbies, and adequate rest is crucial for long-term cardiovascular health.
Smoking Cessation
- Quit Smoking:
Smoking is a major risk factor for heart disease. Quitting smoking improves cardiovascular function almost immediately and significantly reduces the risk of heart attacks and strokes.
Regular Health Screenings
- Monitor Blood Pressure and Cholesterol:
Regular check-ups with your healthcare provider can help detect and manage high blood pressure and abnormal cholesterol levels before they lead to serious complications. - Routine Cardiac Evaluations:
Early detection of heart conditions through routine screening tests can lead to timely intervention and improved outcomes.
Weight Management
- Maintain a Healthy Weight:
Excess body weight places additional strain on the heart. Achieving and maintaining a healthy weight through a balanced diet and regular exercise can significantly lower the risk of cardiovascular disease.
Implementing these lifestyle recommendations can greatly enhance heart health, reduce the risk of disease, and contribute to overall longevity and quality of life.
Trusted Resources & Further Reading
Staying informed about heart health is essential for preventing and managing cardiovascular disease. The following resources offer reliable, up-to-date information and practical advice for maintaining a healthy heart.
Recommended Books
- “Prevent and Reverse Heart Disease” by Caldwell B. Esselstyn Jr.:
This book details a plant-based dietary approach to preventing and reversing heart disease, offering practical insights and scientific evidence. - “The Heart Health Bible” by John M. Kennedy:
A comprehensive guide that covers various aspects of heart health, including lifestyle modifications, dietary strategies, and medical treatments. - “The Great Cholesterol Myth” by Jonny Bowden and Stephen Sinatra:
Explores misconceptions about cholesterol and provides a detailed look at how dietary and lifestyle changes can improve cardiovascular health.
Academic Journals
- Journal of the American College of Cardiology (JACC):
A leading source of research on cardiovascular diseases, JACC provides cutting-edge studies and review articles on heart conditions, treatments, and prevention strategies. - Circulation:
Published by the American Heart Association, this journal features comprehensive research on heart disease and cardiovascular medicine, including the latest advancements in treatment and management.
Mobile Apps
- MyFitnessPal:
This app tracks diet and exercise, helping users maintain a heart-healthy lifestyle through nutritional monitoring and fitness tracking. - Cardiio:
Measures heart rate using your smartphone’s camera, offering insights into cardiovascular health and fitness levels. - Blood Pressure Monitor:
A useful app for tracking blood pressure readings, helping users manage hypertension and monitor heart health over time.
These trusted resources provide valuable information for both individuals and healthcare professionals seeking to enhance their understanding and management of heart health.
Frequently Asked Questions About the Heart
What is the primary function of the heart?
The heart is the central pump of the circulatory system. It continuously circulates blood, delivering oxygen and nutrients to tissues while removing waste products, thereby maintaining overall homeostasis and supporting vital bodily functions.
How does the heart regulate blood pressure?
The heart regulates blood pressure through its pumping action, while baroreceptors in the aorta and carotid arteries detect pressure changes and send signals to the brain, which adjusts heart rate and vascular tone accordingly.
What are common risk factors for heart disease?
Risk factors include smoking, high cholesterol, hypertension, diabetes, obesity, sedentary lifestyle, family history of heart disease, and poor dietary habits. Managing these factors is essential for preventing heart conditions.
How is heart disease diagnosed?
Heart disease is diagnosed using a combination of clinical evaluations, electrocardiograms (ECG/EKG), echocardiography, stress testing, cardiac catheterization, and advanced imaging techniques such as MRI and CT angiography.
What lifestyle changes can improve heart health?
Adopting a heart-healthy lifestyle involves eating a balanced diet, exercising regularly, quitting smoking, managing stress, maintaining a healthy weight, limiting alcohol consumption, and undergoing regular cardiovascular screenings.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about heart health and cardiovascular wellness.




