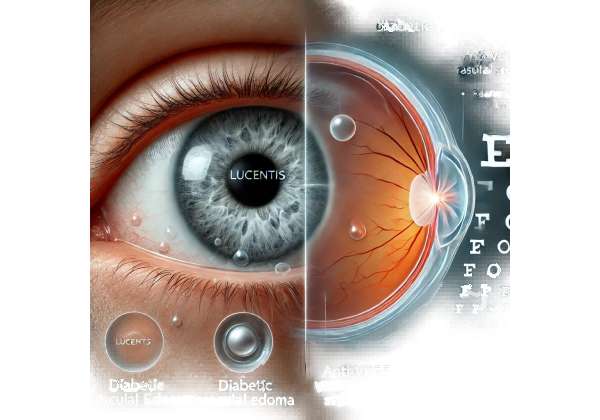
If you’ve been wondering how advanced therapies can help control diabetic macular edema (DME) and preserve your precious eyesight, you’re not alone. The journey to clearer vision doesn’t have to be complicated—even for those dealing with diabetes-related eye complications that can cause blurry vision and daily frustration. One of the most promising and widely discussed treatments is Lucentis, a powerful anti-VEGF medication that’s made a name for itself in the field of retinal care.
Diabetic macular edema can sneak up on you with subtle changes—like increased difficulty reading or driving—before escalating into more significant visual impairments. Knowing what treatments are available, and how they work, is a crucial first step toward preserving and improving your vision. Let’s dive into the world of Lucentis, exploring why so many ophthalmologists and patients see it as a game-changer in DME management.
Understanding the Science Behind Anti-VEGF Solutions
Lucentis, whose generic name is ranibizumab, belongs to a class of drugs known as anti-VEGF (vascular endothelial growth factor) inhibitors. VEGF is a protein naturally produced in the body that stimulates the formation of new blood vessels. Under normal circumstances, VEGF helps maintain healthy tissue growth and repair. However, in some conditions like diabetic macular edema, overproduction of VEGF triggers the growth of leaky blood vessels in the retina. This can result in fluid accumulation at the macula—the region of the retina responsible for sharp, central vision—leading to swelling (edema) and subsequent vision impairment.
How Diabetic Macular Edema Develops
When you have diabetes, chronic high blood sugar levels can damage the delicate network of blood vessels supplying the retina. These vessels can weaken, become more permeable, and leak fluid. Over time, these leaks may cause the macula to swell. Once that swelling sets in, even routine tasks such as reading, working at a computer, or recognizing faces can become more difficult. This process may happen slowly, but without effective intervention, vision can progressively worsen.
Mechanism of Action: Stopping Abnormal Vessel Growth
Lucentis is engineered to bind specifically to VEGF molecules, preventing them from attaching to their receptor sites on the surface of retinal cells. By blocking this interaction, Lucentis significantly reduces the stimulus for abnormal blood vessel formation and leakage in the retina. This “lock-and-key” mechanism is crucial because it directly targets the root of the problem: excessive VEGF activity in the eye. When VEGF is inhibited, the cascade leading to abnormal vessel growth slows or stops, and existing leaky vessels often begin to stabilize.
The Importance of Targeted Therapy
Before the era of anti-VEGF drugs, treatments for DME often revolved around laser photocoagulation. While laser treatments can be effective for some patients, they work by sealing off leaky vessels and preventing further vision loss rather than actively improving visual acuity. Lucentis, on the other hand, has been shown to not only halt progression but also, in many cases, improve vision.
This type of targeted therapy underscores a broader shift in modern medicine: moving away from blanket approaches toward more specific, precisely engineered solutions. By honing in on VEGF, Lucentis tackles a central mechanism driving retinal swelling, giving patients and clinicians a powerful tool in the fight against DME.
Why Early Intervention Matters
Promptly detecting and addressing diabetic macular edema is essential because the retina, particularly the macula, is incredibly sensitive. The longer swelling persists, the greater the risk of permanent damage to the photoreceptor cells responsible for converting light into signals your brain interprets as vision. Once these cells are damaged, reversing that damage becomes increasingly difficult.
Early intervention with Lucentis often yields better outcomes in terms of visual acuity gains. By administering the medication before extensive damage occurs, patients may experience more significant improvements and a reduced need for additional interventions later.
The Role of Personalized Care
Not every patient with DME will respond identically to the same therapy. Factors like duration of diabetes, blood sugar control, and the presence of other diabetic complications can influence treatment success. That’s why personalized care—adjusting injection frequency, combining treatments, or incorporating lifestyle changes—plays a key role in optimizing results. Ophthalmologists often tailor Lucentis regimens based on each patient’s unique medical history and ongoing response to the therapy.
Looking Beyond Vision
While the eye is the central focus, the benefits of effectively treating DME aren’t limited to improved vision. Clearer eyesight can lead to safer driving, enhanced independence, and a better quality of life. It also allows individuals with diabetes to be more proactive about their overall healthcare; for instance, they can read food labels accurately, track blood glucose levels more easily, and stay physically active.
In essence, Lucentis represents a milestone in addressing the vascular complications that stem from diabetes. Its targeted mechanism promises not only the possibility of stabilizing or improving vision but also the potential for reclaiming a more confident, fulfilling lifestyle.
Practical Steps to Optimize Your Lucentis Experience
When it comes to receiving Lucentis injections for diabetic macular edema, there’s more to the process than just the medication itself. From pre-treatment assessments to post-injection care, understanding the practical aspects of Lucentis therapy can significantly improve your experience and overall outcome.
Pre-Treatment Evaluations
Before you and your ophthalmologist decide that Lucentis is your best option, a series of tests and evaluations typically take place. Common diagnostic procedures include:
- Fundus Examination: Your doctor will closely inspect the back of your eye (the retina) using specialized instruments to gauge the extent of any edema or hemorrhage.
- Optical Coherence Tomography (OCT): This imaging test is crucial for quantifying the thickness of your macula and identifying fluid pockets.
- Fluorescein Angiography (FA): A contrast dye is injected into a vein in your arm, and a camera takes pictures of the retina to highlight areas of leakage or abnormal blood vessels.
These evaluations help determine whether Lucentis is suitable for you and establish a baseline against which future improvements can be measured.
Setting Up a Treatment Schedule
Lucentis is generally administered via intravitreal injection (an injection into the vitreous gel in the back of the eye). While initial treatment protocols often involve monthly injections, schedules can vary. Some patients respond so well that the injection frequency can be reduced after the initial loading phase—sometimes referred to as a treat-and-extend regimen. Others may require more frequent or ongoing monthly treatments, especially if their condition is severe or if macular swelling returns.
Injection Day: What to Expect
Many patients feel anxious about the idea of an injection into their eye. However, the procedure is typically quick and done under local anesthesia to minimize discomfort. Here’s a basic rundown:
- Numbing the Eye: Your ophthalmologist will administer drops or use a small injection of anesthetic to make the procedure pain-free.
- Cleaning and Preparation: Antiseptic solutions are applied to reduce the risk of infection.
- Intravitreal Injection: A fine needle is used to deliver Lucentis directly into the vitreous cavity. The process itself is brief—often just a few seconds.
- Post-Injection Check: You’ll typically remain in the clinic for a short observation period to ensure there’s no immediate complication such as increased eye pressure or infection.
Aftercare and Follow-Up
Mild irritation, redness, or blurriness for a day or two following an injection is not unusual. Your doctor may recommend using antibiotic eye drops as a preventative measure against infection. Resting your eyes, avoiding strenuous activity, and steering clear of potential irritants—such as dust or smoke—can also help speed recovery.
Regular follow-up appointments allow your healthcare team to monitor your progress and adjust your treatment plan as needed. These visits may include repeat OCT scans to check macular thickness and confirm whether fluid accumulation has decreased.
Co-Managing Diabetes
Optimal management of diabetic macular edema goes hand in hand with good diabetes care. Maintaining stable blood glucose levels, controlling blood pressure, and adhering to a balanced diet are all critical in preventing further damage to the retinal vessels. In some cases, your primary care physician, endocrinologist, or diabetes educator can collaborate closely with your eye doctor to ensure an integrated approach. This multi-pronged strategy often includes:
- Routine Blood Sugar Checks: Consistency is key for preventing blood vessel damage over time.
- Dietary Counseling: A dietitian can help create meal plans that minimize blood sugar spikes.
- Physical Activity: Moderate exercise improves overall blood vessel health and can enhance insulin sensitivity.
- Medication Reviews: If you’re on oral or injectable diabetes medications, ensuring they’re at the correct dose is essential for long-term eye health.
Communication and Awareness
Never hesitate to reach out to your healthcare team if you notice any change in your vision—such as new floaters, a sudden increase in blurriness, or flashes of light. Early intervention often prevents minor issues from turning into significant complications. Engaging in open dialogue with your ophthalmologist not only builds trust but also helps tailor a regimen that suits your lifestyle and medical needs.
Navigating Emotional and Social Factors
Living with a chronic condition like diabetes can be emotionally taxing. Dealing with eye injections or the threat of vision loss can compound that stress. Seek support from friends, family, or mental health professionals if you find it challenging to cope with your treatment schedule or the day-to-day realities of diabetes. Local support groups and online communities can also be invaluable for tips, encouragement, and shared experiences.
By embracing a comprehensive approach—pre-treatment assessments, informed scheduling, good diabetes management, and emotional support—you’re setting yourself up for the best possible Lucentis experience. Remember, each step along this path, from the first diagnostic test to each subsequent follow-up appointment, is an opportunity to fine-tune your care and preserve your vision.
Evidence from Clinical Trials and Real-World Findings
Solid scientific backing underpins Lucentis’ reputation as a premier therapy for diabetic macular edema. Numerous clinical trials and studies—both randomized controlled trials and observational research—have highlighted the medication’s ability to curb retinal swelling and potentially improve visual acuity. A closer look at some of these studies can help you appreciate the depth of medical consensus surrounding Lucentis.
Landmark Studies that Shaped Current Practices
- RIDE and RISE Trials (Published in Ophthalmology, 2012): These pivotal Phase III trials enrolled hundreds of patients with DME to assess the safety and efficacy of monthly Lucentis injections. The findings were striking: a significant portion of participants receiving ranibizumab gained at least 15 letters in best-corrected visual acuity (BCVA) compared to those in the sham group. Equally important, fewer Lucentis-treated patients progressed to more severe stages of diabetic retinopathy.
- RESOLVE Study (Published in Diabetes Care, 2010): This trial investigated different doses of Lucentis for DME and found that higher treatment doses tended to yield better improvements in BCVA. The authors also noted a decline in central retinal thickness, an indicator of reduced swelling, demonstrating the medication’s targeted impact on retinal fluid accumulation.
- RESTORE Trial (Published in Ophthalmology, 2011): Researchers evaluated Lucentis in conjunction with laser photocoagulation therapy versus laser alone. The group receiving combined treatment not only had better visual outcomes but also experienced less macular thickening compared to the group treated solely with laser therapy. This study laid the groundwork for combination strategies in clinical practice.
Ongoing Research Efforts
While Lucentis has firmly established itself, the research pipeline continues to evolve. Current investigations explore whether extended dosing intervals maintain visual gains over longer periods. Some studies are also examining the potential benefits of combining Lucentis with newer therapies that target additional pathways implicated in DME. This broad, ongoing research reflects a deeper commitment to refining and personalizing DME treatment strategies.
Real-World Observational Data
Clinical trials provide controlled conditions to ascertain efficacy and safety, but real-world data offer valuable insights into how treatments perform outside research settings. A variety of observational studies and patient registries have highlighted:
- Adherence Factors: Patients who follow their injection schedules more consistently often show better maintenance or improvement in vision.
- Long-Term Stability: Many patients sustain gains in visual acuity over multiple years with appropriately spaced injections.
- Variable Response: Although the majority benefit, a subset of patients may require additional treatments or combination approaches (e.g., adding laser therapy or steroids for better outcomes).
Impact on Daily Life
In addition to quantifiable improvements in visual acuity, patients often report enhanced quality of life. They may find it easier to read, drive, or recognize faces—an effect that can significantly reduce the mental strain associated with vision loss. By curbing the likelihood of severe vision impairment, Lucentis may enable individuals to continue working, maintain independence, and stay socially active longer.
Global Health Perspectives
Organizations like the World Health Organization (WHO) and the American Academy of Ophthalmology (AAO) emphasize the importance of early detection and treatment of diabetic retinopathy and DME. While they generally stop short of recommending specific brand-name drugs, the positive data on anti-VEGF therapies, including Lucentis, shapes global clinical guidelines. In many regions, healthcare systems have begun to prioritize funding and insurance coverage for anti-VEGF therapy in recognition of its cost-effectiveness when weighed against the long-term burden of vision loss.
Interpreting the Data
When reading about clinical trials, it’s essential to recognize that not all patients respond identically. Factors like how long you’ve had diabetes, your baseline retinal health, and your ability to maintain consistent follow-up all influence treatment outcomes. Additionally, clinical trial populations may not mirror every nuance of real-world demographics and comorbidities. Nonetheless, the breadth of evidence supporting Lucentis underscores its role as a cornerstone therapy in the battle against DME.
In summary, an ever-growing body of research—from large-scale trials to real-world observational data—demonstrates that Lucentis can not only halt the progression of diabetic macular edema but also, in many cases, significantly improve vision. This dual promise of halting disease progression and restoring lost function resonates with both patients and the ophthalmic community at large, making Lucentis a leading candidate for DME management.
Evaluating Outcomes: Efficacy and Patient Safety
When considering any medical treatment, especially one as delicate as an intravitreal injection, it’s natural to weigh the expected benefits against potential risks. In the case of Lucentis, decades of combined clinical practice and study data suggest that most patients tolerate the medication well and experience meaningful improvements in visual acuity.
Still, as with any injectable therapy, there are potential side effects. Common, generally mild issues include eye redness, mild discomfort, and temporarily blurred vision. Rare but serious complications, such as retinal detachment or intraocular infection (endophthalmitis), require prompt medical attention. Ophthalmologists typically follow strict protocols—using antiseptic measures and closely monitoring the eye after injections—to minimize these risks.
Regarding overall effectiveness, numerous clinical trials and observational registries have documented gains in BCVA. Some patients notice improvements within weeks, while others may require multiple injections over several months to achieve meaningful visual changes. Adhering to recommended follow-up schedules, maintaining proper diabetes control, and communicating any concerns early on further enhance the safety and efficacy profile of Lucentis.
Modern Costs: A Glimpse into Lucentis Pricing
The price of Lucentis can fluctuate depending on several factors, including geographic region, insurance coverage, and healthcare facility policies. In the United States, a single injection can sometimes range in the high hundreds to a couple of thousand dollars, particularly without insurance. Patients often explore financial assistance programs, discounts, or copay support through the drug manufacturer or various nonprofit organizations to alleviate the burden.
Disclaimer:
This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for personalized guidance regarding any medical condition or treatment plan.
We hope this detailed exploration of Lucentis offers clarity and insight into its potential to transform the management of diabetic macular edema. If you found this article helpful, feel free to share it on social media—your support can help others learn about effective solutions for preserving eye health.