Living with elevated eye pressure can be stressful—literally and figuratively. You might constantly wonder if those glaucoma drops are doing enough, or if you’ll remember to put them in on time every day. For many years, medicated eye drops have been the standard approach to prevent ocular hypertension from progressing to full-blown glaucoma. However, not everyone tolerates daily drops well, and some find it challenging to adhere to an ongoing regimen. Enter Durysta, an innovative biodegradable implant that steadily releases medication to keep intraocular pressure (IOP) in check. Instead of fussing with bottles and schedules, you can let a small pellet do the work, reducing the likelihood of missed doses and potential eye damage.
It’s no surprise that treatments designed to reduce reliance on daily drops attract attention, especially among people who juggle complex health routines or have dexterity issues. Durysta offers a simpler, “insert and forget” strategy—at least for a while. But how exactly does this tiny device lower eye pressure, and what should you expect if you decide to try it? Let’s explore what Durysta is, how it’s placed in the eye, and the research behind its effectiveness for ocular hypertension management.
Unpacking Durysta: How a Novel Implant Targets Ocular Hypertension
Durysta (bimatoprost intracameral implant) reflects modern ophthalmic innovation, combining two key elements: a known intraocular pressure-lowering medication (bimatoprost) and a tiny biodegradable implant that dissolves over time. While bimatoprost has a solid track record in topical eyedrops for glaucoma (commercially known as Lumigan), Durysta offers a more sustained mode of delivery.
The Medication Behind the Implant
Bimatoprost is a prostaglandin analog that works by increasing the outflow of aqueous humor—essentially the fluid that maintains eye shape and carries nutrients within the eye. In people with ocular hypertension, fluid drainage pathways like the trabecular meshwork aren’t as efficient as they should be, leading to higher IOP. Prolonged elevation can damage the optic nerve, setting the stage for glaucoma. Prostglandin analogs such as bimatoprost and latanoprost have historically proven effective in lowering IOP by enhancing fluid outflow, making them mainstays in first-line glaucoma therapy.
A Step Toward Consistent Delivery
Yet even the best medication can’t help if patients forget to use it or struggle with side effects from preservatives. That’s where Durysta’s design comes in:
- Long-Lasting Depot: Instead of daily drops, Durysta is placed directly into the anterior chamber of the eye, slowly releasing bimatoprost for several months.
- Biodegradable Matrix: The implant itself consists of a polymer that naturally dissolves without needing surgical removal. As it degrades, it continues to release a controlled amount of medication, keeping IOP stable.
- Local Targeting: Because the drug sits right where it’s needed—in front of the iris, near the trabecular meshwork—the concentration reaching the drainage angle is higher, which may improve efficacy while reducing systemic exposure.
Addressing Adherence Hurdles
Research indicates that a significant portion of glaucoma patients are nonadherent with topical medications—some studies peg the rate at around 30–50%. Whether it’s forgetfulness, bottle discomfort, or cost issues, daily drops simply aren’t feasible for everyone. Durysta aims to tackle that hurdle by eliminating day-to-day dosing. You get the implant once, and the drug works in the background, lowering IOP without further effort.
The Biomechanics of Lowering Pressure
By gradually releasing bimatoprost, Durysta triggers several mechanisms:
- Enhanced Uveoscleral Outflow: The medication boosts the flow of aqueous humor through the uveoscleral pathway, one of the eye’s drainage routes.
- Mild Modification of Tissue: Some prostaglandin analogs may subtly alter collagen in the outflow channels, widening them so fluid leaves more easily.
- Steady Drug Levels: Instead of peaks and troughs from daily eyedrops, the implant fosters a stable drug concentration within the anterior chamber, potentially smoothing out IOP fluctuations over 24 hours.
Interestingly, while prostaglandin analog eyedrops typically reduce IOP by around 25–30%, Durysta might offer similar or slightly improved results. Still, outcomes vary by individual, making it essential to track your own responses and remain in close communication with your ophthalmologist.
Who Might Benefit the Most?
While Durysta is primarily indicated for patients with open-angle glaucoma or ocular hypertension, not everyone with these conditions automatically qualifies. It generally suits:
- Patients struggling with compliance who may skip or forget their eyedrops.
- People experiencing side effects from preservatives in eyedrops, such as redness, itching, or dryness.
- Those looking to minimize daily medication burdens, especially if they manage other chronic conditions.
- Individuals with mild to moderate disease seeking a new way to stabilize IOP while avoiding potential medication layering if multiple drops are required.
For advanced glaucoma, an ophthalmologist may opt for more aggressive or additional treatments—like filtering surgeries or laser procedures—to control severe pressure elevations. Durysta can still play a supportive role, but it’s rarely the sole therapy in complex or end-stage glaucoma.
Limitations and Initial Concerns
Despite its advantages, Durysta isn’t a panacea. Once inserted, the dosage is fixed—meaning if your IOP remains high, you may need additional interventions before the implant fully dissolves. Also, the presence of a foreign body in the eye can theoretically increase the risk of complications like endothelial cell loss or infection, though reported incidences are low. Another consideration is that Durysta isn’t a permanent solution; the effect eventually wanes as the implant dissolves, and you might need repeated placements or switch back to eye drops or other treatments in the future.
Still, for those wanting a worry-free alternative to daily drops, Durysta is a significant innovation. It signals a shift from user-dependent therapies to physician-administered solutions that ensure consistent medication delivery. The next question is: How exactly is this implant placed, and what can you expect during and after the procedure?
Step-by-Step: Insertion, Follow-Up, and Patient Experience
Although the idea of an implant inside the eye can be intimidating, Durysta insertion is designed to be a quick, minimally invasive procedure. In many cases, it’s performed in your ophthalmologist’s office under local anesthesia, and you can typically return to normal activities soon after. Understanding the logistical details can help you approach your first Durysta appointment with confidence.
Pre-Procedure Preparations
Before you’re scheduled for Durysta placement, your eye doctor will likely:
- Review Your Medical History: Confirm any allergies, prior surgeries, or concurrent medications. Certain issues—like active eye infections—may delay the procedure.
- Assess Disease Severity: Is your IOP consistently elevated despite daily drops? Are you missing doses regularly? If so, Durysta might be an ideal alternative. In mild cases, your ophthalmologist might try less invasive measures first.
- Check for Corneal or Endothelial Health: Durysta’s presence in the anterior chamber may raise concerns if you already have compromised corneal endothelium. An endothelial cell count test can determine if your cornea is robust enough to handle the implant.
- Discuss Risks and Benefits: Be sure to ask questions about complications, success rates, and how Durysta may affect any future eye procedures.
Your doctor may also advise whether to keep taking your current eyedrops up until the day of the implant. Typically, discontinuing or tapering might happen once Durysta begins to take effect, but plans can differ based on your specific ocular condition.
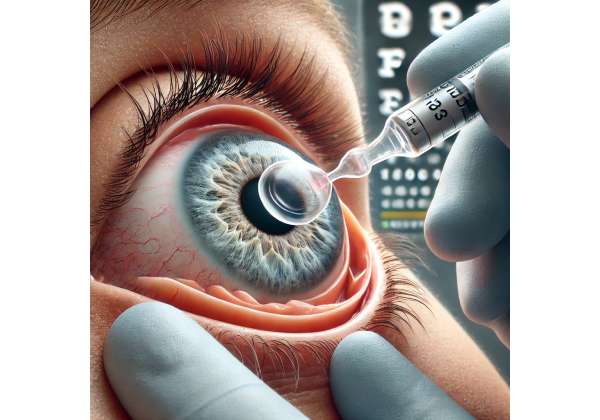
The Insertion Process
On the day of the procedure, expect a relatively streamlined experience:
- Numbing the Eye: To keep discomfort minimal, you’ll receive anesthetic drops. Some doctors might place a mild sedative in the eye if you’re particularly anxious.
- Preparation and Positioning: You’ll be seated or reclined to give your ophthalmologist clear access. An eyelid speculum may gently hold your lids apart.
- Micro-Injection: Durysta comes in a pre-loaded applicator with a tiny needle. After positioning the applicator at the proper angle, the doctor will release the pellet into the anterior chamber, just in front of the iris. This is often described as a slight pressure rather than pain.
- Immediate Post-Placement Check: The physician observes the pellet’s position, ensuring it’s in the correct location and not floating in a way that might block your vision. Some people see a small dot or shadow for a brief time until the implant settles.
Overall, the procedure can take just a few minutes. Many patients are pleasantly surprised by how quick and relatively painless it feels. You might notice mild irritation or redness afterward, but serious complications are rare.
Recovery and Follow-Up Appointments
Most individuals can go about their day immediately. Still, doctors often recommend:
- Avoiding Strenuous Activities: For about 24 hours, skip heavy lifting or rigorous workouts to minimize pressure fluctuations in the eye.
- Wearing Protective Eyewear: If you expect to be in dusty or windy environments, protect your eye from debris that could irritate or introduce bacteria.
- Returning for IOP Checks: Your ophthalmologist will schedule follow-up visits to measure your eye pressure and confirm that the implant is working. Expect an appointment a week or two after insertion, then periodic checks over the next months.
- Monitoring for Unusual Symptoms: Cloudiness, severe pain, or a sudden dip in vision aren’t typical—call your doctor if they arise, as they could signal rare but urgent issues like infection or inflammatory reactions.
Dual or Repeated Implants
Because each Durysta implant eventually dissolves, some patients may need another insertion once the drug’s effect tapers off (often between three and six months, sometimes longer). Whether you’ll switch eyes or re-implant in the same eye depends on your disease progression and how effectively the first Durysta controlled your IOP. In clinical practice, repeated implants have been performed successfully, but your doctor will weigh any potential cumulative endothelial cell impact if you have multiple implants over time.
Integrating Durysta with Other Therapies
It’s not uncommon for patients to remain on a simplified drop regimen in conjunction with Durysta if their eye pressure requires multi-angled control. For instance, a beta-blocker or carbonic anhydrase inhibitor might be used in tandem to get IOP to the ideal target. On the flip side, some patients find that Durysta alone meets their needs, freeing them from daily drop use altogether.
Patient Perspectives and Comfort
Most patients appreciate the hands-off convenience. If you’ve struggled with applying drops consistently—perhaps due to tremors or forgetfulness—Durysta can be a welcome relief. There’s also the intangible benefit of decreased anxiety: no daily reminder that “something is wrong with my eyes.” Instead, you trust the implant to do its job, under periodic medical supervision.
Of course, no approach is foolproof. If you require multiple Durysta implants to maintain IOP control and your cornea shows signs of stress, your ophthalmologist may recommend switching back to drops or exploring procedures like selective laser trabeculoplasty (SLT). In that sense, Durysta fits within a broad array of glaucoma and ocular hypertension solutions, each tailored to different severity levels and patient preferences.
For those seeking evidence of how well this implant stands up to clinical scrutiny, the good news is that a growing body of research has examined Durysta’s track record. Let’s take a closer look at the studies, data, and real-world experiences guiding its use.
What Clinical Trials and Observations Tell Us About Durysta
Durysta’s path from concept to FDA approval was driven by rigorous research—comparing its sustained-release mechanism against standard treatments for ocular hypertension. Over the past few years, a handful of pivotal studies have not only confirmed its efficacy but also shaped guidelines for its use in everyday practice.
Pivotal Phase III Trials
One of the most influential was the ARTEMIS program, encompassing two randomized, multicenter Phase III trials that evaluated the safety and efficacy of bimatoprost intracameral implant:
- Study Design: Participants with open-angle glaucoma or ocular hypertension were randomized to receive Durysta implants or daily topical bimatoprost drops.
- Duration: Researchers followed patients for up to two years, focusing on IOP levels, visual field tests, and any ocular complications that arose.
- Key Findings: According to results published in the Journal of Glaucoma (2020), Durysta’s ability to lower IOP was comparable to daily drops for many patients. A significant portion of participants needed fewer or no topical adjunctive therapies during the first six months. Adverse events—like mild eye redness—were generally mild and transient.
These results played a major role in Durysta gaining FDA approval in the United States for patients with ocular hypertension or open-angle glaucoma who want an alternative to daily drop regimens.
Longevity and Repeatability Studies
Further research has delved into how long a single Durysta implant can maintain lowered IOP and whether subsequent implants remain effective:
- Duration of Efficacy: Some studies show that a single implant can offer meaningful pressure control for about four to six months, though individual variability exists. A subset of patients might maintain target IOP for eight months or longer.
- Reimplantation Outcomes: A second or third Durysta implant often continues to keep IOP in check, albeit with an incremental increase in corneal endothelial cell loss in some cases. Thus, the practice of repeat implantation warrants close monitoring of corneal health.
Comparative Evaluations Against SLT and Other Therapies
While most trials compare Durysta with daily eyedrops, a few institutions have looked at how it stacks up against other interventions:
- Laser Therapies: Selective laser trabeculoplasty (SLT) is a well-regarded outpatient procedure to improve outflow in ocular hypertension. A 2021 pilot study in the American Journal of Ophthalmology observed that Durysta’s short-to-mid-term results matched or slightly exceeded SLT in maintaining stable IOP, though SLT might remain the less invasive or less device-oriented option for certain individuals.
- Filtration Surgery or MIGS (Minimally Invasive Glaucoma Surgery): For patients at moderate or advanced stages, Durysta might not fully replace MIGS or a trabeculectomy. However, in mild to moderate cases, it can delay the need for more invasive procedures.
Real-World Observational Data
Beyond controlled trials, everyday practice reports paint a generally positive picture:
- Patient Satisfaction: Many who switch from daily drops to Durysta say they find it liberating not to worry about compliance or the stinging sensation from certain solutions.
- IOP Fluctuation Reduction: Some clinicians note that Durysta offers more stable, round-the-clock IOP control, reducing the peaks and troughs associated with drop-based therapy.
- Minimal Intraoperative Discomfort: The short, in-office procedure often surprises patients with its ease, parallel to or even simpler than certain laser treatments.
Potential Caveats from Ongoing Research
Still, the field is in constant evolution:
- Endothelial Cell Considerations: A small fraction of users exhibit a more noticeable decline in corneal endothelial cells. For that reason, Durysta is typically limited to a finite number of implants per eye—often one or two total—for now. Studies aim to refine guidelines on safe reimplantation intervals.
- Longer-Term Outcomes: Five-year data remains limited. Although early signals are promising, robust, long-duration follow-ups are needed to confirm the best usage patterns and assess any late-onset complications.
- Cost-Effectiveness: Some publications examine the financial dimension, comparing Durysta’s initial outlay with the cumulative costs of prescription drops over years. This analysis varies widely depending on healthcare system coverage and patient adherence.
While more research will undoubtedly fine-tune Durysta’s place in the ocular hypertension arsenal, the consensus so far is that it delivers meaningful, consistent pressure reduction for suitable candidates. Let’s dive deeper into how it measures up in terms of success rates, safety profiles, and overall acceptance among eye care experts.
Weighing Efficacy and Safety for Intraocular Pressure Control
Durysta’s primary claim to fame is reducing IOP to protect against optic nerve damage. However, no treatment is completely risk-free. Understanding the pros and cons, as well as the typical outcomes, can guide a balanced decision about whether Durysta fits your particular situation.
Effectiveness Snapshot
- Reduced IOP by 20–35%: Studies commonly report a 20–35% drop in eye pressure from baseline—an impressive range that often meets or exceeds recommended target pressures for mild to moderate glaucoma or ocular hypertension.
- Sustainability Over Months: Many patients maintain safe IOP levels for four to six months on average, occasionally longer.
- Less Variation: Constant drug release helps avoid the day-to-day dips and spikes seen with missed or incorrectly applied drops.
Key Safety Highlights
- Low Infection Risk: Thorough aseptic technique during insertion keeps infection complications (endophthalmitis) rare.
- Minimal Discomfort: Most side effects, such as mild soreness or redness, resolve quickly.
- Corneal Health Monitoring: Because repeated Durysta might affect endothelial cells, doctors track this parameter at follow-up appointments. In the vast majority of cases, changes are negligible or within acceptable limits.
Who Should Exercise Caution?
- Already Compromised Endothelium: If you have a history of corneal problems (like Fuchs’ endothelial dystrophy) or previous surgeries that reduced endothelial cell counts, your ophthalmologist may hesitate to place multiple implants.
- Advanced Disease: If your IOP is extremely high or you’ve experienced significant optic nerve damage, you may need more aggressive or multi-modal therapy. Durysta alone might be insufficient to bring pressure into a safe range.
- Sensitivity to Bimatoprost: Some individuals are sensitive to the drug’s components, though allergic reactions are uncommon.
When weighed against the possibility of slowed glaucoma progression and a simpler daily routine, Durysta’s advantages often stand out. Still, each patient’s medical context matters—no one solution works universally, and doctors frequently personalize therapy to meet unique needs. For those who find Durysta appealing yet worry about cost, let’s break down how the pricing generally works.
Examining Pricing Structures and Coverage Options
Like many modern eye treatments, Durysta can carry a higher upfront cost than a prescription for generic eyedrops. However, the long-term savings—financial and otherwise—may offset that initial expense. Factors influencing the final price include:
- Regional Healthcare Systems: In some countries, national insurance covers a large share of the cost if Durysta is indicated for ocular hypertension. In the U.S., coverage varies widely by plan.
- Insurance Tiers: Some private insurers classify Durysta as a “medical benefit” since a physician administers it in-office, while others treat it as a pharmacy benefit. Reimbursements and copays can thus differ drastically.
- Out-of-Pocket Estimates: Without insurance, Durysta can run from \$1,000 to \$3,000 per implant in the U.S. The cost might include the procedure fee, follow-up visits, and the implant itself.
- Patient Assistance Programs: Certain pharmaceutical manufacturers or nonprofit organizations offer financial aid or discount programs, particularly for people with limited resources.
Disclaimer:
This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for personalized guidance.
If you found this deep dive into Durysta helpful, consider sharing it on social media—someone else could benefit from learning about this cutting-edge way to manage ocular hypertension.