Pneumatic retinopexy represents one of the most exciting advances in ophthalmic procedures, offering patients a less invasive option for retinal detachment repair. This innovative therapy leverages a simple yet powerful concept: by injecting a small gas bubble into the eye, the detached retina can be gently repositioned against the underlying tissue. When combined with precise laser photocoagulation or cryotherapy, the treatment effectively seals retinal tears, facilitating natural reattachment. Unlike traditional surgical interventions that often require extensive incisions and prolonged recovery times, pneumatic retinopexy is typically performed in an outpatient setting under local anesthesia. This means less disruption to daily life and a faster return to normal activities.
The procedure’s minimally invasive nature not only reduces the risks associated with more invasive surgeries but also minimizes postoperative discomfort. Patients appreciate the convenience of a treatment that avoids the need for a hospital stay and allows for a more comfortable recovery in the familiar environment of their home. In today’s era of patient-centered care, where both efficacy and quality of life are paramount, pneumatic retinopexy stands out as a viable option for many individuals facing retinal challenges.
Moreover, advancements in imaging technology and surgical techniques have refined the patient selection process, ensuring that the benefits of pneumatic retinopexy are maximized while minimizing potential complications. As a result, this therapy has garnered significant attention from both practitioners and researchers, driving a wealth of clinical studies and innovations in treatment protocols. Whether you’re an individual exploring treatment options or a healthcare provider seeking the latest developments in retinal repair, pneumatic retinopexy offers a compelling combination of safety, efficiency, and patient comfort.
Exploring the Innovative Approach of Pneumatic Retinopexy
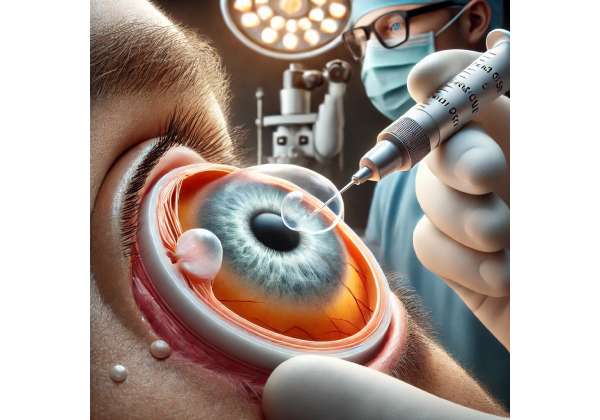
Pneumatic retinopexy is a revolutionary procedure that has transformed the landscape of retinal detachment repair. At its core, the technique involves the injection of a small, expandable gas bubble into the vitreous cavity. This bubble acts as a temporary internal tamponade, pressing the retina back toward the underlying retinal pigment epithelium. The procedure’s simplicity belies its sophisticated design, combining mechanical repositioning with the biological healing process induced by laser photocoagulation or cryotherapy.
Historically, retinal detachment repair often necessitated more invasive techniques, such as scleral buckling or pars plana vitrectomy. These procedures, while effective, could entail significant surgical trauma, lengthy recovery periods, and higher risks of complications. Pneumatic retinopexy emerged as a response to these challenges, offering a less aggressive yet highly effective alternative. Its development was driven by the desire to reduce surgical morbidity and improve patient outcomes by simplifying the repair process without compromising on efficacy.
One of the key advantages of pneumatic retinopexy is its minimally invasive nature. The procedure is usually performed in an outpatient clinic, sparing patients the rigors of prolonged hospitalization and general anesthesia. This outpatient approach not only reduces healthcare costs but also significantly enhances patient comfort and convenience. In many cases, patients experience rapid visual recovery, allowing them to resume daily activities sooner than those undergoing more extensive surgeries.
The success of this procedure hinges on careful patient selection. Ideal candidates are those with uncomplicated retinal detachments—typically characterized by a single break located in the superior retina. Detailed preoperative imaging, including optical coherence tomography (OCT) and B-scan ultrasonography, plays a critical role in determining the suitability of pneumatic retinopexy. These imaging techniques help clinicians identify the precise location and extent of the retinal tear, ensuring that the gas bubble will adequately tamponade the affected area.
Once the gas bubble is injected, patient positioning becomes paramount. The patient is instructed to maintain a specific head position that allows the bubble to press directly against the retinal break. This position is usually maintained for several days, enabling the retinal tissue to reattach firmly. During this period, adjunctive laser or cryotherapy is applied around the tear to create chorioretinal adhesions, which act as permanent “glue” to seal the retinal break.
The biological processes initiated by pneumatic retinopexy are as crucial as the mechanical repositioning of the retina. The gas bubble’s pressure not only repositions the retina but also facilitates the migration of retinal pigment epithelial cells to the tear site, promoting natural healing. This dual mechanism of action—mechanical tamponade combined with biological adhesion—underpins the procedure’s high success rate in appropriately selected patients.
Clinical experience and studies have demonstrated that pneumatic retinopexy can achieve reattachment rates comparable to those of more invasive surgeries, with the added benefits of reduced surgical time and lower postoperative discomfort. However, the procedure is not without its limitations. For example, it may not be suitable for patients with multiple retinal breaks or inferior detachments where the gas bubble cannot adequately tamponade the tear. Despite these limitations, ongoing refinements in patient selection and postoperative management continue to expand the indications for this therapy.
Advancements in surgical instrumentation and intraoperative imaging have further enhanced the safety and efficacy of pneumatic retinopexy. These technological improvements allow for greater precision in gas injection and more accurate localization of retinal breaks, thereby reducing the risk of complications such as cataract formation or secondary retinal tears. As research and clinical experience evolve, the procedure is likely to be refined even further, cementing its role as a frontline treatment option for selected cases of retinal detachment.
In summary, pneumatic retinopexy is an exemplary model of how modern ophthalmology can blend innovation with practicality. By harnessing a minimally invasive technique that combines mechanical repositioning with biological healing, this procedure offers patients a streamlined path to visual recovery while mitigating the risks associated with more invasive surgical alternatives.
Step-by-Step: How Pneumatic Retinopexy Is Performed
The procedure begins with a comprehensive preoperative evaluation. Patients undergo a series of imaging studies, such as optical coherence tomography (OCT) and B-scan ultrasonography, to determine the exact location, size, and configuration of the retinal tear. This meticulous assessment is crucial, as the success of pneumatic retinopexy depends heavily on the accurate identification of the affected area. Only patients with a single, superior retinal break and no evidence of proliferative vitreoretinopathy are considered ideal candidates.
Once patient selection is confirmed, the procedure is typically scheduled as an outpatient intervention. The patient receives local anesthesia to ensure comfort throughout the procedure. In some instances, mild sedation may be administered to alleviate any anxiety. With the eye adequately anesthetized, the clinician proceeds to prepare the ocular surface using antiseptic solutions to minimize the risk of infection.
The core of the procedure involves the injection of a carefully measured volume of expansile gas—commonly perfluoropropane (C3F8) or sulfur hexafluoride (SF6)—into the vitreous cavity. This gas is chosen for its ability to expand after injection, thereby creating a bubble large enough to press the detached retina against the underlying tissue. The injection is performed with precision, using a fine gauge needle to minimize any trauma to the ocular structures. The choice between C3F8 and SF6 is based on the desired duration of the gas bubble’s presence in the eye; while SF6 is absorbed more quickly, C3F8 remains longer and may be preferable for more complex detachments.
Immediately following the gas injection, the patient is instructed on the importance of postoperative positioning. Proper head positioning is critical because it ensures that the gas bubble is directed toward the retinal break. Patients may be required to maintain this position for several days, with periodic breaks as advised by their clinician. This phase is vital, as the bubble’s pressure must be consistently applied to facilitate the reattachment process.
Once the gas bubble is in place, the next step involves applying laser photocoagulation or cryotherapy to the margins of the retinal tear. These techniques create small burns or freeze-induced scars around the break, which eventually form strong adhesions between the retina and the underlying tissue. The timing of these adjunctive treatments can vary; in some cases, laser therapy is applied immediately after the gas injection, while in others, it is delayed until the retina has repositioned. The decision is made based on the specifics of the detachment and the clinician’s judgment.
Throughout the procedure, the clinician monitors intraocular pressure and the overall status of the retina using indirect ophthalmoscopy. This real-time observation is essential to ensure that the gas bubble is achieving the desired effect and that there are no unexpected complications. The entire process typically takes less than an hour, underscoring its efficiency compared to more invasive surgical methods.
Postoperatively, patients receive detailed instructions regarding head positioning, activity restrictions, and the use of prescribed medications such as anti-inflammatory and antibiotic drops. Follow-up visits are scheduled to monitor the reattachment progress and to address any potential complications early on. These follow-up appointments may include repeat imaging studies to confirm that the retinal tear has sealed effectively and that the retina remains attached.
Patient education is a cornerstone of the procedure. Before discharge, clinicians ensure that patients understand the importance of adhering to postoperative guidelines. This education not only enhances the chances of a successful outcome but also helps manage expectations regarding recovery time and visual improvement.
In essence, the step-by-step process of pneumatic retinopexy reflects a careful balance between advanced technology and patient-centered care. From the initial evaluation to the final postoperative check-ups, every stage is designed to maximize therapeutic success while minimizing discomfort and risk. The streamlined nature of the procedure, combined with its outpatient setting and rapid recovery timeline, makes it an attractive option for many patients facing retinal detachment.
Cutting-Edge Research: What Studies Reveal About Pneumatic Retinopexy
Recent research has played a pivotal role in validating the effectiveness and expanding the indications of pneumatic retinopexy. Numerous clinical studies have compared this technique with traditional methods, such as scleral buckling and pars plana vitrectomy, revealing comparable reattachment rates in carefully selected cases.
A notable study published in the American Journal of Ophthalmology (2017) evaluated over 150 patients undergoing pneumatic retinopexy. The researchers reported an initial reattachment success rate of approximately 85%, with many patients achieving full retinal reattachment after a single procedure. The study emphasized that patient selection was critical, noting that individuals with a single superior break and minimal vitreous traction had the best outcomes. This research provided robust evidence that, when used under appropriate conditions, pneumatic retinopexy offers outcomes similar to more invasive procedures, but with the added benefits of shorter recovery times and reduced surgical trauma.
Another influential investigation, featured in Retina (2016), focused on the long-term visual outcomes following pneumatic retinopexy. The findings indicated that patients not only experienced rapid anatomical reattachment but also significant improvements in visual acuity over a follow-up period of 12 to 24 months. The study highlighted the role of adjunctive laser photocoagulation in consolidating retinal adhesion and preventing recurrent detachments. These results have reinforced the procedure’s status as a reliable option for select cases of retinal detachment, particularly in a modern clinical setting where patient quality of life is a primary concern.
Additional research published in the Journal of Ophthalmic Surgery (2018) delved into the cost-effectiveness of pneumatic retinopexy compared to more traditional surgical interventions. The study concluded that, aside from its clinical benefits, the procedure significantly reduced overall healthcare expenditures. Factors such as the avoidance of general anesthesia, shorter operating times, and reduced hospital stays contributed to its economic advantage. Such findings are particularly relevant in today’s healthcare environment, where cost-efficiency and resource management are as important as clinical outcomes.
Beyond randomized clinical trials, observational studies and case reports have enriched our understanding of pneumatic retinopexy’s practical applications. For example, several case series have documented the successful use of this technique in challenging scenarios, including cases where patients had contraindications to more invasive procedures. These real-world insights underscore the versatility of pneumatic retinopexy and its potential to be adapted for a broader range of clinical presentations.
Furthermore, advancements in imaging and surgical instrumentation have paved the way for ongoing refinements in the procedure. Enhanced intraoperative imaging allows surgeons to more precisely target retinal tears, thereby increasing the likelihood of a successful reattachment. This technology-driven evolution, corroborated by clinical research, continues to improve the safety profile and overall efficacy of pneumatic retinopexy.
While the body of evidence is robust, researchers acknowledge that long-term studies are still needed to evaluate the durability of retinal reattachment and the incidence of late complications. Nevertheless, the current literature consistently supports the notion that pneumatic retinopexy is a safe, effective, and economically viable option for managing specific types of retinal detachment. The convergence of clinical data, technological improvements, and cost analyses has cemented its role as a valuable tool in modern ophthalmology.
Evaluating the Safety and Efficacy of Pneumatic Retinopexy
Pneumatic retinopexy is widely regarded as a safe and effective procedure when applied to well-selected cases. With success rates frequently exceeding 80% in ideal candidates, this technique offers comparable outcomes to more invasive surgeries while significantly reducing patient morbidity. The minimally invasive nature of the procedure minimizes risks such as infection, hemorrhage, and postoperative inflammation. However, complications—though infrequent—can include secondary retinal tears, elevated intraocular pressure, or the need for repeat interventions.
Continuous monitoring during and after the procedure, combined with strict adherence to postoperative positioning and medication regimens, has proven instrumental in maintaining its high safety profile. Overall, patients typically experience a smoother recovery process, with many returning to their routine activities faster than those undergoing conventional retinal detachment repairs.
Financial Considerations and Therapy Cost Insights
In terms of cost, pneumatic retinopexy is often more affordable than traditional surgical options. Depending on geographic location and facility, the procedure generally ranges from approximately \$3,000 to \$5,000. This cost-effectiveness is attributed to its outpatient nature, reduced anesthesia requirements, and shorter operative times.
Medical Disclaimer: The information provided in this article is intended for informational purposes only and should not be considered as medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment recommendations.
If you found this article helpful, please consider sharing it on your preferred social platforms such as Facebook or X.