Central retinal artery occlusion (CRAO) is one of the most urgent ophthalmic emergencies, often resulting in sudden and profound vision loss. Because the central retinal artery is the primary blood supply to the retina, any blockage can deprive this light-sensitive layer of the oxygen and nutrients it needs for proper function. Patients and healthcare providers alike face an immense challenge in preserving vision once a CRAO has occurred. Traditional interventions may include lowering intraocular pressure or attempting to dislodge the clot, but their success rates vary, and prompt action is paramount. Against this backdrop, hyperbaric oxygen therapy (HBOT) is steadily gaining recognition as a potential game-changer in preserving and possibly restoring visual function following a CRAO event.
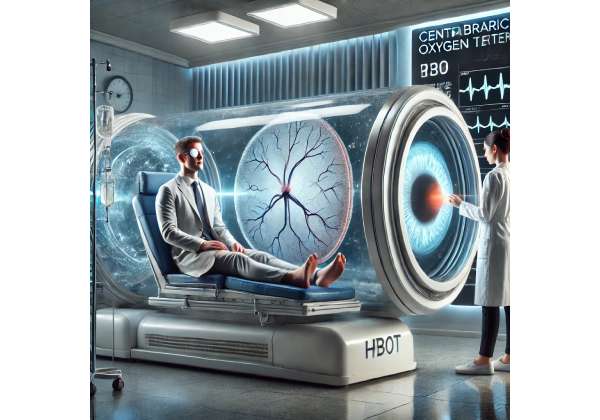
Hyperbaric oxygen therapy involves placing a patient in a specialized chamber where the atmospheric pressure is elevated above normal levels. This environment allows the lungs to absorb significantly more oxygen than under standard conditions. Enhanced oxygen delivery has shown promise in various ischemic conditions—ranging from diabetic foot ulcers to gas gangrene—and now ophthalmologists and hyperbaric specialists are exploring its applicability for central retinal artery occlusion. Although more research is needed to standardize protocols and pinpoint the exact treatment window, preliminary data and clinical anecdotes suggest that HBOT could offer an important lifeline when every minute matters. Below, we delve into key aspects of this therapy, from fundamental principles and protocols to emerging studies and pricing details, all focused on how hyperbaric oxygen therapy can save your vision from CRAO.
Understanding Hyperbaric Oxygen for Sudden Vision Loss
Hyperbaric oxygen therapy, commonly abbreviated as HBOT, represents a treatment modality in which patients breathe almost pure oxygen in an environment that is approximately 1.5 to 3 times normal atmospheric pressure. The fundamental idea is to increase oxygen saturation in the blood, thereby delivering more oxygen to tissues experiencing hypoxia or compromised blood flow. For conditions like central retinal artery occlusion, where an arterial blockage starves the retina of vital nutrients, enhanced oxygen availability can potentially limit permanent damage.
The Physiological Rationale
When you enter a hyperbaric chamber, the pressure differential causes more oxygen molecules to dissolve directly into the plasma portion of your blood. Red blood cells are not the only carriers of oxygen in this pressurized scenario—your plasma becomes an additional vehicle. Because central retinal artery occlusion obstructs normal blood flow, boosting plasma oxygen content may help circumvent the blockage and support the damaged retinal cells temporarily. Even if the principal artery remains occluded, the retina might access oxygen through smaller collateral vessels, buying critical time to avert irreversible loss of photoreceptor function.
Studies in hyperbaric medicine highlight several mechanisms through which HBOT can be beneficial:
- Elevated Tissue Oxygenation: By increasing partial pressure of oxygen in the bloodstream, HBOT helps tissues that are otherwise deprived.
- Reduced Edema: High oxygen levels can cause vasoconstriction in healthy blood vessels, reducing swelling but not depriving tissues of oxygen because of the increased oxygen-carrying capacity. For the retina, controlling edema is crucial in preserving structural integrity.
- Promotion of Angiogenesis: Over longer therapy courses, elevated oxygen pressures may encourage the formation of new blood vessels, which could prove advantageous if the primary artery remains partially blocked.
Brief History and Current Uses
While hyperbaric oxygen therapy has its roots in the early 20th century, it became more formally recognized in the mid-1900s. Initially employed for conditions such as decompression sickness in divers, the therapy later expanded to treat carbon monoxide poisoning, necrotizing fasciitis, diabetic wounds, and more. Over the decades, clinicians and researchers discovered that some of the same principles aiding divers and burn victims could also apply to certain eye disorders.
Although the eye has distinctive physiological and anatomical features, the retina is comparable to neural tissue in terms of its high oxygen demand. A CRAO event has been likened to a “stroke” in the eye—tissues downstream from the blockage begin to die off if oxygen is not restored quickly. Traditional stroke management has only partial overlap with CRAO treatments, owing to differences in vascular architecture and accessible interventions. Nonetheless, hyperbaric oxygen therapy has emerged as a method to elevate local oxygen levels, a principle similarly valued in acute stroke management and traumatic brain injury.
Timelines and Urgency
Timing is critical in CRAO. Many ophthalmologists adopt the phrase “time is retina,” akin to the stroke community’s “time is brain.” Animal models and clinical evidence consistently show that the longer the retina remains without adequate oxygen, the higher the likelihood of irreversible damage. Some case reports suggest that HBOT may still offer marginal benefits if initiated within 24 to 48 hours after symptom onset, but the conventional wisdom is that the best possible visual outcomes are more likely if therapy is started within a few hours of occlusion.
For instance, when a patient presents with sudden painless vision loss, immediate steps—such as ocular massage or administering drugs to lower intraocular pressure—are frequently undertaken while the medical team coordinates potential HBOT. In some centers, direct referral to a hyperbaric facility is considered standard if the patient qualifies and the time window is feasible.
Understanding the Treatment Session
In hyperbaric treatment for CRAO, the patient is taken to a hyperbaric chamber (either a monoplace or multiplace chamber) where the pressure is raised to between 1.5 and 2.5 times normal atmospheric pressure. They breathe pure or near-pure oxygen through a mask or hood, depending on the chamber’s design. Sessions can last between 60 and 90 minutes, and multiple sessions over consecutive days may be recommended for optimal results. While many protocols vary, some clinics adhere to daily or twice-daily HBOT sessions for several days following the initial occlusive event.
During the session, patients often experience a mild sensation of fullness in the ears, similar to ascending or descending in an airplane. Trained staff continuously monitor vital signs and watch for possible complications, such as ear barotrauma. In large multiplace chambers, there is room for medical personnel to remain present, further enhancing patient safety.
Potential Role in Vision Preservation
Though hyperbaric oxygen therapy cannot guarantee a full restoration of sight, its ability to mitigate the progression of retinal damage is noteworthy. Even modest visual improvements could substantially impact a patient’s quality of life, allowing tasks like reading, navigating familiar spaces, or recognizing faces. With CRAO often resulting in severely reduced visual acuity or even counting fingers at close range, any intervention that might salvage even partial function can be life-altering.
Still, HBOT is not universally accessible, and its role in CRAO treatment remains under debate in some medical circles. Large-scale randomized controlled trials are relatively scarce, and logistical constraints—such as cost and availability of hyperbaric facilities—can limit its widespread adoption. Nevertheless, many clinicians who have witnessed positive patient outcomes view HBOT as an invaluable option in the therapeutic arsenal against CRAO.
By increasing oxygen supply to the starving retina, hyperbaric therapy seeks to preserve cellular metabolism and stave off irreversible death of photoreceptors. When viewed in tandem with other emergency measures, it may form part of a multifaceted approach to a condition where time is of the essence.
Practical Steps for Incorporating Hyperbaric Oxygen in CRAO Care
As central retinal artery occlusion stands as an acute and sight-threatening condition, integrating hyperbaric oxygen therapy into its management demands swift, well-coordinated action. The journey from an ophthalmologist’s diagnosis to a hyperbaric facility can be time-sensitive. Below is a step-by-step outline that highlights the necessary steps and protocols to ensure patients receive timely, effective care.
Step 1: Immediate Recognition and Referral
When a patient presents with sudden, painless visual loss, an ophthalmologist typically looks for the classic fundoscopic signs of CRAO, such as a pale retina with a cherry-red spot at the macula. Concurrently, the physician may apply first-line measures:
- Ocular Massage: This gentle yet brisk pressure aims to dislodge the embolus.
- Intraocular Pressure Reduction: Medication or paracentesis (deliberate removal of a small volume of aqueous humor) may be employed to lower intraocular pressure, encouraging blood flow.
- Breathing into a Paper Bag (Rarely Advised): Historically, this was thought to elevate arterial CO₂, dilating retinal vessels, though its efficacy is debated.
If these measures do not yield a rapid restoration of vision, the ophthalmologist may recommend a consult with a hyperbaric specialist. Because the clinical window is narrow, an established referral network is vital. Many hospitals that have hyperbaric chambers operate 24/7, but not all do, making advanced planning crucial.
Step 2: Assessing Patient Suitability
Before initiating hyperbaric oxygen therapy, a quick but thorough evaluation is required to ensure the patient can safely tolerate increased atmospheric pressure and high levels of oxygen. Key considerations include:
- Underlying Lung Conditions: Certain disorders like chronic obstructive pulmonary disease (COPD) can predispose individuals to air trapping and potential barotrauma.
- Ear, Sinus, and Dental Health: Pressure changes can be painful or harmful if the Eustachian tubes, sinuses, or dental structures have issues.
- Claustrophobia: Some patients find enclosed hyperbaric chambers uncomfortable, though sedation or larger multiplace chambers can mitigate this problem.
- Cardiac Stability: Patients with cardiac arrhythmias or recent heart procedures should be reviewed by a cardiologist to confirm their ability to undergo increased atmospheric pressure.
None of these factors absolutely contraindicate therapy, but they need to be accounted for and managed appropriately. If the patient is deemed suitable, they can proceed to the next stage.
Step 3: Chamber Type and Pressure Settings
Hyperbaric oxygen therapy commonly occurs in two basic configurations:
- Monoplace Chambers: Designed for a single patient, these are often made of clear acrylic, allowing visual monitoring from the outside. The entire chamber is pressurized with oxygen.
- Multiplace Chambers: Large enough to house multiple patients or a patient plus medical personnel. In these facilities, the chamber is typically pressurized with air, while the patient receives near-pure oxygen via a mask, hood, or endotracheal tube if intubated.
For CRAO, pressures typically range between 1.5 and 2.5 ATA (atmospheres absolute). The precise setting may vary based on local protocols, patient tolerance, and the severity of the retinal occlusion. Once inside the chamber, the pressure is gradually increased, usually over the course of several minutes, to help the patient’s body adapt.
Step 4: Duration and Frequency of Treatments
Optimal duration and frequency of HBOT sessions for CRAO are not universally standardized, primarily due to limited large-scale studies. However, common practice involves:
- Initial Intensive Phase: One or two sessions per day for the first three to five days, each lasting 60 to 90 minutes.
- Extended Treatment: Additional sessions may be administered if the patient continues to show improvement or if the treating physician believes further gains could be achieved. Some protocols run for one to two weeks, tapering sessions as progress stabilizes.
Close ophthalmologic follow-up is vital throughout this process. Vision tests—such as checking visual acuity, pupil reactivity, and retinal imaging—can help gauge the therapy’s effectiveness and guide decisions about when to modify or discontinue HBOT.
Step 5: Combining HBOT with Adjunctive Therapies
Most ophthalmologists agree that hyperbaric oxygen therapy should not be the sole approach in managing CRAO. Instead, it functions best as a complement to other interventions:
- Thrombolytics or Anti-Platelet Agents: In select cases, systemic or local administration of clot-busting drugs may be considered, although more common in stroke management than in routine CRAO care.
- Vasodilators: Certain topical or systemic agents could aid in dilating retinal vessels, though evidence for their efficacy remains mixed.
- Nutritional and Supportive Measures: Ensuring optimal hydration and controlling systemic factors—like hypertension or diabetes—is critical in overall recovery and prevention of further embolic events.
In some hospitals, a dedicated stroke or vascular team might evaluate CRAO patients for possible underlying conditions, such as carotid artery disease or cardiac sources of emboli. Collaboration among specialties ensures a comprehensive approach that addresses the root causes of the occlusion while simultaneously working to preserve existing vision.
Step 6: Monitoring, Patient Education, and Rehabilitation
Post-therapy, patients require periodic check-ups with both the hyperbaric team and the ophthalmologist. Assessments may include:
- Optical Coherence Tomography (OCT): Provides detailed cross-sectional images of the retina to detect swelling or structural changes.
- Visual Field Testing: Determines whether the visual field is expanding, stabilizing, or further declining.
- Fundus Photography: Allows clinicians to track changes in the retinal appearance over time.
Beyond clinical monitoring, patient education is crucial. Individuals who have experienced a CRAO often have significant cardiovascular or systemic risk factors that need addressing. Lifestyle changes, medication regimens, or further medical evaluations may be necessary to reduce the chances of another vascular event. In addition, low-vision rehabilitation can help patients adapt to any persistent visual deficits, improving their day-to-day functioning.
Potential Challenges
Although the effectiveness of hyperbaric oxygen therapy for CRAO has shown promise, several practical barriers exist:
- Geographical Limitations: Access to a hyperbaric chamber might be limited, particularly in rural or remote areas.
- Financial Constraints: Insurance coverage can vary, and out-of-pocket costs can be high if coverage is lacking (discussed more in a later section).
- Lack of Standardized Protocols: Without large-scale randomized studies, recommended pressures, session lengths, and treatment durations can differ from one center to another.
Despite these hurdles, more eye centers and emergency departments are forging partnerships with hyperbaric units to streamline care. When orchestrated effectively, hyperbaric oxygen therapy can be woven into the broader tapestry of urgent interventions for central retinal artery occlusion, potentially alleviating what might otherwise be a devastating visual outcome.
Recent Clinical Research on Hyperbaric Oxygen and Retinal Outcomes
Evidence supporting hyperbaric oxygen therapy for central retinal artery occlusion is steadily accumulating, though the field still craves larger, high-quality studies to establish definitive guidelines. Existing research comprises case reports, retrospective reviews, and smaller prospective studies that collectively highlight the potential merits—and limitations—of HBOT in retinal emergencies. Below is a synthesis of the most compelling research findings shaping current understanding.
Notable Case Reports and Observational Studies
One of the pivotal ways researchers have investigated HBOT for CRAO is through in-depth case reports. Multiple documented instances describe patients presenting with severe visual loss—sometimes as dire as hand motion perception—who achieved meaningful improvement after initiating hyperbaric sessions within hours of symptom onset. Many regained visual acuity to a level sufficient for reading or navigating without assistance. While case reports naturally lack the rigor of controlled trials, they do illustrate what is possible under optimal conditions.
Retrospective observational studies offer a broader lens on outcomes. In these analyses, hospital records of patients treated with HBOT for CRAO are reviewed for changes in visual acuity or visual fields over time. One such study showed that patients receiving hyperbaric therapy within 24 hours of occlusion onset had better final vision compared to those who started therapy later. Nevertheless, these retrospective designs can be confounded by variations in initial visual acuity, coexisting medical conditions, and differences in HBOT protocols.
Mechanistic Insights from Animal Models
Complementing clinical data, animal research has helped elucidate how hyperbaric oxygen might protect the retina. In certain animal models, artificially induced retinal artery occlusions allowed scientists to manipulate different oxygen pressures and measure the resulting cellular and molecular changes. Consistent findings include reduced apoptosis (cell death) in photoreceptors and preservation of retinal structure on histological examination. These studies suggest that hyperbaric oxygen’s main advantage lies in sustaining the metabolic demands of retinal tissue during occlusion, minimizing irreversible damage.
Animal studies also highlight a potential role for delayed treatment: in some scenarios, partial functional recovery is observed even if hyperbaric therapy starts several hours after artery blockage. This aligns with clinical observations indicating that while earlier is unequivocally better, some salvage may still be possible if the therapy is not initiated immediately.
Emerging Data from Prospective Trials
Though still limited, certain centers are undertaking prospective clinical trials to systematically document the benefits of HBOT for CRAO. These trials recruit patients soon after diagnosis, then randomly assign them to either conventional therapy—like ocular massage, intraocular pressure reduction, and observation—or the same conventional therapy plus hyperbaric oxygen sessions. By following participants over weeks to months, these studies track changes in best-corrected visual acuity and visual fields. Preliminary findings from smaller-scale endeavors often demonstrate at least some degree of improved final vision in the HBOT group, though the number of participants is typically small.
Another focus of emerging research is the synergy between hyperbaric oxygen and adjunct treatments. For example, a few trials are exploring whether combining HBOT with intravenous tissue plasminogen activator (tPA) or antiplatelet medications can further boost visual recovery by dissolving or preventing clots while simultaneously improving oxygen delivery. Early data hint at possible benefits, but the risks—such as bleeding complications—must be carefully balanced.
The Debate on Efficacy
Hyperbaric oxygen therapy for CRAO remains a subject of debate among clinicians. Skeptics argue that the retina’s specialized circulation might limit how effectively increased oxygen diffuses to the ischemic area, especially when the central artery is severely blocked. They also point out the scarcity of large, randomized trials to definitively prove causation rather than mere correlation between HBOT and vision improvement.
Proponents, however, emphasize the therapy’s relatively favorable safety profile and the logical physiological basis for its use. They argue that in the absence of other consistently effective treatments, hyperbaric oxygen stands out as a reasonable and potentially impactful intervention. Many practicing ophthalmologists and hyperbaric specialists cite not only the growing body of literature but also anecdotal reports of saved vision in patients considered prime candidates for therapy—particularly those who arrive at a hyperbaric center within a few hours of symptom onset.
Where the Research Is Headed
As interest in hyperbaric oxygen therapy for CRAO grows, researchers are likely to focus on:
- Larger, Multicenter Trials: Collaborations among hospitals and hyperbaric facilities could pool resources to enroll enough patients for statistically robust evaluations.
- Optimizing Treatment Parameters: By testing different pressure levels, session lengths, and frequencies, investigators aim to clarify the “best” approach for CRAO.
- Biomarkers and Imaging: Advanced imaging techniques, including functional MRI for the retina, might shed light on the microcirculatory changes occurring during and after HBOT. Understanding these nuances could help refine patient selection and predict outcomes.
Though the scientific community eagerly awaits more definitive data, current evidence—both clinical and laboratory-based—lends credibility to the idea that hyperbaric oxygen can be a worthwhile component of a CRAO treatment strategy. Until large trials provide more clarity, most clinicians will continue to rely on existing research, practical experience, and the individual circumstances of each patient when recommending HBOT.
Safety Standards and Proven Efficacy of Treatment
When it comes to preserving sight in the face of central retinal artery occlusion, safety and efficacy are the two main pillars that guide clinical decision-making. As a high-stakes intervention, hyperbaric oxygen therapy must be scrutinized not only for its life-enhancing benefits but also for potential risks. Below is an in-depth look at the safety profile and documented efficacy of this treatment in the context of CRAO.
Key Safety Considerations
Like any medical procedure, hyperbaric oxygen therapy can have side effects or complications, although serious adverse events are uncommon when performed in accredited centers under professional supervision.
- Barotrauma: Increased pressure can harm air-filled spaces in the body, most commonly affecting the ears and sinuses. Patients may experience ear pain or, in rare instances, a ruptured eardrum if pressure equalization techniques (like swallowing or yawning) are inadequate. Barotrauma can extend to the lungs, but this is far less frequent and typically associated with underlying lung pathology.
- Oxygen Toxicity: Breathing nearly pure oxygen at elevated pressures for prolonged periods can lead to pulmonary or central nervous system (CNS) oxygen toxicity. Symptoms might include chest discomfort, coughing, or even seizures in extreme cases. However, following established time and pressure protocols substantially reduces this risk.
- Claustrophobia and Anxiety: Some patients feel anxious in confined spaces, especially in monoplace chambers. When necessary, mild sedation or the use of larger multiplace chambers can address this concern.
- Hypoglycemia in Diabetic Patients: Those on insulin or other glucose-lowering medications may see blood sugar fluctuations in a high-oxygen environment. Close monitoring is essential.
Most hyperbaric clinics employ dedicated safety measures such as continuous patient observation, adherence to established treatment profiles, and pre-treatment evaluations to identify individuals at higher risk of complications. Accreditation bodies, like the Undersea and Hyperbaric Medical Society (UHMS) in the U.S., set guidelines that facilities must follow to maintain a safe environment.
Documented Efficacy in Vision Restoration
Although hyperbaric oxygen therapy is not universally considered a standard for CRAO, multiple lines of evidence support its role in improving visual outcomes for select patients:
- Early Intervention Success: Prospective and retrospective data indicate that starting HBOT within a short window—often cited as two to 12 hours after onset—correlates with better recovery. Improved best-corrected visual acuity and field expansion have been reported, sometimes allowing patients to resume tasks they previously could not perform.
- Partial Salvage of Vision: Even in cases where complete restoration is not achievable, partial improvement can be meaningful. Gaining the ability to read larger print or detect movement can significantly enhance a patient’s independence and reduce reliance on assistive devices.
- Mechanistic Plausibility: Beyond clinical data, the physiological underpinnings—boosted oxygen delivery, potential angiogenesis, and reduced edema—support the idea that hyperbaric therapy aids retinal survival in ischemic conditions.
- Synergistic Use with Other Modalities: Some centers combine HBOT with other approaches like intra-arterial fibrinolysis (in highly selected cases) or even ocular interventions. Although the evidence base for combination treatments is still emerging, preliminary reports indicate they could further augment visual recovery.
Special Populations
Certain demographic groups and health conditions require extra caution:
- Elderly Patients: Senior patients often present with multiple comorbidities (e.g., hypertension, arteriosclerosis). While they can benefit from HBOT, thorough cardiac and pulmonary assessments are essential.
- Pediatric Cases: CRAO is rarer in children, but protocols must be adapted to their smaller body size and distinct physiological responses. Pediatric hyperbaric specialists oversee these treatments.
- Pregnant Women: In general, hyperbaric oxygen therapy for pregnant patients is approached conservatively. However, emergent situations—such as severe carbon monoxide poisoning—have justified its use. For CRAO, the treating physician must carefully weigh the risks and benefits, although reports of CRAO in pregnancy are extremely rare.
Comparing HBOT to Other Interventions
Conventional CRAO management includes interventions like digital ocular massage, IOP-lowering medications, and vasodilators. While these measures may help shift the embolus or reduce oxygen demand, they do not directly address the retina’s urgent need for more oxygen. By contrast, hyperbaric oxygen directly raises tissue oxygen levels, providing a potential means to keep cells viable for longer.
Some clinicians have also explored intra-arterial thrombolysis, an invasive approach involving catheter-guided administration of clot-busting agents directly into the ophthalmic artery. Though theoretically promising, the procedure carries risks like intracranial hemorrhage. Given HBOT’s comparatively benign safety profile, many providers see it as a less invasive, lower-risk option, albeit with an uncertain—but often favorable—magnitude of benefit.
Long-Term Outcomes and Follow-up
Because CRAO can be accompanied by systemic health issues—such as carotid artery disease or cardiac arrhythmias—long-term success extends beyond merely recovering partial eyesight. Regular follow-up visits and comprehensive care from cardiologists, neurologists, and vascular surgeons may be necessary to avert recurrent ocular or cerebral vascular events. From an ophthalmic standpoint, ongoing monitoring with tests like optical coherence tomography (OCT) or fundus fluorescein angiography (FFA) can help track any late-stage complications, including neovascularization of the retina or optic nerve head.
In terms of visual recovery stability, many patients who demonstrate improvement with HBOT maintain at least part of these gains. That said, the extent of improvement can vary, ranging from mild gains in acuity to marked restoration. Establishing precise prognostic factors—age, underlying disease, duration of occlusion, and presence of embolic sources—remains a work in progress.
The consensus among practitioners who have integrated hyperbaric oxygen therapy into CRAO management is that while no single method can guarantee a return to full normal vision, HBOT stands as a valuable tool in the treatment repertoire. Its strong safety record, coupled with credible evidence for visual rescue in emergent occlusions, underlines its growing acceptance in ophthalmic and hyperbaric circles.
Cost Considerations for Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy for central retinal artery occlusion can vary greatly in price, ranging from several hundred to a few thousand dollars per session. Costs often depend on the type of chamber used, whether the facility operates 24/7 for emergencies, and local insurance or government reimbursement policies. Some private clinics offer package deals with multiple sessions at discounted rates, whereas hospital-based programs may charge on a per-session basis. Many insurance providers cover at least part of the expense if HBOT is deemed medically necessary, though coverage details differ widely. Patients are advised to contact their insurer or local hyperbaric center to determine out-of-pocket costs before starting therapy.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or treatment.
We warmly encourage you to share this article with friends, family, or online groups that could benefit. Feel free to use our Facebook and X (formerly Twitter) share buttons, or any preferred social platforms, to help spread awareness about hyperbaric oxygen therapy for central retinal artery occlusion!










