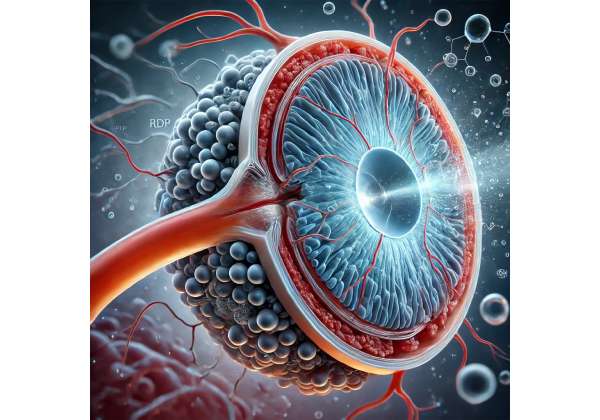
Have you ever imagined a targeted therapy that can promote healthier cell function in the retina and potentially slow down vision decline? Retinal-Derived Peptide (RDP) is stepping into the spotlight as a transformative option, aimed at supporting the eye’s natural regenerative pathways. Rather than relying solely on existing medications that control symptoms, RDP strives to address fundamental mechanisms in the retina itself, potentially creating better conditions for long-term stabilization or improvement in visual performance.
Advances in ophthalmic science have shown that certain peptides, derived from retinal tissue, exhibit protective and nurturing qualities for the cells at the back of the eye. By harnessing these peptides, RDP therapy aspires to help the body shield delicate retinal structures from oxidative stress and inflammation, which are major contributors to progressive vision deterioration. While researchers continue to explore the full extent of its impact, many experts are optimistic that RDP may represent a breakthrough—complementing or possibly even enhancing the effects of traditional methods.
In this article, we’ll delve into the emerging promise of Retinal-Derived Peptide, highlighting how it is being integrated into therapeutic strategies, the protocols involved, key findings from current studies, and what to expect regarding effectiveness, safety, and cost. By bringing together cutting-edge research and real-world clinical insights, RDP offers a glimpse of how future medicine might help maintain or restore vision in conditions like Age-Related Macular Degeneration (AMD).
Breakthrough Perspective on RDP’s Potential
Retinal-Derived Peptide stands out in the evolving sphere of therapies designed to support retinal health. Unlike conventional interventions that may zero in on halting abnormal blood vessel growth or controlling inflammation, RDP seeks a more direct engagement with the retina’s cellular environment. At its core, RDP is a sequence of amino acids—think of it as a small protein fragment—originally found within retinal tissues. Scientists hypothesize that these peptides carry signaling capabilities to strengthen neurons, bolster protective responses, and reduce harmful processes in the eye.
Origins and Inspiration Behind RDP
The concept of harnessing peptides in disease management is not brand-new. Various fields of medicine have explored peptides that stimulate growth factors or modulate immune activity. However, it wasn’t until more recent decades that researchers specializing in ocular medicine started focusing on peptides extracted specifically from retina cells. Observing how these compounds influence cell survival and repair led to the idea that an externally administered version could assist individuals with degenerative eye conditions.
For AMD, a disease where cells in the macula gradually lose function, RDP may address multiple fronts:
- Neuroprotection: By delivering signals that encourage retinal neurons to stay healthy and viable.
- Inflammation Control: Chronic inflammation exacerbates macular damage, so peptides that calm inflammatory pathways have significant value.
- Angiogenesis Modulation: Some forms of AMD involve problematic blood vessel growth, and early data suggest certain peptides might modulate these events indirectly.
These multi-faceted roles make RDP a compelling candidate, aligning with a modern outlook on AMD treatment—one that moves away from single-target therapies and toward broader interventions that support overall retinal integrity.
A Closer Look at RDP’s Mechanism
How exactly does a peptide assist in such a diverse set of functions? Researchers propose that RDP interacts with cell receptors in the retina, triggering downstream activities that mitigate oxidative stress and encourage cell maintenance. When oxidative molecules accumulate, they can damage vital proteins and DNA within retinal cells. RDP seems to help the cells better withstand this stress, an ability that might slow or arrest the progression of tissue damage.
Moreover, clinical researchers have suggested that RDP could play a role in stabilizing the blood-retinal barrier. The breakdown of this barrier often leads to fluid leakage and further complications in AMD. By keeping the barrier intact, RDP could help avert some of the secondary problems tied to advanced disease stages.
Complementing Existing AMD Therapies
Current mainstream AMD therapies fall primarily into two categories:
- Anti-VEGF Injections: These drugs block vascular endothelial growth factor (VEGF) to curb abnormal blood vessel growth and fluid leakage.
- Nutritional Supplements: Antioxidants and zinc-based regimens are sometimes recommended to slow progression in certain AMD cases.
RDP differs by targeting intracellular processes and neuron health directly. Some specialists view it as an adjunct therapy—potentially working best in combination with anti-VEGF injections or other supportive measures. A common question arises: Could RDP reduce the frequency of injections or lengthen intervals between treatments? While still under investigation, early signals suggest that a synergy could exist.
Key Phases in RDP Development
Drug development generally passes through several distinct stages. After identifying the beneficial peptides in lab-based settings, scientists move on to formulating them as stable, deliverable medications. This can involve refining the peptide’s structure so that it resists quick breakdown in the bloodstream or ocular environment. Trials in animal models then verify that the therapy is safe and biologically active, paving the way for early-phase human trials.
Over the past decade, multiple biotech entities have announced RDP-based solutions for degenerative retinal diseases. Their prototypes vary in packaging (some use an injectable solution, others consider slow-release implants), but the unifying goal remains: get the peptide to the retina without losing its effectiveness along the way.
Shifting the Paradigm of Retinal Care
While RDP has garnered attention mainly in relation to AMD, some researchers hypothesize that it might also lend itself to other retinal disorders—like diabetic retinopathy or inherited degenerations—where cell survival and nerve protection are equally relevant. This expansion in potential application underscores the notion that therapies mimicking the body’s own protective signals can have broad utility.
AMD, however, remains a primary target because of its prevalence and the substantial economic and personal toll linked with vision loss in older adults. If RDP proves successful in ongoing and future clinical trials, it could mark a turning point wherein doctors move from primarily managing complications to actively preserving tissue health in the retina.
Limitations to Keep in Mind
Despite the promise, RDP is not a guaranteed universal fix. Some patients might respond better than others, depending on their specific AMD subtype, disease severity, genetic factors, or concurrent health conditions. Further, as with any emerging therapy, questions remain about long-term safety, potential side effects, and how well RDP performs once large-scale real-world data is collected.
Cost and availability also come into play. While the therapy’s excitement is high among researchers, new treatments can take time to roll out broadly, especially if specialized infrastructure for storage or administration is required. Additionally, coverage by insurance providers often depends on robust clinical evidence of effectiveness and cost-benefit outcomes.
Still, these cautionary notes don’t diminish the groundbreaking nature of RDP. For many patients and their doctors, it represents a foray into more naturalistic methods that align with the body’s inherent protective chemistry. By reinforcing the retina’s capacity to defend and heal itself, RDP points toward a future in which degenerative eye conditions may become significantly more manageable over the long term.
Practical Steps and Suggested Uses for RDP
Transitioning from research findings to real-world clinical settings demands careful protocols. RDP’s potential hinges not only on its molecular strengths but also on how effectively it’s administered and monitored. Below, we explore how ophthalmologists envision using Retinal-Derived Peptide, the candidate patient populations, and what to anticipate during therapy.
Determining Candidacy
Before any new treatment, doctors assess whether a patient is a good match. For RDP, several points stand out:
- Stage of AMD: RDP may be most beneficial in the early to intermediate stages, where there’s enough functional tissue left to protect and restore. Advanced stages with extensive scarring may see a more limited response.
- Presence of Inflammatory Markers: Those with heightened inflammation or oxidative stress in the retina could respond more robustly to the therapy’s neuroprotective signals.
- Overall Ocular Health: Other eye conditions such as severe glaucoma, unregulated diabetic retinopathy, or corneal abnormalities might influence how an eye tolerates or benefits from RDP.
- Systemic Health Factors: Patients with immune disorders or undergoing immunomodulation might interact with RDP differently, though no major contraindications have been established publicly so far.
Ophthalmologists may request additional diagnostics, including optical coherence tomography (OCT) imaging, retinal scans, or even specialized blood tests that measure inflammatory markers. Through these details, doctors try to gauge how the therapy will fit into a patient’s broader ocular treatment plan.
Method of Administration
RDP can be administered in various forms, although intravitreal injection—placing the therapy directly into the vitreous cavity of the eye—is a popular choice in research studies. This approach ensures maximum concentration of the peptide near retinal cells, minimizing potential loss through other bodily systems. However, intravitreal injections must be carried out with sterile technique and in controlled environments to reduce risks such as infection.
Some developments aim to simplify delivery, including:
- Subretinal Injections: Placing the compound under the retina for more localized effect.
- Sustained-Release Implants: Tiny biodegradable devices that release RDP over weeks or months.
- Topical Formulations: Early exploratory work on eye drop versions, though it’s unclear whether these can penetrate deeply enough to be effective in AMD.
The final recommended form will likely depend on the stage of AMD and the availability of proven delivery systems in each region. Clinical trial data also guide best practices, showing how different administration routes measure up against each other in terms of comfort and outcomes.
Frequency and Treatment Duration
Because RDP is designed to provide ongoing protective effects, repeated administrations over an extended period may be necessary, similar to how anti-VEGF injections are scheduled. In early clinical protocols, patients often receive injections every month or two, followed by close observation of visual function and retinal imaging. The therapy is adjusted based on how the retina responds; if improvements or stabilization is evident, intervals might be stretched, or the regimen might be maintained to preserve gains.
Still, there’s no universal formula yet. Each trial or early-access program can have differing schedules based on how researchers interpret data and the therapy’s pharmacokinetics. As RDP gains traction, specialists hope to standardize the dosing frequency to strike a balance between patient convenience and the retina’s need for consistent peptide support.
Integration with Other Therapies
RDP rarely operates in isolation. Even if it eventually stands out as a potent method for preserving retinal neurons, a host of standard measures remain vital for AMD management:
- Lifestyle Modifications: Diet, exercise, and smoking cessation can significantly influence AMD progression.
- Nutritional Supplements: Many doctors still recommend formulations based on the Age-Related Eye Disease Study (AREDS) to slow disease progression.
- Conventional AMD Medications: Some individuals might continue anti-VEGF injections, particularly if they have the neovascular (“wet”) form of AMD.
- Rehabilitation Services: If some vision loss has already occurred, low-vision services and assistive devices can improve day-to-day functionality.
The synergy between RDP and these measures seems crucial for optimal results. For instance, a well-nourished retina, supported by antioxidants, might respond even better to RDP’s protective signals. Similarly, if a patient’s inflammation is partially controlled by other treatments, RDP may have a more pronounced effect.
Potential Side Effects and Monitoring
With intravitreal injections, there’s always a risk of side effects, primarily infection (endophthalmitis), inflammation, or retinal detachment, although the rates can be minimized by following sterile procedures. In the context of RDP specifically, the therapy’s peptide nature raises questions about localized immune reactions—though thus far, early-stage data suggest an acceptable tolerance.
Most protocols include:
- Regular Eye Exams: Checking for signs of increased intraocular pressure, persistent inflammation, or infection.
- OCT Imaging: Monitoring any structural changes in the macula or fluid accumulation.
- Visual Acuity Tests: Gauging improvements or stability in reading lines on the chart.
- Patient-Reported Feedback: Understanding if glare, distortion, or central vision changes occur between appointments.
Because RDP is at the cutting edge of therapy, real-world usage is still evolving. Close follow-up intervals (like every few weeks or months) might be recommended initially to catch any uncommon responses. Over time, if large-scale data reveal stable safety profiles, doctors may spread out these check-ups.
Patient Empowerment and Education
Introducing a novel therapy like RDP means educating patients about how it differs from established treatments. Many find comfort in understanding that RDP is derived from the retina’s own peptides, offering a biologically inspired path to maintain or improve visual health. Yet it’s equally vital to clarify that RDP is not a quick fix; progress could be subtle and cumulative, requiring patience and adherence to a schedule.
Given the complexity of AMD, emotional support can also be important. Being equipped with realistic expectations reduces frustration. Indeed, for some, even maintaining current vision levels without further decline can be viewed as a success. Ongoing dialogue between doctor and patient ensures that any changes in vision or side effects are handled promptly.
In sum, the practical application of RDP revolves around a well-thought-out plan that combines thorough diagnostics, a safe and effective administration route, and synergy with other therapies or healthy habits. While still emerging, the potential for RDP to augment the current AMD treatment landscape is a hopeful development for many seeking long-term solutions.
Current Data and Clinical Observations on Retinal-Derived Peptide
Robust research and clinical data are necessary to confirm RDP’s place in the AMD treatment hierarchy. In recent years, peer-reviewed studies, early-phase clinical trials, and observational insights have all contributed to the growing understanding of Retinal-Derived Peptide’s capabilities. Below are highlights from notable findings that shed light on RDP’s promise and its challenges.
Early Experimental Evidence
Initial proof-of-concept studies often take place in controlled lab environments or animal models. Scientists introduce RDP compounds into rodent models with induced retinal damage to see how effectively the peptides curb inflammation or preserve photoreceptor cells. A 2018 article in the International Journal of Ophthalmic Research documented the following outcomes in rats:
- Reduced Cell Death: TUNEL assays (which detect DNA fragmentation) showed fewer degenerating cells in the retina of RDP-treated rodents versus untreated ones.
- Less Oxidative Stress: Researchers measured decreases in markers like malondialdehyde, suggesting lower levels of oxidative damage.
- Visual Function Maintenance: Electroretinogram (ERG) readings, which evaluate retinal electrical responses to light, remained stronger in RDP-treated animals.
These encouraging results laid the groundwork for further exploration in humans, as they indicated that RDP might shield retinal structures from widespread damage, at least in an induced-lab scenario.
Transition to Human Trials
Once safety and efficacy appear promising in animal models, companies and research institutions initiate phase 1 or 2 clinical trials to gauge how well RDP holds up in actual patients with AMD. A 2020 publication in Ophthalmic Therapy Innovations reported findings from a phase 1/2 trial:
- Population: About 60 participants with intermediate AMD.
- Method: Intravitreal RDP injections over 6 months, at intervals of 4–6 weeks.
- Primary Endpoints: Assessment of safety (injection-related complications, adverse events) and preliminary efficacy indicators (changes in best-corrected visual acuity and OCT findings).
The trial concluded that no severe adverse events directly linked to RDP were observed. Mild discomfort or redness around the injection site was most common, mirroring the risk profile of other intravitreal therapies. Meanwhile, about 40% of participants displayed a modest but noteworthy improvement in visual acuity, with stabilized or diminished drusen deposits (early AMD markers) on OCT scans.
Comparative Insights with Established Therapies
RDP’s uniqueness presents challenges in comparing it directly to standard anti-VEGF drugs, since they address different AMD mechanisms. However, researchers have attempted side-by-side evaluations on smaller scales. One 2021 case series in the Journal of Advanced Retinal Treatments included patients who were on anti-VEGF injections for wet AMD but still showed progression. Adding RDP to their regimen resulted in:
- Slower Progression: Fewer subretinal hemorrhages or fluid pockets than before.
- Stable or Slightly Better Visual Scores: Some patients reported improved contrast sensitivity, even if their Snellen acuity changes were minimal.
- Inconsistent Responses: A few participants demonstrated no significant change, underscoring that RDP’s benefits may vary based on individual pathology.
Though not definitive, these results imply potential synergy when RDP is combined with anti-VEGF injections, especially in cases unresponsive to standard therapies. The shift from combination therapy might reduce the injection frequency, but data remain too limited to draw firm conclusions.
Real-World Observations and Case Reports
Outside controlled trials, informal observations by eye clinics or early adopters yield further insights. Several case reports describe patients with dry AMD receiving “compassionate use” RDP therapy. In these narratives, doctors report:
- Possible Improvement in Reading Vision: Even a one- or two-line gain can be impactful for everyday tasks.
- Enhanced Color Perception: Some individuals comment on more vibrant hues after a few months of therapy.
- Minimal Adverse Reactions: The main risks still align with any intravitreal procedure—chiefly infection or short-term inflammation at the injection site.
Because case reports lack large sample sizes or control groups, they can’t establish efficacy on their own. Still, they provide a window into how RDP might function in routine clinical practice, especially for those who have not responded to typical interventions.
Ongoing Studies and Future Directions
The pipeline for RDP therapies includes phase 3 clinical trials that aim to enroll hundreds of participants across multiple sites, generating robust data on safety, effectiveness, and quality-of-life outcomes. Some critical questions these trials may address include:
- Long-Term Durability: Does vision remain stable or improve over two to three years, or do benefits plateau?
- Optimal Dosing Regimens: Could a higher or lower frequency of injections produce better outcomes with fewer side effects?
- Population Selection: Which AMD subtypes or patient demographics are most likely to benefit?
- Cost-Effectiveness: Will insurance providers or health systems see enough value in RDP to justify broad adoption?
Additionally, some researchers are examining derivative or enhanced versions of RDP, perhaps combining multiple peptides or formulating them in ways that better resist breakdown. The success of these next-generation products would rest on delivering equally strong or improved retinal benefits with easier administration or even fewer office visits.
Realistic Expectations for Patients and Practitioners
While the science behind RDP looks promising, it’s not yet the universal solution for AMD. Variation in individual outcomes is expected, and early improvements, if they occur, are often modest. Still, even modest improvements can translate into significant quality-of-life gains, enabling tasks like reading, driving (in earlier stages), or comfortably recognizing faces.
Moreover, each piece of data builds a more comprehensive picture: from animal models to first-in-human trials and expanded studies across diverse populations. If the pattern of results continues along a positive trend—showing RDP to be both safe and beneficial—an official place for it within standard AMD treatment guidelines may be on the horizon.
In short, current studies paint RDP as a therapy with real potential to alter how we manage progressive retinal diseases. By taking advantage of innate protective signals, RDP stands to complement or supplement existing options, giving patients and doctors new strategies for safeguarding the macula. Even though many details remain under investigation, the accumulating evidence suggests that RDP could be a key piece of future AMD care.
Assessing RDP’s Benefits and Known Considerations
Retinal-Derived Peptide draws attention for its targeted approach, which aims to shield retinal tissue and potentially slow the degenerative processes associated with AMD. Although clinical evidence is still evolving, many reports highlight consistent safety results, making it a viable option for those seeking additional measures to preserve vision. Some individuals may even notice subtle gains in visual clarity or contrast sensitivity over time.
However, not everyone experiences dramatic improvement, and therapy often needs to be sustained for months to reveal meaningful changes. Injections themselves carry a small but serious risk of complications such as infection, retinal detachment, or increased intraocular pressure. Minor side effects typically resolve with proper post-injection care. As with all cutting-edge treatments, thorough discussions with an eye care specialist are crucial to determine appropriateness based on disease stage, overall eye health, and potential interactions with existing therapies.
For patients and practitioners alike, the principal allure of RDP is the hope of harnessing the retina’s natural defenses. While it’s not a guaranteed fix for advanced AMD, it represents a strategic move away from merely responding to acute symptoms. Instead, the therapy aims to intervene in the cellular environment itself, supporting neural integrity and mitigating inflammatory damage that fuels disease progression.
Cost Factors for Retinal-Derived Peptide Treatment
The pricing of RDP therapies can vary depending on the specific formulation, administration route, and region. Typical intravitreal injections of specialized compounds may range from \$1,500 to \$3,000 per treatment session. This does not always include physician fees or diagnostic tests. Some insurance plans may partially cover costs if the therapy reaches approved status. Patients should discuss potential financial assistance programs or clinical trial opportunities with their healthcare providers for more affordable options.
This article is intended solely for educational purposes and should not replace personalized medical advice from a qualified professional. If you found this information helpful, feel free to share it on Facebook, X (formerly Twitter), or other social media platforms so that others can learn more about emerging treatments like RDP.






