Glaucoma is one of the world’s leading causes of irreversible blindness, affecting millions of people across different age groups and ethnicities. Characterized by progressive damage to the optic nerve, glaucoma often arises from elevated intraocular pressure (IOP) that compromises blood flow and nerve fiber health. Although the condition initially presents with few to no symptoms, untreated high IOP eventually leads to peripheral vision loss, culminating in tunnel vision or complete blindness.
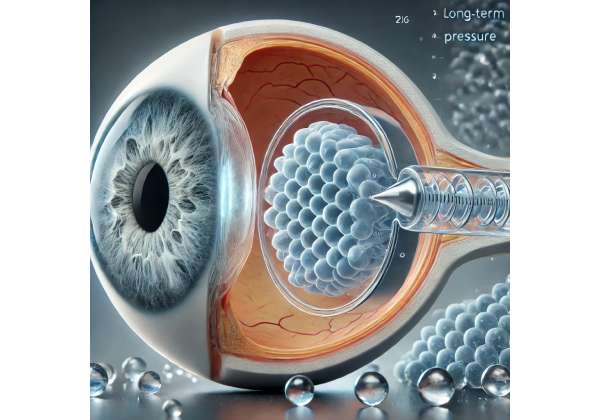
Many patients rely on medication, laser therapies, or conventional surgical implants to regulate IOP. However, each intervention carries its own limitations, ranging from daily adherence challenges with eye drops to more invasive surgical risks. A new frontier in minimally invasive glaucoma surgery (MIGS) is now emerging: hydrogel-based implants designed to maintain long-term pressure control with fewer complications. These advanced devices promise a gentler approach to outflow enhancement, harnessing the unique properties of hydrogels to sustain consistent IOP reduction while preserving ocular structures. Below, we explore how these implants work, their advantages over existing treatments, and how they may reshape our standards for glaucoma care.
A Closer Look at Hydrogel Solutions for Glaucoma
Glaucoma therapy primarily focuses on lowering intraocular pressure by improving aqueous humor outflow or decreasing its production. Traditional strategies vary from topical medications—prostaglandin analogs, beta-blockers, carbonic anhydrase inhibitors—to surgeries like trabeculectomy or drainage device implantation. Yet each approach has drawbacks: medications can be hard to maintain daily, and surgeries can lead to complications or insufficient pressure control over time.
Hydrogel implants aim to bridge the gap between pharmacological convenience and surgical efficacy. By leveraging the swelling and water-retaining capabilities of hydrophilic polymers, these implants establish or augment a drainage pathway for aqueous fluid. The hydrogel’s biocompatibility and malleability also reduce the risk of tissue damage or scarring.
The Science Behind Hydrogels
Hydrogels are three-dimensional networks of hydrophilic polymers that can absorb and retain large amounts of water. The high water content renders them soft and pliable, mimicking the properties of living tissues—a significant advantage for ophthalmic applications. Key attributes of hydrogels used in glaucoma implants include:
- High Biocompatibility: Ensuring minimal inflammatory or immune reactions.
- Stability and Elasticity: Maintaining shape under physiological conditions while accommodating subtle changes in ocular tissues.
- Adjustable Porosity: Engineers can tune the hydrogel’s pore size to modulate fluid flow rates or drug release if needed.
- Inertness: Hydrogel surfaces generally resist protein adsorption and bacterial colonization, minimizing complications like infection or device occlusion.
When placed at the correct outflow site—usually near the trabecular meshwork or the suprachoroidal space—hydrogel implants facilitate or enlarge an outflow channel, letting aqueous humor drain more easily. The device passively adjusts to microenvironmental changes without the permanent structural modifications seen with older stents or full-blown filtration surgeries.
Redefining Minimally Invasive Approaches
Minimally invasive glaucoma surgery (MIGS) has gained popularity for reducing complications compared to traditional filtering procedures. MIGS typically aims for modest IOP reduction in mild-to-moderate glaucoma, with the potential for faster recovery times. Hydrogel-based devices extend MIGS possibilities:
- Implantation via Microincision: Surgeons can deliver hydrogel-based devices through small incisions that reduce healing time, infection risk, and patient discomfort.
- Lower Tissue Trauma: The device’s soft composition is gentler on sensitive eye structures, lessening the threat of scarring or unpredictable wound healing.
- Potential for Combination: Surgeons can perform the implant procedure alongside cataract extraction or in synergy with medication regimens.
The synergy of minimal invasiveness, robust IOP control, and improved tissue compatibility sets hydrogel implants apart from older-generation surgical tubes or shunts. By providing a measured outflow that matches physiological fluctuations, these implants could help maintain stable pressures without drastically overshooting or undershooting the target IOP.
Understanding the Breakthrough Technology Behind Hydrogel Implants
Hydrogel-based implants draw on advanced material science to ensure they function effectively inside the eye’s delicate environment for years. Each stage of design and manufacturing carefully addresses the challenges unique to ocular tissues, such as preventing fibrosis, ensuring consistent drainage, and maintaining implant stability over long durations.
Polymer Composition and Functionality
The choice of polymer is crucial. Polymers like poly(2-hydroxyethyl methacrylate) (pHEMA), polyethylene glycol (PEG) derivatives, or silicone-modified hydrogels are commonly investigated. The device’s hydration level can surpass 80% of its weight in water, ensuring softness and compliance. Some designs also integrate cross-linkers to strengthen the gel matrix without rendering it too rigid.
A typical hydrogel implant might expand slightly after insertion, gently pressing against the sclera or the trabecular meshwork. However, advanced formulations maintain controlled expansion, so they do not obstruct normal ocular anatomy or cause overfiltration. Microchannels within the hydrogel govern fluid flow, letting aqueous humor pass at a regulated rate. Over time, the device adapts to subtle changes in the ocular environment, retaining its shape without degrading or losing mechanical integrity.
Device Architecture and Placement
Various shapes and architectures have emerged, with the final design depending on the targeted outflow route:
- Trabecular Meshwork Implants: Placed near Schlemm’s canal, these implants bypass a portion of the meshwork to reduce outflow resistance. The hydrogel portion ensures gentle stent patency and less friction with surrounding tissues.
- Suprachoroidal Shunts: Inserted between the sclera and choroid, these implants harness the negative pressure in the suprachoroidal space to draw fluid out from the anterior chamber. The hydrogel portion helps maintain an open suprachoroidal corridor.
- Subconjunctival Devices: Some implants drain fluid into the subconjunctival space, akin to a bleb, but rely on hydrogel-based control to minimize bleb-related complications and keep more natural physiologic drainage.
Regardless of design, the aim is to provide stable, moderate IOP reduction, reduce or eliminate the need for drops, and limit the risk of scarring or device failure.
Customized Flow Control Mechanisms
One of the biggest engineering challenges is controlling outflow so that the eye doesn’t become hypotonic (extremely low pressure). Hydrogel-based devices can be tailored with micro-scale channels or slit valves to regulate flow, ensuring a more constant IOP near the desired target. If IOP surges, the device might slightly swell, temporarily increasing flow capacity until pressure normalizes.
Some prototypes even explore drug-eluting hydrogels that release anti-fibrotic or anti-inflammatory agents, mitigating scar tissue formation at the device-tissue interface. This approach tries to avoid the typical scenario where scarring eventually blocks or encapsulates older implants. By combining structural support with localized drug delivery, next-generation hydrogels might address two major hurdles: mechanical patency and fibrotic encapsulation.
Biocompatibility and Anti-Inflammatory Properties
Biocompatibility stands front and center for a foreign device in the sensitive ocular environment. The hydrophilic surfaces of the implants generally resist bacterial adherence and reduce friction against delicate tissues, lowering the incidence of postoperative infection or inflammation. Because the device can be placed with minimal incisional trauma, the host response is often mild, with fewer inflammatory cells migrating to the area.
Moreover, the inert polymer chemistry typically translates to minimal immunogenic potential. Some developers incorporate specialized coatings or molecules that further reduce inflammatory cell activation. This focus on a biologically harmonious design helps ensure that the implant remains functional over time, without engendering chronic irritation or the body’s rejection response.
From the polymer’s molecular backbone to the intricately carved fluid channels, every dimension of these hydrogel-based implants revolves around the central mission: offering controlled, stable, and comfortable IOP reduction for patients who might otherwise face progressive vision loss or the inconveniences and side effects of more invasive surgeries.
How Hydrogel Implants Are Placed: Key Steps for Surgeons and Patients
Although hydrogel implants are often classified under the MIGS umbrella, the procedure demands careful planning, specialized training, and well-defined postoperative management. Nonetheless, many patients find that the less invasive nature of hydrogel implantation provides an appealing alternative to older surgical solutions.
Preoperative Assessment and Candidacy
As with any glaucoma procedure, thorough preoperative evaluation is essential:
- Disease Severity and Type: Patients with open-angle glaucoma typically benefit the most. Narrow angles or advanced damage may require alternative or additional interventions.
- Medication History: Surgeons assess how well the patient’s IOP has been controlled with drops or prior laser therapy. If there’s partial or insufficient response, hydrogel implants may fill the gap.
- Anatomical Suitability: Gonioscopy helps confirm the angle structures. Advanced imaging (such as OCT of the anterior segment) may reveal suprachoroidal space details if that’s the intended route.
- General Eye Health: Assessing comorbid conditions—like cataracts or corneal opacities—ensures no competing ocular priority overshadows MIGS. Some surgeons prefer to combine the implant procedure with cataract extraction if feasible.
Deciding whether to implant the device in conjunction with other MIGS or lens-based procedures rests on the patient’s status and the surgeon’s approach. While synergy can save time and sedation, each additional procedure also carries incremental risk.
Surgical Procedure Breakdown
Although each hydrogel device has unique insertion tools or incisions, the general steps might look like this:
- Anesthesia and Setup: Local or topical anesthesia is administered. The eye is draped and prepared in a sterile fashion.
- Microincision Creation: Typically 1-2 mm in length, placed at or near the corneal limbus for angle-based implants, or a slightly more posterior location for suprachoroidal approaches.
- Implant Delivery: The surgeon uses a specialized injector loaded with the hydrogel device. Through gonioscopic guidance (angle implants) or careful dissection (suprachoroidal devices), they position the implant in its final location.
- Position Verification: Real-time imaging or direct visualization ensures correct orientation and anchorage. The surgeon confirms that fluid can pass around or through the hydrogel and that the device does not obstruct other ocular structures.
- Incision Closure (If Needed): Many MIGS incisions are self-sealing. However, if there’s any concern about leaks, a fine suture can be placed. An antibiotic-steroid drop is administered to minimize infection or early inflammation.
Most patients return home the same day, with instructions on postoperative care, which typically includes antibiotic-steroid eye drops for a few weeks. In some cases, surgeons taper the patient’s existing glaucoma medications quickly if the hydrogel device demonstrates adequate pressure reduction.
Postoperative Follow-Up and Adjustments
After surgery, IOP checks and slit-lamp evaluations are frequent in the initial weeks. As the hydrogel integrates, the surgeon monitors:
- Immediate IOP Response: Some implants reduce pressure fairly quickly, while others may take days to reach equilibrium.
- Inflammatory Signs: While mild anterior chamber reaction is common, persistent inflammation might indicate device misplacement or an immune response.
- Position Stability: Even a small migration of the implant can alter outflow. If the device shifts, a minor revision or repositioning under local anesthesia may be required.
- Long-Term Stability: Over months, the surgeon assesses whether the implant continues to maintain target IOP. The patient’s need for adjunctive medications typically declines, but not always entirely.
Most hydrogel implant recipients experience minimal downtime. Visual recovery is usually swift unless combined with cataract surgery or if a rare complication arises. Activities can generally resume within a week, though vigorous exercise is temporarily restricted.
Managing Potential Complications
While safer than extensive filtration surgeries, complications can still occur:
- Hypotony (Excessive Pressure Drop): If outflow is too robust or if the suprachoroidal route fosters uncontrolled drainage, IOP can plummet dangerously. The surgeon might need to place a suture or in-office procedure to reduce outflow.
- Device Dislocation or Occlusion: The implant can shift or develop blockages from blood, inflammatory debris, or fibrin. Revisions or flushing might help.
- Transient PAS (Peripheral Anterior Synechiae): In angle-based approaches, the device might irritate the iris root, causing synechial attachments.
- Inflammation or Infection: As with any ocular surgery, endophthalmitis risk is small but serious. Prophylactic antibiotics and sterile technique mitigate this risk.
In general, the soft, flexible design of hydrogel-based implants lowers the likelihood of mechanical friction or corneal endothelial cell loss. By following close postoperative care and customizing medication taper schedules, surgeons can maximize the chance of stable, long-term success.
Research Behind Hydrogel Devices: Key Insights and Trials
Though a relatively new entrant, hydrogel-based implants have undergone rigorous investigation to validate their effectiveness and safety for long-term glaucoma control. Ongoing clinical trials, observational studies, and laboratory testing collectively shape our understanding of these promising devices.
Early Feasibility and Pilot Studies
Initial case series and feasibility trials typically enrolled small cohorts of 10-50 patients, focusing on:
- Device Tolerability: Patients were monitored for adverse events like persistent inflammation or device extrusion. In general, these pilot projects found high tolerability, with minor inflammatory responses easily controlled by standard steroid drops.
- Short-Term IOP Reduction: Within the first 3-6 months, the majority of patients saw meaningful IOP drops, often reducing or eliminating the need for one or more eye drop medications.
- Stable Anatomic Position: Imaging (like anterior segment OCT) indicated the implants remained well-seated, with no major migrations or blockages.
Although limited by smaller sample sizes, these early results were encouraging enough to propel larger, more robust trials.
Larger Randomized Trials
Some manufacturers or academic consortia have progressed to multicenter, randomized controlled studies comparing hydrogel implants to established MIGS devices or standard medical therapy. Key findings from these advanced trials often highlight:
- Equivalent or Superior Pressure Control: Hydrogel devices maintain IOP reduction on par with mainstream MIGS solutions, such as iStent or Xen Gel Stent, with the potential benefit of a gentler insertion technique.
- Reduced Medication Burden: A significant fraction of hydrogel-implanted patients either discontinued topical medications entirely or only needed a mild regimen to maintain target IOP, translating to cost savings and improved adherence.
- Long-Term Durability: Published data for 2-3 year follow-ups suggest robust stability, though extended 5+ year data is still pending. Early signs indicate these implants may remain functional without major reoperation.
Additionally, the risk profiles frequently compare favorably to older filtering surgeries like trabeculectomy or tube shunts, which can be prone to bleb leaks, hypotony, or bleb infections. The minimal incisional approach likely lowers the incidence of such complications.
Bench and Animal Model Testing
Before reaching human trials, hydrogel materials undergo extensive bench testing, measuring mechanical strength, swelling ratios, fluid conduction, and resilience under cyclical ocular pressure. Animal models—often rabbits, pigs, or primates—validate the device’s biological performance in living tissue. Among key areas of focus:
- Fibrotic Response: Scientists track whether fibroblasts encapsulate or degrade the hydrogel over time. Many designs incorporate anti-fibrotic strategies to minimize scarring.
- Infection Susceptibility: The device’s surface is evaluated for bacterial adhesion, with modifications introduced if microbial growth is discovered.
- Long-Term Degradation or Toxicity: Some hydrogels degrade gradually, so ensuring no harmful byproducts or micro-fragments remain crucial. Non-degradable variants must remain inert.
These preclinical phases refine final device configurations before translation to clinical settings. The synergy of in vitro, animal, and early human data lays the foundation for robust, well-controlled human trials that shape regulatory approvals and best-practice guidelines.
Ongoing Studies and Future Directions
As hydrogel implants gain momentum, additional research lines continue to expand:
- Refined Flow Mechanisms: Some developers investigate “smart hydrogels” that dynamically alter porosity based on environmental factors (e.g., pH or temperature). Theoretically, this might let the device modulate flow in real-time.
- Integration with IoT or Sensor Technology: A potential futuristic angle is combining the implant with micro-sensors that continuously measure IOP, relaying data to a smartphone or clinic. This synergy between sensor data and flow control could personalize therapy even further.
- Patient Selection Metrics: As data accumulates, clinicians will better determine which glaucoma subtypes or stage severities respond best. For instance, angle-closure variants might not benefit unless the angle is re-opened surgically.
- Combined Approaches: Trials also explore using these implants alongside phacoemulsification for cataract, investigating synergy in a single operative session or comparing them with advanced MIGS devices.
Overall, the research trajectory is enthusiastic. Analysts anticipate that with a few more years of data, hydrogel devices could become as common as existing MIGS implants, offering a new dimension in personalized, effective, and stable IOP management.
Real-World Impact, Safety Record, and Key Advantages
Clinical success stories underscore how hydrogel-based implants can transform daily life for glaucoma patients who once relied on multiple eye drops or faced repeated surgeries. By consistently lowering IOP to a safer range, these devices aim to halt or slow the progressive damage to the optic nerve, preserving visual fields and quality of life.
A More Comfortable Alternative to Conventional Surgery
Many patients find the concept of a gentler, microincisional device appealing. Traditional filtering surgeries (e.g., trabeculectomy) or large drainage implants demand significant healing times, bleb management, and frequent postoperative adjustments. In contrast, hydrogel implants:
- Reduce the Postoperative Burden: The device’s design lowers the risk of leaks, hypotony, or bleb-related complications.
- Offer Quick Recovery: Most people resume normal activities within a few days, and frequent follow-up visits primarily serve to confirm stable IOP rather than intervene in complications.
- Diminish the Fear Factor: Patients who shy away from major eye surgeries might accept MIGS with a hydrogel approach.
Safety Profile and Potential Hurdles
Though generally safe, each device or approach carries inherent risks:
- Transient Hypotony: If the initial outflow is more vigorous than planned, IOP can drop too low. Early detection typically resolves this via minor interventions.
- Late Occlusion: Rarely, inflammatory cells or micro-hemorrhages can clog the device channels. Some cases may require in-office flushing or reoperation.
- Material Degradation (If Biodegradable): For certain designs intended to degrade over time, incomplete or uneven breakdown might affect flow consistency.
- Learning Curve: Surgeons new to MIGS or specifically to the hydrogel implant technique may require training to master the correct placement angle, depth, or injection speed.
When performed by experienced specialists, the incidence of severe complication is low, and the implants are well-received. Often, standard MIGS precautions—such as managing minor hemorrhages or inflammatory responses—apply similarly to hydrogel implants.
Confirmed Gains in Quality of Life
Reported patient-reported outcomes from preliminary studies and anecdotal evidence highlight benefits like:
- Reduced Medication Load: Some individuals can stop using daily eye drops entirely, while others see a 50-75% drop in usage. Less medication means fewer side effects, costs, and compliance burdens.
- Improved Confidence and Lifestyle: Stably controlled IOP can reduce anxiety over sudden vision deterioration. Activities like reading, driving, or traveling become more consistent.
- Less Frequent Office Visits: Once stabilized, the implant requires minimal ongoing adjustment, freeing patients from frequent re-checks or procedures.
Over time, these incremental advantages translate into substantial emotional and financial relief for both patients and healthcare systems. By lowering the risk of advanced glaucoma damage and the need for more invasive interventions down the road, hydrogel devices demonstrate a compelling cost-benefit ratio, especially for those diagnosed at moderate stages.
Pricing and Potential Coverage for Hydrogel Implants
As a new technology, hydrogel implant procedures can vary in cost depending on the device used, the clinical facility, and geographic location. In many regions, total fees (including device cost, surgeon’s fee, and operating room expenses) might range from around \$3,000 to \$6,000 per eye. Because not all insurers have recognized the therapy’s long-term benefits, coverage remains inconsistent—some may classify it under MIGS procedures for moderate open-angle glaucoma, while others may require prior authorization or a demonstration of medical necessity.
Patients often explore options such as:
- Private Insurance Plans: Some might cover all or part of the procedure under specialized MIGS codes or if the patient has shown inadequate response to more conventional treatments.
- Health Savings Accounts (HSAs): Funds from HSAs can help offset out-of-pocket costs.
- Financing Programs or Payment Plans: Certain clinics offer monthly payment structures to accommodate those lacking full insurance support.
- Research Grants or Trial Participation: If a device is still under clinical investigation, patients might qualify for subsidized or free treatment in exchange for being part of a study.
Ultimately, prospective recipients should request a clear cost breakdown from their eye surgeon or healthcare facility. While up-front costs might be higher than continuing topical medications, the promise of lasting IOP management and fewer medication dependencies can prove financially and medically advantageous over the long term.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or treatment.
We warmly invite you to share this article with friends, family, or online communities who might benefit. Use our Facebook and X (formerly Twitter) share buttons—or any other platforms you prefer—to help spread the word about hydrogel-based implants and their potential to transform glaucoma management!






