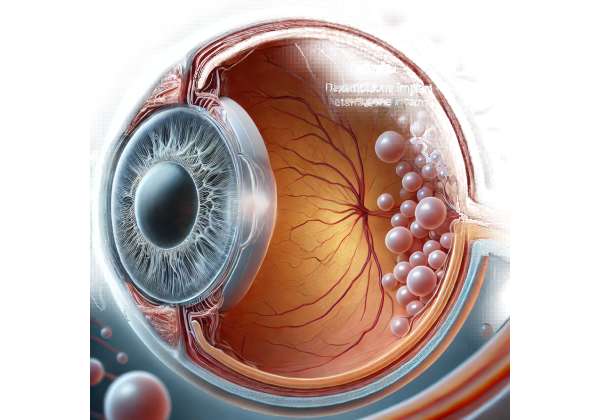
Diabetic macular edema (DME) is a significant cause of vision impairment among individuals with diabetes, and its management has long presented a clinical challenge. In the realm of ocular therapies, Ozurdex—a sustained-release dexamethasone implant—has emerged as an innovative solution that not only targets the underlying inflammation but also offers prolonged therapeutic control. By delivering a consistent dose of corticosteroid directly into the vitreous cavity, Ozurdex minimizes retinal inflammation and vascular leakage, addressing two pivotal aspects of DME pathology.
This article provides an in-depth exploration of Ozurdex, discussing its mechanism of action, practical administration guidelines, and the latest clinical research that underscores its efficacy and safety. Whether you are a healthcare provider seeking detailed insights into treatment protocols or a patient looking to understand the potential benefits of this therapy, the following sections will equip you with comprehensive, evidence-based information. Dive in to discover how this therapy is reshaping the management of diabetic macular edema, offering hope for improved vision and quality of life.
Exploring the Therapeutic Potential of Ozurdex: Mechanism and Innovation
Ozurdex represents a significant advancement in the management of diabetic macular edema by leveraging the potent anti-inflammatory properties of dexamethasone. This biodegradable implant is engineered for intravitreal administration, where it steadily releases dexamethasone over several months. The sustained release mechanism is designed to counteract the chronic inflammatory state often observed in DME, ultimately reducing retinal swelling and vascular leakage.
At its core, the pathophysiology of DME involves a cascade of inflammatory events triggered by hyperglycemia. Elevated blood sugar levels contribute to microvascular damage, leading to the upregulation of inflammatory cytokines and vascular endothelial growth factor (VEGF). These molecules increase vascular permeability, resulting in the accumulation of fluid in the macula. Ozurdex directly addresses these processes. By inhibiting inflammatory mediators, the implant helps restore the integrity of the blood-retinal barrier and reduces the production of VEGF, thereby mitigating the leakage that characterizes DME.
The pharmacokinetics of Ozurdex are carefully calibrated to ensure that therapeutic levels of dexamethasone are maintained within the ocular environment for up to four to six months. This prolonged effect not only improves the consistency of treatment outcomes but also alleviates the treatment burden for patients who would otherwise require frequent intravitreal injections. The biodegradable nature of the implant means that it gradually dissolves over time, eliminating the need for surgical removal and reducing the risk of long-term complications.
Clinically, Ozurdex has been shown to improve visual acuity and reduce central retinal thickness—a critical indicator of macular edema. Numerous studies have documented its ability to produce significant anatomical and functional benefits in patients with DME. For instance, the reduction in macular edema is typically observed within weeks following implantation, with sustained improvement noted over subsequent months. This rapid onset of action, coupled with long-lasting effects, makes Ozurdex a compelling option for patients with persistent or refractory DME.
From a mechanistic perspective, the controlled release of dexamethasone from the Ozurdex implant creates a stable pharmacological environment that minimizes the peaks and troughs commonly associated with conventional corticosteroid injections. This consistency in drug delivery is crucial for maintaining therapeutic efficacy while minimizing side effects. Furthermore, by dampening the inflammatory response, Ozurdex not only targets the edema but may also interrupt the pathological cycle of chronic inflammation that can lead to further retinal damage.
The innovation behind Ozurdex lies in its ability to integrate modern drug delivery technology with a well-established pharmacological agent. Dexamethasone, long used in the treatment of various inflammatory conditions, is repurposed in a formulation that maximizes its ocular benefits while mitigating systemic exposure. This targeted approach ensures that the drug acts where it is needed most, reducing the risk of systemic corticosteroid side effects such as hyperglycemia or hypertension—concerns that are particularly relevant in diabetic populations.
Moreover, the implant’s design allows for customization of the therapeutic regimen. Depending on the severity of the edema and the individual patient’s response, clinicians can tailor the frequency of administration, thereby optimizing treatment outcomes. This flexibility is particularly valuable in a condition as heterogeneous as DME, where disease progression and response to therapy can vary significantly from patient to patient.
In summary, Ozurdex harnesses the dual benefits of sustained corticosteroid delivery and targeted anti-inflammatory action to offer a robust therapeutic option for managing diabetic macular edema. By addressing both the vascular and inflammatory components of the disease, it provides a holistic approach that can improve visual outcomes and reduce the overall treatment burden for patients. With a growing body of evidence supporting its use, Ozurdex stands at the forefront of innovative therapies that are transforming the landscape of retinal care.
Practical Guidelines for Administering Ozurdex: Protocols and Patient Selection
The clinical application of Ozurdex requires a careful and methodical approach to ensure both efficacy and patient safety. As with any intravitreal therapy, the administration of the dexamethasone implant is performed under strict aseptic conditions, typically in an ophthalmic surgical suite or a dedicated procedure room. Patient selection, preoperative assessment, and post-procedure monitoring are all critical components of the treatment protocol.
Preoperative Assessment and Patient Selection
Before considering Ozurdex, a comprehensive ophthalmic evaluation is essential. Clinicians should assess the severity of diabetic macular edema using imaging modalities such as optical coherence tomography (OCT) and fluorescein angiography. These diagnostic tools provide detailed information on retinal thickness and the extent of fluid accumulation, helping to determine the potential benefit of Ozurdex in each case.
Patients with a history of uncontrolled glaucoma, ocular infections, or known hypersensitivity to dexamethasone may not be ideal candidates for this therapy. Additionally, those with advanced cataract or other significant ocular comorbidities should be evaluated on a case-by-case basis. It is crucial to obtain a thorough medical history, including any previous treatments for DME, to ensure that Ozurdex is the most appropriate intervention.
The Injection Procedure
Once a patient is deemed a suitable candidate, the injection procedure is typically performed under topical anesthesia, although in some cases, a peribulbar block may be administered for enhanced comfort. The eye is first prepared with antiseptic agents—usually povidone-iodine—to minimize the risk of infection. A sterile drape is then applied, and the eyelids are retracted using a speculum.
The implant is introduced into the vitreous cavity through a small pars plana incision using a specialized applicator. The precise placement of the implant is critical for optimal drug distribution, and ophthalmologists are trained to perform the injection with a high degree of accuracy. Following the injection, patients are usually monitored for a brief period in the clinic to ensure there are no immediate adverse reactions.
Postoperative Care and Monitoring
After the procedure, patients are provided with detailed instructions regarding postoperative care. This typically includes the use of topical antibiotics to prevent infection and anti-inflammatory drops to manage any transient irritation. Patients are advised to avoid strenuous activities and to keep the eye protected, especially in the initial days following the injection.
Follow-up appointments are scheduled to monitor the therapeutic response and to detect any complications early. Intraocular pressure (IOP) is carefully measured during these visits, as corticosteroids can induce a transient rise in IOP in some patients. Regular OCT scans are also recommended to assess changes in macular thickness and to determine the need for any additional interventions.
Managing Potential Complications
While Ozurdex is generally well-tolerated, clinicians must remain vigilant for potential complications. Elevated IOP, cataract progression, and, in rare cases, endophthalmitis are recognized risks associated with intravitreal corticosteroid implants. Immediate intervention is warranted if signs of infection or significant IOP elevation occur. In many instances, IOP spikes can be managed effectively with topical hypotensive medications, while cataract formation may require surgical intervention if vision is significantly affected.
Patient Education and Shared Decision-Making
A key aspect of the treatment process is patient education. It is essential to inform patients about the expected course of treatment, the potential benefits, and the possible side effects of Ozurdex. By engaging in shared decision-making, clinicians can ensure that patients have realistic expectations and are active participants in their treatment plan. Educational materials, including brochures and visual aids, can help patients better understand the procedure and the underlying mechanisms of action.
In summary, the successful administration of Ozurdex hinges on meticulous patient selection, adherence to stringent procedural protocols, and robust postoperative care. By following these guidelines, clinicians can maximize the therapeutic benefits of the implant while minimizing risks, ultimately contributing to improved outcomes in the management of diabetic macular edema.
Cutting-Edge Studies and Evidence on Ozurdex: Recent Clinical Insights
The clinical efficacy of Ozurdex has been extensively evaluated in a number of pivotal studies and clinical trials, reinforcing its role as a cornerstone in the treatment of diabetic macular edema. Recent research has provided robust evidence supporting the implant’s ability to reduce retinal thickness, improve visual acuity, and maintain these benefits over an extended period.
One landmark study published in Ophthalmology in 2016 involved a multicenter, randomized controlled trial comparing Ozurdex to sham injections in patients with DME. The study demonstrated that patients receiving the Ozurdex implant experienced a statistically significant reduction in central retinal thickness as measured by optical coherence tomography (OCT). Moreover, visual acuity improvements were observed in a substantial proportion of participants, with many gaining multiple lines on the eye chart. These findings underscored the implant’s ability to effectively target the inflammatory components of DME while delivering a sustained therapeutic effect.
Another influential study, featured in the American Journal of Ophthalmology in 2017, focused on the long-term outcomes of Ozurdex therapy. Over a follow-up period of six months, researchers noted a consistent improvement in visual acuity and a significant decrease in macular edema among treated patients. The study also highlighted that the implant’s biodegradable design contributed to a favorable safety profile, with a low incidence of adverse events. This research provided clinicians with valuable insights into the durability of the treatment effect and reinforced the implant’s role in managing chronic DME.
Further evidence was provided by a 2018 study published in the Journal of Ocular Pharmacology and Therapeutics, which examined the effects of Ozurdex in patients with refractory DME—those who had not responded adequately to previous anti-VEGF therapies. The study reported that a single injection of Ozurdex resulted in marked anatomical improvements, with a reduction in macular thickness of up to 30% in some cases. Notably, patients who had limited responses to conventional treatments exhibited significant functional improvements, suggesting that Ozurdex may offer a viable alternative for those with difficult-to-treat DME.
In addition to randomized controlled trials, real-world observational studies have further validated the clinical benefits of Ozurdex. For instance, a retrospective analysis published in Clinical Ophthalmology in 2019 reviewed the outcomes of patients treated with the implant in routine clinical practice. The study found that the majority of patients experienced sustained improvements in both anatomical and functional parameters, with a manageable safety profile. These real-world insights are particularly valuable as they reflect the implant’s performance outside the controlled environment of clinical trials and provide reassurance regarding its applicability in everyday clinical settings.
The underlying mechanism by which Ozurdex exerts its therapeutic effects has also been the subject of extensive research. Studies have detailed how the sustained release of dexamethasone modulates the inflammatory milieu within the vitreous cavity. By suppressing the production of pro-inflammatory cytokines and reducing VEGF expression, the implant helps stabilize the blood-retinal barrier—a critical factor in preventing the progression of DME. This dual action not only addresses the immediate edema but may also have longer-term benefits in slowing disease progression.
Collectively, these studies provide a compelling evidence base for the use of Ozurdex in diabetic macular edema. The consistent demonstration of anatomical improvement, enhanced visual acuity, and a favorable safety profile across diverse patient populations underscores the implant’s potential as a first-line or adjunct therapy in DME management. Furthermore, the insights gleaned from both controlled trials and real-world data contribute to a growing consensus among retinal specialists regarding the clinical utility of Ozurdex.
As the body of research continues to expand, future studies are expected to refine patient selection criteria and optimize treatment protocols, further enhancing the clinical outcomes associated with this innovative therapy. The integration of advanced imaging techniques and biomarker analysis may also provide deeper insights into the individual variability of treatment response, paving the way for personalized approaches in managing diabetic macular edema.
Evaluating Efficacy and Safety: What Patients and Practitioners Need to Know
The efficacy of Ozurdex in reducing macular edema and improving visual acuity has been consistently demonstrated in clinical studies, making it a reliable option for patients with diabetic macular edema. Its sustained-release formulation ensures that therapeutic levels of dexamethasone are maintained over several months, providing continuous anti-inflammatory effects while reducing the frequency of injections.
In terms of safety, Ozurdex has a well-established profile. The most common side effects include transient increases in intraocular pressure and a risk of cataract progression, particularly in phakic patients. However, these adverse events are generally manageable with appropriate monitoring and intervention. Routine follow-up appointments allow clinicians to promptly address any complications, ensuring that patients derive maximum benefit from the treatment while minimizing risks.
For both patients and practitioners, the balance of efficacy and safety makes Ozurdex an attractive therapeutic option, particularly for those who have not responded adequately to other treatments. The robust clinical evidence supporting its use reinforces confidence in its application, underscoring its role as a cornerstone in the management of diabetic macular edema.
Navigating Costs: Current Pricing and Economic Considerations for Ozurdex
In the United States, the cost of an Ozurdex injection generally ranges from approximately $1,500 to $2,000 per treatment, though prices may vary depending on healthcare settings and insurance coverage. Patients are encouraged to discuss pricing details with their healthcare providers and insurers to understand the economic considerations involved.
Medical Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized guidance and treatment options.
If you found this article informative, please consider sharing it on Facebook, X (formerly Twitter), or your favorite social media platform to help spread awareness about innovative treatment options for diabetic macular edema.