Stargardt disease is an inherited retinal disorder that leads to progressive vision loss, most notably affecting the macula, the central region of the retina responsible for sharp, detailed sight. Patients commonly experience a gradual decline in their ability to see fine detail and color, significantly impacting daily activities like reading or recognizing faces. Caused by mutations in genes such as ABCA4, Stargardt disease triggers the accumulation of toxic byproducts in the retinal cells and particularly harms the delicate retinal pigment epithelium (RPE). While there are several approaches to manage the condition, including vitamin supplementation and low-vision aids, these measures often only ease the symptoms rather than halt the degenerative process itself.
Emerging science, however, is painting a more optimistic picture. Stem cell therapy focusing on RPE cells is opening new avenues for treating Stargardt disease at its core. By renewing or replacing the compromised RPE, clinicians and researchers aim to improve retinal function, slow degeneration, and potentially restore aspects of lost vision. This innovative therapeutic concept leverages breakthroughs in stem cell biology to better preserve the retina’s structure and function, offering hope to patients who previously had limited treatment options. In the coming sections, we take a closer look at how RPE-focused stem cell therapy may bring significant progress for Stargardt disease management.
Insights into a Promising Cellular Therapy for Vision Restoration
Stargardt disease poses a unique challenge for eye specialists due to the dysfunctional process that specifically targets the macula’s RPE layer. The retinal pigment epithelium supports photoreceptor cells (the rods and cones) through essential roles such as nutrient delivery, phagocytosis of photoreceptor outer segments, and maintenance of the blood-retinal barrier. Once RPE cells start failing, it triggers a domino effect, gradually leading to the death of photoreceptors in the macula. This cascade diminishes patients’ central vision, making everyday tasks increasingly difficult.
The Rationale Behind Stem Cell Interventions
Stem cell therapy has garnered attention in multiple fields of regenerative medicine, but its application to eye disease, especially those involving the retina, is of particular interest. The premise is straightforward yet powerful: if the underlying pathology in Stargardt disease is the deterioration of RPE cells, then replacing them with healthy, functional equivalents could stabilize or regenerate retinal function. Stem cells—whether embryonic, induced pluripotent stem cells (iPSCs), or adult mesenchymal stem cells (MSCs)—can be guided to differentiate into RPE cells in vitro. These new, laboratory-grown RPE cells can theoretically be transplanted back into the subretinal space, where they could integrate and resume normal biological functions, nourishing photoreceptors and potentially slowing or halting disease progression.
Moreover, transplanted RPE cells may deliver benefits beyond mere replacement. There is evidence suggesting that transplanted cells can modulate the local environment by reducing inflammation and offering neuroprotective factors. Given that Stargardt disease can create a toxic environment laden with lipofuscin accumulation and oxidative stress, providing a more supportive local milieu could be as critical as the direct cell-replacement effect.
Comparing RPE Cell Sources
While the general concept of RPE transplantation is the same, the source of the transplanted cells can differ:
- Human Embryonic Stem Cells (hESCs): These are pluripotent cells capable of differentiating into virtually any cell type, including RPE. Researchers have used hESC-derived RPE in early clinical trials, observing varying degrees of success in halting degeneration or improving vision.
- Induced Pluripotent Stem Cells (iPSCs): Created by reprogramming adult somatic cells (like skin fibroblasts) into a stem-cell-like state, iPSCs can then be pushed toward RPE lineage. This method holds the promise of personalized medicine—patient-specific iPSCs sidestep the possibility of immune rejection.
- Adult Stem Cells: While typically less potent in their differentiation range, certain mesenchymal or neural progenitor stem cells may still differentiate into cells resembling RPE or secrete growth factors that support RPE and photoreceptors.
Determining the most practical and safe source of RPE cells for Stargardt therapy remains under active study. Each approach has its benefits and drawbacks, with immunogenicity, ethical considerations, and scalability all playing roles in the choice.
Potential Advantages Over Conventional Methods
Conventional management for Stargardt disease often includes antioxidant supplementation, protective eyewear, and visual rehabilitation to support remaining eyesight. Though these methods can offer symptomatic relief and slow progression marginally, they do not fundamentally replace or rejuvenate diseased tissue. Stem cell therapy, on the other hand, is designed to restore function at a cellular level:
- Tissue Regeneration: By implanting new RPE cells, therapy aims to rebuild a damaged retinal layer, addressing the root cause of many degenerative changes.
- Biochemical Repair: Healthy RPE cells help clear waste products, regulate nutrition, and maintain a stable environment essential for photoreceptor survival.
- Neuroprotection: Newly introduced cells may release growth factors and other signals that help preserve existing photoreceptors and slow disease progression.
Although initial evidence from research and pilot trials points toward beneficial outcomes, large-scale confirmation is still ongoing. Nevertheless, the rationale behind replacing RPE cells is compelling enough that many top-tier eye research centers and pharmaceutical companies are pursuing it.
Realistic Expectations
It’s crucial to maintain realistic expectations. Stem cell-based therapy is not yet a definitive cure. For patients whose Stargardt disease has progressed significantly—where photoreceptors are already extensively damaged—transplanting fresh RPE cells can only do so much. Nevertheless, in earlier stages or in those with some preserved retinal layers, the new cells might protect and even partially rejuvenate central vision.
Furthermore, patients must be aware that clinical trials remain the main avenue for accessing such treatments in many parts of the world. Strict regulatory pathways ensure that transplanted cells meet rigorous safety standards. Potential complications include immune rejection, infection, or the theoretical risk of unwanted cell growth. By rigorously screening patients and refining protocols, researchers aim to optimize both safety and success rates, opening a future where RPE-based cell therapy becomes a cornerstone in Stargardt disease treatment.
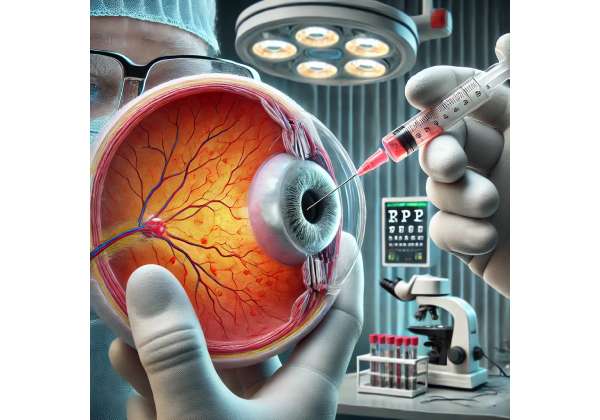
How RPE Cell Transplants Are Performed and Managed
Successfully implanting stem cell-derived RPE cells into a patient with Stargardt disease requires meticulous coordination of surgical technique, cell preparation, and follow-up care. The goal is to deliver new cells precisely where they can best function—in the subretinal space, beneath the retina—while minimizing trauma and maximizing cellular integration. From laboratory processes that yield RPE cells to the operating room protocol, each step plays a pivotal role in achieving favorable outcomes.
Laboratory Cultivation and Quality Checks
Long before a patient enters the operating suite, a team of cell biologists and technicians work on cultivating healthy RPE cells from a chosen stem cell source. In the case of iPSC lines, researchers start with an adult somatic sample (e.g., a simple skin biopsy), introduce reprogramming factors, and guide the resulting pluripotent cells to differentiate into RPE. Similarly, in embryonic stem cell lines, scientists control the differentiation pathways to produce pure RPE populations. Key processes include:
- Differentiation Protocols: Specialized growth media containing factors like nicotinamide, IGF-1, or retinoic acid can steer stem cells toward an RPE fate.
- Purification and Expansion: Once a population of RPE-like cells emerges, they are expanded until the desired cell count is reached, ensuring that enough viable cells are available for transplantation.
- Quality Assurance: Researchers analyze cell markers, morphology, and functionality. For instance, lab tests may measure the ability of RPE cells to phagocytose photoreceptor outer segments, confirm expression of critical RPE genes, and ensure no contamination or unintended cell types are present.
Following growth and quality checks, the cells are often suspended in a carefully crafted solution or seeded onto a scaffold (like a thin polymer membrane) to maintain their alignment and shape. This step can be vital, as RPE cells naturally form a monolayer in vivo, and certain scaffolds may facilitate more natural integration.
Surgical Delivery into the Eye
The next stage occurs in the ophthalmic operating room. Surgeons with expertise in retinal procedures typically perform a vitrectomy—a process in which the vitreous gel is partially or fully removed from the eye. This clearance allows them to access the subretinal space where RPE cells reside.
With the retina exposed, a microinjection or specialized cannula delivers the RPE cell suspension or scaffold beneath the retina. Ensuring that the correct area of the retina is targeted, especially regions of maximal damage or areas likely to benefit from transplanted cells, is essential. High-resolution imaging, such as optical coherence tomography (OCT), may guide the surgeon. This step is delicate: applying too much pressure or volume can create retinal detachment, while insufficient precision may result in poor cell placement and suboptimal integration.
Postoperative Care and Rehabilitation
Once RPE cells are in place, the recovery phase begins, often involving close clinical surveillance to detect any signs of retinal detachment, inflammation, or infection. Physicians might prescribe topical or systemic immunosuppressants to prevent cell rejection, especially if embryonic or unmatched iPSC-derived cells were used. Patients also receive standard post-surgery treatments like antibiotic eye drops to minimize the risk of infection.
Visual rehabilitation is another element of the post-surgery protocol. Since implanted RPE cells aim to preserve or slightly restore central vision, patients might benefit from low-vision training, light-sensitivity management, and specialized optical aids. Some clinics systematically evaluate visual acuity, color vision, and contrast sensitivity over weeks to months, tracking whether improvements correlate with integrated transplanted cells.
Monitoring Long-Term Outcomes
Stargardt disease is chronic, and benefits from cell therapy may unfold gradually. Over time, repeated eye examinations can reveal whether transplanted cells remain stable and functional. Tools like OCT track subretinal changes, while microperimetry measures localized visual function. Additionally, fluorescent angiography or fundus autofluorescence may check the health of RPE layers and detect abnormal accumulations of toxic byproducts.
Regular communication between the patient and their healthcare team is essential. If any unexpected side effects—like persistent inflammation or unusual growth patterns—emerge, swift medical intervention is critical. Conversely, clear improvement in quality of life or visual capabilities, even modest gains, can validate the therapy’s impact and guide further refinements in technique for future patients.
By aligning cutting-edge laboratory science with advanced surgical methods and diligent follow-up, RPE transplant procedures have the potential to alter the course of Stargardt disease. Although still evolving, these clinical protocols are becoming increasingly precise, offering a chance at meaningful vision improvement for those who otherwise faced a gradual decline in eyesight.
Current Investigations and Encouraging Developments
Stem cell-based therapies for Stargardt disease, particularly those focusing on RPE cells, are the subject of keen interest among ophthalmic researchers worldwide. Clinicians are testing new cell lines, refining transplantation techniques, and using advanced imaging tools to monitor outcomes more effectively. As a result, a growing body of evidence supports the safety and potential benefits of these approaches, spurring further investment and optimism in the field.
Notable Clinical Trials
Several high-profile clinical trials have helped shape our understanding of RPE cell therapy for inherited retinal diseases like Stargardt. While each study has unique protocols and objectives, collectively they highlight key trends:
- Phase I/II Studies with hESC-derived RPE: Early-stage clinical trials using human embryonic stem cell (hESC)-derived RPE grafts demonstrated that the procedure is generally safe and well-tolerated in patients with Stargardt disease or dry age-related macular degeneration (AMD). Many participants maintained or improved their visual acuity, although the magnitude of improvement varied widely.
- iPSC-based RPE Trials: Some research centers, particularly in Japan, have pioneered induced pluripotent stem cell technology, testing patient-specific iPSC lines. These studies aim to reduce the risk of immune rejection by using cells genetically identical to the patient. Preliminary findings suggest stable integration of the transplanted RPE and minimal inflammatory responses, which is promising for future large-scale implementation.
- Scaffold-based Transplants: Rather than injecting loose cells, certain research groups are employing biodegradable scaffolds or polymeric sheets seeded with RPE. Early results indicate that these constructs might encourage more uniform cell layering, enhancing viability and functional outcomes.
Many of these trials remain ongoing, continually assessing safety parameters like tumor formation risk or severe immune complications. However, their encouraging interim data consistently point toward the viability of RPE-based therapies.
Advancements in Imaging and Biomarkers
Integral to these clinical breakthroughs are significant enhancements in retinal imaging and biomarker analysis. Sophisticated technologies such as adaptive optics scanning laser ophthalmoscopy (AOSLO) can visualize individual photoreceptors, allowing researchers to see, in near real-time, whether transplanted RPE is supporting local photoreceptor survival. Blood tests and ocular fluid analyses sometimes track changes in inflammatory markers or growth factors, potentially offering insight into how effectively new cells are functioning at a molecular level.
Genetic tests and gene expression profiling are also utilized in tandem with RPE transplantation studies. By correlating specific genotypes of Stargardt disease with patient responses, scientists hope to pinpoint which subsets of the population might benefit the most. Personalized medicine approaches, in which therapy is tailored to each patient’s genetic background, could further enhance success rates.
Collaborative Research Efforts
Large consortia and international collaborations significantly boost the pace of progress. Institutions such as the National Eye Institute (NEI) in the United States and parallel European research networks fund multi-center studies, pooling data from diverse patient populations. This collaborative model accelerates the learning curve, allowing for swift identification of best practices while minimizing redundancy in research efforts.
Moreover, partnerships between academia and industry ensure that laboratory discoveries can be translated into scalable, clinically relevant products. Pharmaceutical and biotech companies working on cell therapy production, scaffold design, or immunomodulatory regimens coordinate with public health bodies to navigate regulatory pathways. Although the process can be lengthy, the synergy between research labs and commercial players is fundamental to transforming experimental treatments into mainstream clinical solutions.
Moving Toward Widespread Adoption
As data from ongoing trials accumulate, more patients and clinicians are becoming aware of the potential of RPE replacement. Over time, one can envision a scenario where a patient newly diagnosed with Stargardt disease might be offered comprehensive genetic testing, followed by a personalized RPE transplant protocol tailored to their unique disease stage and genetic profile. Rigorous follow-up would confirm integration of the transplanted cells and monitor vision changes, with the possibility of repeated or “booster” treatments if necessary.
While this scenario remains aspirational for most current patients, the trajectory of research suggests it may not be too far off. Each successful pilot case and clinical trial not only signals confidence in the approach but also fosters further technological refinement. By continuing to define best practices—such as which cell source is optimal, how to reduce procedure complexity, and how to mitigate cost—RPE-based cell therapies could emerge as a pivotal treatment for Stargardt disease in the near future.
Evaluating Clinical Outcomes and Possible Risks
The ultimate measure of any intervention for Stargardt disease—or indeed any retinal condition—is how effectively it preserves or improves vision while ensuring patient safety. Stem cell therapies targeting RPE cells are no exception. Although the global perspective on these treatments is largely optimistic, careful scrutiny of clinical data and real-world patient experiences is necessary to understand both the rewards and the potential downsides.
Visual Improvements and Stabilization
Preliminary results from various studies often show modest but clinically meaningful visual gains. Specifically:
- Visual Acuity: Some participants report improvements of a few lines on the Snellen chart. While these changes can make a difference in day-to-day tasks, they may not restore perfect central vision, especially in advanced disease.
- Contrast Sensitivity: Patients sometimes note better detection of subtler contrasts, important for reading in low light or distinguishing objects against similarly hued backgrounds.
- Reduced Progression Rate: In many cases, the therapy appears to slow or halt the progression of retinal atrophy. This benefit can be particularly significant for younger patients who have more to lose if the disease progresses unchecked.
Not every patient experiences improvement, and some see only a plateau in their visual deterioration—a result that can still be viewed as positive, given Stargardt disease’s typically relentless progression.
Safety Profile and Immunological Considerations
From a safety standpoint, most stem cell transplant trials follow participants for months to years to catch delayed complications:
- Immune Rejection: Even though the retina is considered somewhat immune-privileged, foreign cells might still trigger a reaction. Patients receiving hESC-derived RPE may require immunosuppressive medications for a time. iPSC-based approaches that use the patient’s own cells are thought to reduce this risk significantly.
- Tumorigenicity: A theoretical concern with pluripotent stem cells is the possibility of teratoma formation or unchecked cell growth. Thorough differentiation protocols and cell purification drastically reduce this risk, but it remains an important parameter under continuous surveillance in clinical trials.
- Surgical Complications: Any intraocular surgery can introduce risks like infection, hemorrhage, or retinal detachment. Skilled surgeons and careful postoperative management help keep these complications relatively low in incidence.
Importance of Timing and Disease Stage
Another crucial factor influencing outcomes is the stage at which the intervention takes place. For patients with Stargardt disease in its early or intermediate phases, RPE cell therapy may yield better results. Once photoreceptor cells have degenerated extensively, providing healthy RPE might not suffice to restore meaningful function. This highlights the importance of early detection and a proactive approach, a challenge given that Stargardt disease can sometimes progress undiagnosed until noticeable vision loss sets in.
Quality of Life Considerations
Beyond objective clinical metrics, many patients gauge success by improvements in daily function. Tasks like reading, navigating indoors, recognizing faces, and driving in early-stage cases can define independence and well-being. Even modest gains in central vision or contrast sensitivity can significantly enhance day-to-day living. Psychologically, receiving an innovative therapy—especially if it halts further decline—can offer hope and reduce the emotional strain tied to progressive, incurable diseases.
Ongoing Monitoring and Patient Responsibility
Those who undergo RPE transplantation typically commit to frequent follow-up visits. Regular eye exams, imaging studies, and possible blood tests for immunological markers help clinicians identify and address any emerging issues early. This degree of monitoring, while time-intensive, is crucial to maximizing the therapy’s benefits and detecting adverse events.
Ultimately, RPE-focused stem cell therapy remains in the investigative phase, but the consistent observation across multiple clinical settings is that many patients experience a favorable balance of efficacy and safety. As methods and technologies advance, so should the reliability and accessibility of these therapies, edging closer to becoming a standard option for Stargardt disease patients.
Cost Factors and Financial Considerations of RPE-Based Treatments
Stem cell therapy involving RPE cells is highly specialized and can be financially demanding. In many countries, full-scale clinical protocols may cost several thousand to tens of thousands of dollars or more, reflecting the complexity of cell production, surgical expenses, and postoperative monitoring. Some research clinics or non-profit foundations offer subsidized programs to offset these costs for eligible participants. However, coverage by insurance plans remains varied. While certain insurers may partially reimburse experimental treatments under compassionate use, others classify them as investigational. Patients exploring these therapies should inquire about potential out-of-pocket fees, travel expenses to specialized centers, and the possibility of participating in a formal clinical trial that might reduce or eliminate certain costs.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or treatment.
We invite you to share this article with friends, family, or online groups that might benefit from learning about stem cell therapy for Stargardt disease. Please use our Facebook and X (formerly Twitter) share buttons—or any other platform you prefer—to help spread hope and awareness of this promising treatment avenue!