Choroideremia is a rare, inherited retinal disorder that affects countless individuals around the world. Characterized by progressive vision loss, this X-linked condition often starts with night blindness, followed by a gradual loss of peripheral vision. Ultimately, many patients face the severe threat of near-total blindness, typically by middle age. The culprit lies in a defective gene responsible for producing REP1 (Rab Escort Protein-1), a protein critical to the health and function of cells in the retina and choroid. Without a working copy of this gene, retinal cells cannot properly maintain the structures involved in visual processing and nourishment.
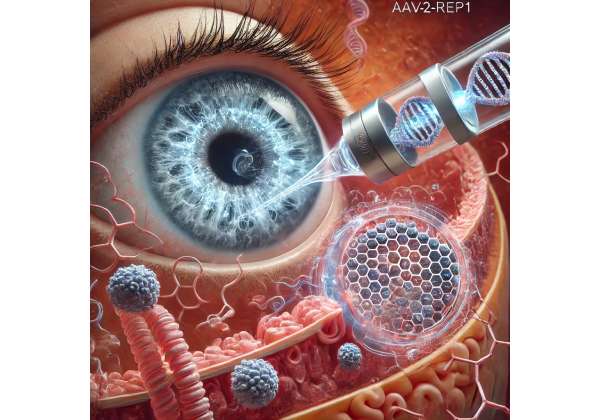
Over the years, scientists and clinicians have searched for ways to slow or halt disease progression. Traditional management has typically focused on supportive measures—such as low-vision aids or lifestyle adjustments—to help patients cope with diminishing sight. However, these approaches do not address the underlying genetic cause. Now, a new frontier in therapy has emerged in the form of gene replacement strategies. By leveraging a safe viral vector, like adeno-associated virus serotype 2 (AAV2), researchers can deliver a functional copy of the REP1 gene to the retina. This approach, commonly referred to as AAV2-REP1 therapy, offers renewed hope that patients may preserve functional vision far longer than previously considered possible. Below, we explore how this therapy works, what the most recent evidence reveals, how it is administered, and the potential costs of this groundbreaking intervention.
A Gene Therapy Breakthrough for Progressive Vision Loss
AAV2-REP1 therapy targets the root cause of choroideremia by providing a functioning version of the CHM gene (the gene encoding the REP1 protein). As an X-linked disorder, choroideremia predominantly affects males who inherit only one copy of the X chromosome. However, females carrying the mutation can sometimes experience mild symptoms due to X-inactivation or other genetic factors. Because the disease progresses steadily once it begins, gene therapy aims to intervene at a stage when enough viable retinal cells remain capable of taking up the therapeutic vector and producing the necessary protein.
Why the REP1 Protein Is Critical
Within the retina, cells called photoreceptors are chiefly responsible for detecting light and initiating the complex signaling that ultimately leads to visual perception. These cells rely on normal metabolic processes and protein transport to stay healthy. REP1 is involved in the prenylation of Rab GTPases—key molecules that help shuttle essential proteins and materials within cells. When REP1 is nonfunctional, this transport system falters. Over time, photoreceptors and the underlying retinal pigment epithelium (RPE) cells degrade, causing the characteristic symptoms of night blindness, tunnel vision, and eventual central vision loss.
The beauty of gene therapy lies in its ability to replace or restore the defective genetic information at the cellular level. By packaging a functional CHM gene into an AAV2 vector, clinicians strive to introduce a working blueprint for REP1 production directly to retinal cells. This means that, once inside the cell, the therapeutic gene can integrate—at least on an expression level—and direct the cell’s machinery to produce functional REP1, potentially halting or slowing the degenerative process.
How the AAV2 Vector Works
Adeno-associated viruses (AAV) have gained recognition in gene therapy largely due to their relatively mild immunogenicity and ability to infect non-dividing cells like neurons and photoreceptors. The AAV2 serotype, in particular, has been used extensively for ocular gene therapy trials, thanks to a strong safety record and specificity for retinal tissue.
Key attributes of AAV2-REP1 therapy include:
- Targeted Delivery: Delivered via a subretinal injection, the vector is placed close to the photoreceptors and RPE cells, maximizing transduction efficiency.
- Prolonged Expression: AAV2 vectors can remain active for years, making them an ideal candidate for treating chronic or degenerative conditions.
- Minimal Immune Response: While not entirely free of risks, AAV2 is typically less inflammatory than other viral vectors, reducing the likelihood of serious adverse events.
By restoring REP1, these cells theoretically regain the capacity for normal protein transport, thereby slowing further degeneration and possibly preserving existing photoreceptor function. While early intervention is often optimal, clinical trials have also included patients at more advanced stages, revealing varying degrees of success depending on disease severity.
Landmark Progress in Inherited Retinal Disease
AAV2-based therapies are not new to the eye care community. One high-profile example is Luxturna (voretigene neparvovec-rzyl), developed for certain forms of Leber’s congenital amaurosis (LCA). The success of that FDA-approved treatment proved that gene therapy could deliver long-term improvements in visual function for an inherited retinal disease.
In the context of choroideremia, AAV2-REP1 stands on a similar threshold of scientific enthusiasm. Indeed, it builds upon the same logic: fix the underlying gene to halt or slow the disease, rather than addressing symptoms or secondary complications. This approach exemplifies a wave of precision medicine strategies that aim to correct the root cause at a molecular level. By restoring a patient’s functional protein production, the hope is to maintain the structural integrity of the retina, forestalling blindness for years—and possibly decades.
Administering the AAV2-REP1 Approach: Key Steps
While the potential of gene therapy is transformative, successful outcomes hinge on properly executing each step in the procedural chain—from patient selection to post-operative care. AAV2-REP1 therapy is no exception, and patients considering it must understand both the complexity and the care required to maximize benefits.
Identifying Suitable Candidates
Because choroideremia typically manifests in childhood or adolescence with night blindness as an early sign, diagnosing the condition often involves clinical exams, genetic testing, and imaging studies such as optical coherence tomography (OCT) and fundus autofluorescence. Confirming a CHM mutation cements the diagnosis. Key considerations for AAV2-REP1 candidacy include:
- Extent of Retinal Damage: The therapy hinges on viable photoreceptors. If extensive degeneration has already occurred, the potential for significant functional gain or stabilization may be lower.
- Baseline Visual Function: Visual acuity, visual field measurements, and the presence or severity of night blindness can help predict treatment outcomes.
- Overall Health: Patients with significant immunological conditions or who cannot safely undergo ocular surgery may face contraindications.
- Age Factors: Although there is no strict upper age limit, younger individuals tend to have more robust retinal cells, possibly responding better to gene replacement.
Typically, an interdisciplinary team comprising a genetic counselor, a retinal surgeon, and medical specialists weighs these factors to decide if AAV2-REP1 is likely to be beneficial.
Subretinal Injection Procedure
The procedure itself involves delivering the therapeutic vector directly beneath the retina—a delicate process that demands surgical precision. The steps commonly include:
- Preoperative Prep: Patients may be administered local or general anesthesia. The surgeon and their team perform a final check of the ocular surface and anesthesia, ensuring that the eye is sterile and stable.
- Vitrectomy: Often, a pars plana vitrectomy is conducted first, removing the vitreous gel to provide clearer access to the subretinal space.
- Retinotomy: A tiny incision in the retina is made. Using a fine cannula, the surgeon injects a small volume of fluid containing the AAV2-REP1 vector into the subretinal space. This action creates a temporary retinal detachment or “bleb” that elevates the photoreceptor layer from the underlying retinal pigment epithelium.
- Vector Delivery: The virus-laden solution diffuses among the photoreceptors and RPE cells. Over time, cells internalize the viral particles, which deliver the functional REP1 gene.
- Closure and Recovery: After injection, the retina is allowed to settle. The surgeon may use gas or air within the vitreous cavity to support retinal reattachment, if necessary. Sutures are typically unnecessary for the microincisions made during vitrectomy.
Following the procedure, patients often remain under clinical observation for a few hours or overnight, depending on their health status and the surgeon’s protocol. Protective measures—such as eye shields—may be prescribed, and patients are instructed to avoid strenuous activities or actions that could elevate intraocular pressure.
Postoperative Monitoring and Care
Recovering from subretinal gene therapy involves multiple follow-up visits. Initially, these may occur within the first week, then monthly or at set intervals for up to a year or more. Key assessments include:
- Retinal Imaging: OCT scans help evaluate reattachment, measure thickness changes in the outer retina, and confirm that no adverse structural changes have occurred.
- Functional Tests: Visual acuity, color vision, and perimetry (visual field testing) track improvements or stabilization in the months following surgery. In some cases, specialized tests like microperimetry or electroretinography (ERG) might be employed.
- Inflammation and Immune Response: Some patients may require short-term topical or oral corticosteroids to manage inflammation. Monitoring for signs of an immune reaction to the AAV vector is critical, though clinically significant immune responses are rare.
- Lifestyle Guidance: Patients should report any sudden changes—like flashes of light, severe eye pain, or unusual floaters—as these can signal complications such as retinal detachment or infection.
Within a few months, many individuals notice improved light sensitivity or better maintained peripheral vision. However, results vary, and realistic expectations are vital. Some patients may experience minimal improvement yet still gain an advantage by slowing the natural progression of choroideremia.
Combining with Other Interventions
In some scenarios, AAV2-REP1 gene therapy may be integrated with additional ocular therapies or supportive strategies. For instance:
- Nutritional Support: Though not a cure, certain diets rich in antioxidants or omega-3 fatty acids may benefit overall retinal health.
- Low-Vision Aids: Devices like magnifiers, contrast-enhancing eyewear, and orientation training still play a valuable role, particularly for individuals with advanced disease stages.
- Future Retinal Prosthetics: Should disease progress in areas not treated by gene therapy, some may explore emerging solutions like retinal implants—though these remain a niche.
Importantly, gene therapy does not reverse all damage accrued over years of degeneration. Instead, it seeks to maintain or bolster the function of cells that remain viable. The precision of subretinal injection, the timing of intervention, and the individual’s baseline health all intertwine to shape final outcomes.
Cutting-Edge Evidence and Clinical Trials
Gene therapy for choroideremia has evolved rapidly from concept to clinic. Early success stories, though small in scale, galvanized broader international research. At present, a diverse array of clinical trials, observational studies, and real-world reports continue to amass data on the safety, efficacy, and durability of AAV2-REP1 interventions. Understanding these findings is key to grasping both the promise and the limitations of the treatment.
Early Proof-of-Concept Findings
Pioneering work on AAV2-REP1 therapy emerged from academic institutions such as the University of Oxford, where the first-in-human trials demonstrated encouraging results. These initial Phase I/II studies reported:
- Improved Visual Function: Some participants gained light sensitivity or improved visual acuity in treated areas, which was especially notable given that choroideremia typically shows steady deterioration.
- Safety and Tolerability: Adverse events were generally limited to low-grade inflammation or mild post-surgical complications, suggesting that the therapy was relatively safe.
- Sustained Expression: Follow-up examinations indicated that viral-mediated gene expression endured over time, a critical factor in maintaining the REP1 protein and forestalling disease progression.
Given these outcomes, more extensive trials were launched to verify results across a larger and more diverse patient population, including those at varied disease stages.
Multi-Center Trials and Extended Follow-Up
Subsequent studies involving multiple centers have reinforced the notion that AAV2-REP1 therapy can preserve vision. Key highlights include:
- Durable Effects: Some participants show stable or improved function up to several years post-treatment. Although not universal, the trend has been significantly more positive than typical choroideremia trajectories.
- Favorable Safety Profile: Larger cohorts confirm that serious complications—such as uncontrolled intraocular inflammation, vector-related toxicity, or severe retinal damage—remain infrequent. Mild, transient inflammatory responses were the most common concern.
- Dose Optimization: Studies have explored different vector concentrations. Higher-dose regimens sometimes yield more robust efficacy but can marginally increase inflammation risk. Refining the balance between dose and safety remains a priority.
In these trials, advanced imaging techniques have shed light on subtle anatomical changes. For instance, many participants maintain better-preserved photoreceptor layers around the injection site, underscoring that gene therapy may physically protect and nourish the retina. This is particularly meaningful in choroideremia, where thinning of retinal layers is often relentless.
Real-World Data and Observational Reports
While controlled clinical trials are essential, real-world implementations add depth to our understanding. Some patients who participated in early trials are now nearing the five-to-ten-year mark post-injection. Retrospective analyses of their progress indicate that:
- Progression Slows: Even if not halted entirely, the degenerative process appears significantly delayed compared to natural history.
- Quality of Life Gains: Some individuals report improvements in daily tasks like reading, recognizing faces, or navigating in dimly lit environments.
- Variability in Outcome: Just as with other gene therapies, no universal blueprint guarantees uniform results. Differences in injection technique, disease stage, immune responses, and genetic background can shape each person’s trajectory.
Additional studies are investigating whether a second injection—either into different retinal regions or a re-administration in the same area—could extend benefits further. At this stage, re-dosing remains a gray area, as researchers strive to better understand immune system interactions and the diminishing returns that might arise if large swaths of the retina have already deteriorated.
Next Phases and Ongoing Inquiries
The mission to perfect AAV2-REP1 therapy continues. Active research agendas encompass:
- Combination Therapies: Co-administering neuroprotective agents or anti-inflammatory drugs alongside the vector to enhance cellular survival.
- Alternative Delivery Modes: Exploring whether less invasive injection routes, like suprachoroidal delivery, might still adequately target photoreceptors while simplifying the surgical process.
- Long-Term Safety: Monitoring for delayed complications remains critical, as gene therapies are still relatively new in the broader context of medical history.
- Genetic Modifiers: Investigations into secondary genetic factors that influence individual responses to therapy, aiming to personalize and optimize outcomes.
Since the retina is a relatively immune-privileged site compared to the rest of the body, the majority of evidence suggests that AAV-mediated gene therapy retains a high margin of safety. Researchers and clinicians remain driven to ensure that all relevant parameters—dose, vector design, surgical nuance—are refined before scaling up availability.
Overall, the trajectory for AAV2-REP1 in choroideremia is highly optimistic. Each layer of evidence—ranging from small pilot studies to more extensive multi-year trials—reinforces the notion that we can manipulate the genetic underpinnings of retinal disease and positively alter patients’ quality of life.
Evaluating Benefits and Potential Risks
Like any pioneering medical intervention, AAV2-REP1 therapy carries both promise and uncertainties. For patients confronting a life-altering disease like choroideremia, balancing the potential for extended vision against the inherent risks of gene therapy is a critical aspect of informed decision-making. Drawing on aggregated data from research centers, trial results, and clinical observations, we can illuminate both the therapy’s advantages and its cautionary points.
Confirmed Advantages
- Disease Modification: Unlike existing supportive measures, AAV2-REP1 directly tackles the genetic defect underlying choroideremia. By delivering a functional copy of the CHM gene, the therapy addresses the disease’s root cause, providing a chance to significantly slow—or in some cases partially reverse—retinal degradation.
- Preservation of Photoreceptors: The therapy often aims to stabilize or even modestly improve visual function, especially if administered before advanced atrophy sets in. Patients report enhanced clarity in low-light settings, expanded or better-maintained peripheral fields, and sometimes improved acuity.
- Long-Lasting Effect: AAV vectors generally provide sustained transgene expression. If successful, a single surgical injection could offer benefits spanning multiple years, diminishing the need for repeated treatments.
- Safety Record: Although no therapy is entirely free of risk, experiences across numerous AAV-based retinal trials suggest a favorable safety profile. Serious complications, like uncontrollable inflammation or substantial vision loss induced by the therapy itself, remain rare.
From a patient’s perspective, the possibility of preserving independence—driving longer, sustaining employment, or simply recognizing loved ones’ faces—represents a profound psychological and practical benefit.
Potential Drawbacks and Risks
Despite its many merits, AAV2-REP1 has limitations and potential dangers that warrant discussion:
- Surgical Complexity: Subretinal injections are intricate procedures. There is a small but real risk of retinal detachment, hemorrhage, or infection. Skilled surgeons minimize these complications, yet they cannot be wholly eliminated.
- Inflammatory Response: Even mild immune reactions can disrupt retinal cells. Post-operative care often involves monitoring for signs of uveitis or choroiditis, which may require corticosteroids or immunomodulators.
- Limited Window of Efficacy: If the disease has advanced considerably and only a narrow ring of viable retina remains, the therapy’s impact may be modest. Timing and baseline retinal health significantly influence outcomes.
- Individual Variability: Genetic differences, immune profiles, and technical nuances (such as injection site) can result in heterogeneous responses. While many see improvement or stabilization, a subset may gain less significant benefit.
- Unknown Long-Term Outlook: Current data on durability stretch only into the five-to-ten-year range. Lifelong monitoring is necessary to confirm whether improvements endure and to track any late-arising adverse events.
A balanced view acknowledges that gene therapy is inherently complex, and not all individuals qualify or can manage the intricacies of the procedure and follow-up. However, for those who do meet the candidacy requirements, the chance at preserving functional vision often outweighs the enumerated risks.
Strategies to Minimize Complications
Clinical best practices have emerged to reduce complications and enhance success:
- Rigorous Screening: Only patients with confirmed CHM mutations and sufficient intact retina for transduction are selected.
- Gradual Post-Operative Steroid Taper: This approach helps regulate inflammation without compromising the vector’s efficacy.
- Standardized Surgical Protocols: Trained vitreoretinal specialists follow careful injection procedures, often developed and refined through multi-center trials.
- Close-Interval Monitoring: Frequent evaluations in the immediate postoperative months catch early signs of complications, which can often be managed conservatively if addressed promptly.
By following these guidelines, many patients experience a relatively smooth recovery phase, giving the therapy the best chance to integrate at the cellular level and deliver the sought-after benefits.
Cost Considerations for AAV2-REP1 Treatment
Prices for gene therapies can be significant, reflecting years of research, specialized manufacturing processes, and the complexity of surgical delivery. Depending on the specific healthcare system, total costs may range from tens of thousands to several hundred thousand dollars. Some centers bundle surgical fees, hospitalization, and follow-up care into a single package, while others separate each component. Insurance coverage varies widely, with certain policies offering partial reimbursement if gene therapy is deemed medically necessary and meets predefined criteria. Patients may also find assistance through clinical trials, philanthropic organizations, or special payment plans that mitigate out-of-pocket expenses.
Disclaimer: This article is for educational purposes only and does not replace professional medical advice. Always consult with a qualified healthcare provider to determine the best treatment options for your specific condition.
We invite you to share this article on Facebook, X (formerly Twitter), or your preferred social media platforms. By spreading the word, you can help raise awareness of AAV2-REP1 therapy and provide hope to others facing choroideremia or similar genetic retinal diseases.